Factors Influencing Condom Use for the Prevention of Pregnancy and HIV Infection among Teenagers In Kampangpeth Province, Thailand
Wongsawat P1*, Songthap A1, Pengcha P2, Hoyrat P2
1 Department of Community Health, Faculty of Public Health Naresuan University, Thailand.
2 Irrigation Hospital, Srinakarintarawirot Prasarnmitr, Thailand.
*Corresponding Author
Pramote Wongsawat,
Department of Community Health, Faculty of Public Health Naresuan University, Thailand.
Tel: +66-81-8581950
Fax: +66-55-967333
E-mail: moteww@gmail.com
Received: January 14, 2020; Accepted: January 30, 2020; Published: February 04, 2020
Citation: Wongsawat P, Songthap A, Pengcha P, Hoyrat P. Factors Influencing Condom Use for the Prevention of Pregnancy and HIV Infection among Teenagers In Kampangpeth Province, Thailand. Int J Chronic Dis Ther. 2020;6(1):98-101. doi: dx.doi.org/10.19070/2572-7613-2000020
Copyright: Wongsawat P© 2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Despite convenience, availability, accessibility and affordability of condoms, a significant proportion of adolescents worldwide engage in unprotected sexual activities, leading to rising rates of new HIV infections and pregnancy. This study was conducted to determine factors influencing condom use for the prevention of HIV infection and pregnancy among secondary school students in Kampangpeth Province. Across-sectional design was conducted between February and March 2019 to select 183 samples by stratified random sampling. Data were collected using a questionnaire and analyzed using mean, frequencies, percentage, and regression analysis. Factors influencing condom use included knowledge of sexual education [OR = 1.26 (95%CI: 1.04 – 1.52), p = 0.017], self-efficacy to prevent pregnancy and HIV [OR = 1.10 (95%CI: 1.01 – 1.20), p = 0.027], curiosity to try sex [OR = 1.17 (95%CI: 1.04 – 1.31), p = 0.011], time spent with a boy/girlfriend [OR = 1.09 (95%CI: 0.85 – 1.00), p = 0.049], consumption of sexual media [OR = 1.08 (95%CI: 0.99 – 1.17), p = 0.048], good family care [OR = 7.89 (95%CI: 1.07 – 58.11), p = 0.043]. being male [OR = 5.26 (95%CI: 0.07 – 0.71), p = 0.014], and living with parents [OR = 3.42 (95% CI: 1.15 – 10.19), p = 0.027]. This study concluded that based on the factors influencing condom use to protect against HIV infection and pregnancy in adolescents, sexual education in secondary schools should be encouraged to increase sexual knowledge and family ties between parents and adolescents especially girls should also be strengthened.
2.Introduction
3.Materials and Methods
3.1 Study Design and Subjects
3.2 The Study Tool
3.3 Data Collection and Analysis
3.4 Ethical Consideration
4.Results
4.1 Socio-demographic Characteristics
4.2 Factors influencing Condom Use
5.Discussion
6.Conclusion
7.Acknowledgements and Declaration
8.References
Keywords
Condom use; Adolescents; Secondary School; HIV, Teenage Pregnancy.
Introduction
The most commonly used method of modern contraception among adolescents is condom [1, 2]. Convenience, availability, accessibility and affordability [3] maybe a great extent to explain the preference of the youths over other methods. As opposed to oral pills [4], a condom is effective in the prevention of both infections and unplanned pregnancy. However, a significant proportion of adolescents worldwide engage in unprotected sexual activities [5]. Consequently, the impacts such as rising rates of new HIV infections and teenage pregnancy has been well elaborated among this age group.
HIV/AIDS is the world’s second leading cause of adolescent deaths and, regrettably, adolescent girls account for over twothirds of the global new HIV infections [6]. Thailand alongside Indonesia, Viet Nam, China, Myanmar, and India accounted for over 90% of people living with HIV in the entire region [7]. Additionally, approximately 21 million girls below 20 years get pregnant annually; almost half of that is unintended. Of these, no fewer than 12 million pregnancies result in birth, contributing nearly 11% of the global births [8, 9]. Not only is adolescent pregnancy a public health concern in Thailand, but also the increasing rates of repeat birth [10]. As reported by a population and social research, Thailand is at the leading role in Asia for unintended teenage pregnancies [11]. It was estimated that more than 10% of Thai adolescent girls get pregnant yearly [12].
The increasing rates of new HIV/STDs infections and teenage pregnancy have been attributed to the consistently falling prevalence of contraceptive use in recent years [13]. It revealed that barely 60% of adolescents and youths consistently use a condom during the last sex [14]. The aim of this study, therefore, was to determine factors influencing condom use for the prevention of HIV infection and pregnancy among secondary school students. The results of this study can be utilized to set up a program for the prevention of pregnancy and HIV infection in adolescents.
A cross-sectional study was carried out among secondary school students in Kampangpeth Province between February and March 2019. A sample of 183 was determined using the estimation sample proportion. The study employed a stratified random sampling technique for the selection of the subjects. Only students aged 16 through 19 years were included in this study.
A questionnaire was developed and validated prior to the data collection. It consisted of six parts; 1) socio-demographic characteristics, 2) condom use, 3) knowledge, 4) attitude, 5) perceived impact and 6) perceived self-efficacy. Both the content validity and the reliability of the questionnaire were evaluated. All questions with Item Objective Congruence (IOC) index of greater than 0.5 were metthe standard criteria of the validity test [15]. The multidimensional reliability tests yielded a Chronbach’s alpha coefficient of 0.76, 0.86, 0.71 and 0.88 for knowledge, attitude, perceived impact, and perceived self-efficacy, respectively.
Data were collected by self-administered questionnaire to the respondents andanalyzed usingthe Statistical Package for Social Sciencesprogram (SPSS®, version 20.0). Socio-demographic variables ofthe participants were analyzed using frequency (%) and mean (SD). A binary logistic regression was performed to determine factors influencing condom use. All analyses were performed at a 0.05 level of statistical significance.
The research was approved by Naresuan University Institutional Review Board (IRB). Informed consent forms were obtained from participants of legal age, while parents/guardians of participants below the legal age provided assent forms. Data were treated with strict confidentiality.
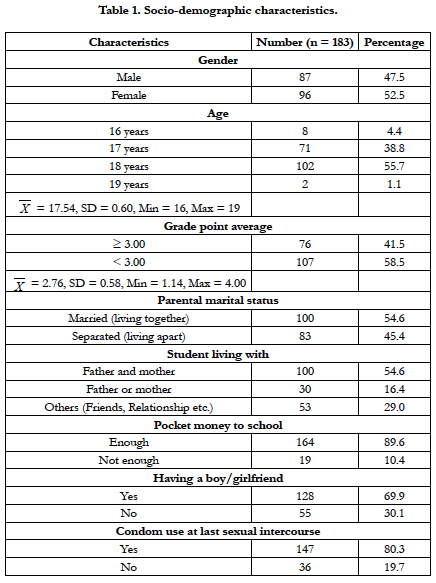
More than half of the students were females (52.5%) with a grade point average below 3.00 (58.5%). Approximately 95% were between the ages of 17 and 18 years (mean 17.54 ± 0.60). More than half of their parents were married (54.6%). While 54.6% of the students lived together with both parents, 16.4% lived with either parent and 29% lived with friends, relatives etc. The vast majority received enough pocket money (89.6%) More than twothirds (69.9%) were in a love relationship with approximately 80% reporting condom use during the most recent sexual experience (Table 1).
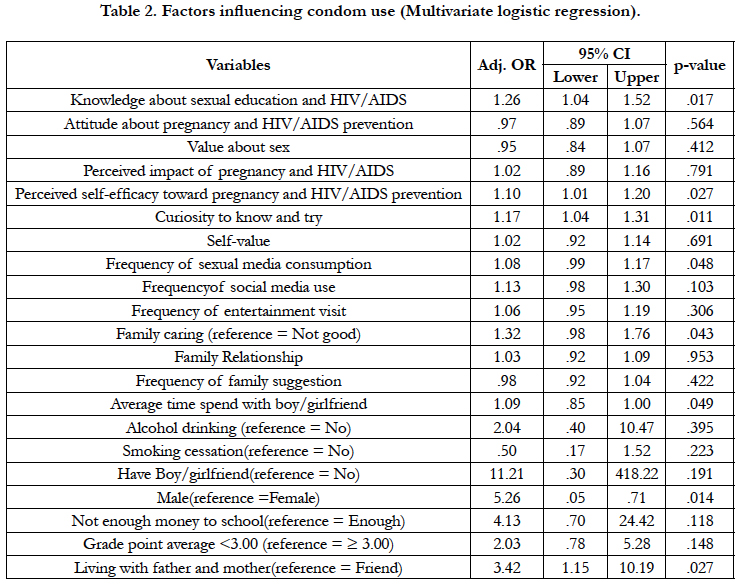
Factors from the multivariate analysis (Table 2.) were identified to be significantly associated with condom use. The results showed that an increase in knowledge by one score increases the probability of condom use 1.26 times [OR = 1.26 (95%CI: 1.04 – 1.52), p = 0.017]. An increase in self-efficacy to prevent pregnancy and HIV/AIDS by one score also increases the likelihood of condom use 1.10 times [OR = 1.10 (95%CI: 1.01-1.20), p = 0.027]. Additionally, probability of condom use increased by 1.17 times when students’ curiosity to know and try sex increases by one score [OR = 1.17 (95%CI: 1.04-1.31), p = 0.011]. One score increase in time spent with a boy/girlfriend increases the possibility of condom use by 1.09 [OR = 1.09 (95% CI: 0.85 – 1.00), p = 0.049]. Similarly, an increase in the consumption of sexual media by one score increases the tendency to use condom by 1.08 [OR = 1.08 (95% CI: 0.99 – 1.17), p = 0.048]. Furthermore, students who received good family care were 1.32 times as likely to use condom than adolescents from poor family care background [OR = 7.89 (95%CI: 1.07-58.11), p = 0.043]. Males were 5.26 times more likely to use condom than females [OR = 5.26 (95% CI: 0.07-0.71), p = 0.014]. Students who live with their parents were 3.42 times as likely to use condom as those who live with friends [OR = 3.42 (95%CI: 1.15-10.19), p = 0.027].
Discussion
Our research has found some interesting findings of condom use among secondary school adolescents. The results suggest that higher knowledge of sexual education increases the possibility of condom use. This was consistent with preceding evidence among Thai vocational school students that reported increased condom use among students with higher knowledge of HIV, STD and teenage pregnancy [16]. Undoubtedly, sufficient knowledge of sexual education and HIV/AID is an indispensable influencer of condom use for the prevention of HIV infection and pregnancy among teenagers. This might be because, when adolescents are adequately informed, they become more capable of making healthy sexual decisions such as the effective use of condom. Previous literature has reported varying levels of knowledge among adolescents ranging from low levels in the Democratic Republic of Congo (DRC) and Nigeria [17] to adequate levels in other parts of the world [18, 19]. Additionally, it has been observed that adolescent with high self-efficacy in preventing pregnancy and HIV infections were more likely to use condom. This was also consistent with a documented body of evidence which postulated that delays in sexual initiation and practice of safe sex are more likely among teenagers with high self-efficacy than those with low self-efficacy [20-22].
Teenagers who were curious to experience intercourse were more likely to use condom. This high condom use tendencies might have been as a result of their curiosity about sex which could lead them to explore more information about safe sex practice that may not have been available to incurious adolescents. Similarly, teenagers who frequently consumed sexual content from the media appeared more likely to use condom. Advancement in technology has led to the proliferation of many sexual media (electronic or print) outlets through which both harmful and beneficial content can be released to the public. It is possible that teenagers who exploit such media may have gained adequate knowledge concerning the importance and benefits of using a condom during sex. In addition, they may have been made more awareness of their vulnerability to HIV and unwanted pregnancy in unprotected sexual encounters.
While teenagers from a good caring family background were more likely to use condom than their counterparts from poorly caring families, those who live with their parents were equally more likely to use condom. Not surprisingly, it has been opined that living with both parents protects teenagers from sexual intercourse [23], possibly because of proper parental monitoring and guidance. Evidence has also suggested that family connectedness increases parent-adolescent communication regarding sex and delays teenage sexual onset [24]. This communication could develop adolescent negotiation skills in sexual decision making and empower them to practice safe sex.
As compared to female teenagers, males were exceedingly more likely to use condom. This aligns with piling evidence from both Asia and Africa [25-27]. This may not be unconnected to the fact that male condom is more readily accessible than female condoms and, on the part of female adolescents, skepticism to carry condoms may possibly further explain the observed difference. The more time spent with a boy/girlfriend, the higher the probability of using a condom. This could be valid because spending a considerable amount of time with a boy/girlfriend may lead to having sexual intercourse multiple times. This frequent sex may instill in their mind the fear of pregnancy, thus may opt to use condom to prevent it.
Conclusion
This study concluded that several factors can predict adolescent condom use to protect against HIV infection and pregnancy. Higher sexual education knowledge, perceived self-efficacy, curiosity to try, consumption of sexual media, family care, time spent with boy/girlfriend, being male and living with parents were the factors influencing condom use. Therefore, sexual education in secondary schools should be encouraged and family ties between parents and adolescents especially girls should be strengthened.
Acknowledgements and Declaration
The authors wish to acknowledge the contribution of school directors, teachers, and parents for their kind supports and assistance in coordinating the students at the time of data collection. The authors also declared no conflict of interests.
References
- Arunrat T, Gordon C, Banwell C, Utomo I D, Sleigh A. Sexual perceptions and practices of young people in Northern Thailand. J Youth Stud. 2011 May 1;14(3):315-339.Pubmed PMID: 22319025.
- Osaikhuwuomwan JA, Osemwenkha AP. Adolescents’ perspective regarding adolescent pregnancy, sexuality and contraception. Asian Pacific J Reprod. 2013 Mar 1;2(1):58-62.
- UNAIDS D. Joint United Nations Programme on HIV/AIDS (UNAIDS). Global and Regional data HIV/SIDA pag. 2017:12-6.
- Tololu AK, Belda SS, Worku BA, Deressa GN, Hassan RN, Gudeta TM. Premarital sexual practice and associated factors among robe TVET students at robe town, bale zone, Oromia region, southeast Ethiopia, 2016.. MOJ Public Heal. 2017;5(6):193-203.
- Musumari PM,Tangmunkongvorakul A, Srithanaviboonchai K, Yungyuankul S, Techasrivichien T, Suguimoto SP,et al. Prevalence and Correlates of HIV Testing among Young People Enrolled in Non-Formal Education Centers in Urban Chiang Mai, Thailand: A Cross-Sectional Study. PLoS One. 2016 Apr 12;11(4):e0153452. Pubmed PMID: 27070553.
- UNAIDS/UNICEF. All In to #EndAdolescentAIDS. [Last accessed on 2019 May 20] Available from: https://www.unaids.org/sites/default/files/media_ asset/20150217_ALL_IN_brochure.pdf.
- UNAIDS U. The gap report. Geneva. Switzerland. 2014 Jul 10.
- Darroch JE, Woog V, Bankole A, Ashford LS, Points K. Costs and benefits of meeting the contraceptive needs of adolescents. Guttmacher Institute. 2016 May.
- UNFPA. Girlhood, not motherhood preventing adolescent pregnancy.2015 [Last Accessed on 2019 Oct 17]. Available from: https://www.unfpa.org/sites/default/files/pub-pdf/Girlhood_not_motherhood_final_web.pdf. [Last Accessed on 2019 Oct 17].
- UNICEF. Situation Analysis Of Adolescent Pregnancy in Thailand. [Last accessed on 2019 Aug 20]. Available from: https://www.unicef.org/thailand/ media/1126/file/Situation%20Analysis%20of%20Adolescent%20Pregnancy%20in%20Thailand.pdf.
- Chinthakanan O, Rochat RW, Morakote N, Chaovisitseree S. The hidden problems of illegal abortions in Thailand. Chiang Mai Med J.2014;53(4):187-91.
- UNFPA. The State of Thailand's Population: Motherhood in Childhood, Facing the Challenge of Adolescent Pregnancy. [Last accessed on 2019 Oct 20]. Available from: https://thailand.unfpa.org/sites/default/files/pubpdf/State%20of%20Thailand%20Population%20report%202013-MotherhoodinChildhood_en.pdf.
- Latimore AD, Aramrattana A, Sherman SG, Galai N, Srirojn B, Thompson N, et al. Sexually transmitted infection risk behaviors in rural Thai adolescents and young adults: Support for gender- and age- specific interventions. Sex Transm Dis. 2013 Mar;40(3):216.
- Thai National AIDS Committee. Thailand AIDS response progress report. 2014. Nonthaburi: National AIDS Management Center Department of Disease Control Ministry of Public Health Thailand. 2015.
- Turner RC, Carlson L. Indexes of item-objective congruence for multidimensional items. Int J Test. 2003 Jun 1;3(2):163-71.
- Thato S, Charron‐Prochownik D, Dorn LD, Albrecht SA, Stone CA. Predictors of condom use among adolescent Thai vocational students. J Nurs Scholarsh. 2003 Jun;35(2):157-63.
- Gebremedhin SA, Wang Y, Tesfamariam EH. Predictors of HIV/AIDS knowledge and attitude among young women of Nigeria and Democratic Republic of Congo: cross-sectional study. J AIDS Clin Res. 2017;8(3):677.
- de Andrade V, Baloyi B. HIV/AIDS knowledge among adolescent sign-language users in South Africa. African J AIDS Res. 2010 Sep 28;9(3):307-13.
- Talwar P, Rahman MFBA. Assessment of HIV knowledge among university students using the HIV-KQ-18 scale: A cross-sectional study. South East Asia J Public Heal. 2015 Sep 13;5(1):33-8.
- Childs G, Moneyham L, Felton G. Correlates of Sexual Abstinence and Sexual Activity of Low-Income African American Adolescent Females. J Assoc Nurses AIDS Care. 2008 Nov 1;19(6):432-42.
- Guerra-Ordoñez JA, Benavides-Torres RA, Onofre-Rodríguez DJ, Márquez- Vega MA, Guerra-Rodríguez GM, Wall, KM. Self-efficacy and Coping as Correlates of Migrant Safe Sexual Behavior to Prevent HIV. J Assoc Nurses AIDS Care. 2017 Sep 1;28(5):761-9.
- Widman L, Golin CE, Grodensky CA, Suchindran C. Do Safer Sex Self- Efficacy, Attitudes toward Condoms, and HIV Transmission Risk Beliefs Differ among Men who have Sex with Men, Heterosexual Men, and Women Living with HIV?. AIDS Behav. 2013 Jun 1;17(5):1873-82.
- Abate G, Tessema F, Girma A. Premarital sexual practice and associated factors among preparatory school students in Jimma town, Oromia region, South West Ethiopia. J of Bio, Agri and Healthcare. 2016;6(15): 34–41.
- Khalaj F, Farahani A, Cleland J, Mehryar AHM. Associations between family factors and premarital heterosexual relationships among female college students in Tehran. Int Perspect Sex Reprod Health. 2011 Mar;37(1):30-9. Pubmed PMID: 21478086. https://www.ncbi.nlm.nih.gov/pubmed/21478086
- Odimegwu C, Adedini SA. Do Family Structure and Poverty Affect Sexual Risk Behaviors of Undergraduate Students in Nigeria? .Afr J Reprod Health. 2013 Dec;17(4):137-49. Pubmed PMID: 24558790.
- Pinyopornpanish K, Thanamee S, Jiraporncharoen W, Thaikla K, McDonald J, Aramrattana A, et al. Sexual health, risky sexual behavior and condom use among adolescents young adults and older adults in chiang mai, thailand: Findings from a population based survey. BMC Res Notes. 2017 Dec 4;10(1):682. Pubmed PMID: 29202883.
- Yi S, Te V, Pengpid S, Peltzer K. Social and behavioural factors associated with risky sexual behaviours among university students in nine asean countries: A multi-country cross-sectional study. SAHARA J. 2018 Dec;15(1):71-79. Pubmed PMID: 30058474.