Head Trauma using A Bladed Weapon
Diallo M1,2*, Kouitcheu R1, Alfalasi M1, Kaya JM1, Touta A1, Roche PH1
1 Neurosurgery Department, Hospital Nord Marseille, France.
2 Faculty of Medicine of Bamako, Mali.
*Corresponding Author
Diallo Moussa,
Neurosurgery Department, Hospital Nord Marseille, France.
E-mail: mdiallo5@gmail.com
Received: June 01, 2018; Accepted: June 27, 2018; Published: June 28, 2018
Citation: Diallo M, Kouitcheu R, Alfalasi M, Kaya JM, Touta A, Roche PH. Head Trauma using A Bladed Weapon. Int J Surg Res. 2018;5(4):111-114. doi: dx.doi.org/10.19070/2379-156X-1800024
Copyright: Diallo M© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Head trauma by a bladed weapon is an uncommon attack on the skull and its contents. Despite its rarity, it can have serious consequences for the victim. It sometimes follows a fight in cases of rape or aggression under the effect of narcotics. The authors report the case of a traumatic brain injury with a knife that occurred in a 40-year-old man in a context of acute alcoholism.
2.Introduction
3.Clinical Case
4.Discussion
5.Conclusion
6.References
Keywords
Head Trauma; Bladed Weapon; Knife; Acute Alcoholism.
Introduction
The head is not the first target in cases of aggression with a bladed weapon. As a result, brain injury with stab wounds is very rarely encountered by neurosurgeons. Despite this scarcity, they can have serious neurological consequences in victims, ranging from intracranial hypertension to death by lack of adequate care within a reasonable time frame. If there are basic principles to be followed for the assessment of a lesion after a head injury with the knife, the surgical approach would differ according to the case. The authors report the case of a head trauma with a knife in a 40-year-old man in a context of acute alcoholism. The scarcity of the case, the difficulties of the surgical approach and the presentation can serve to enrich the literature.
Clinical Case
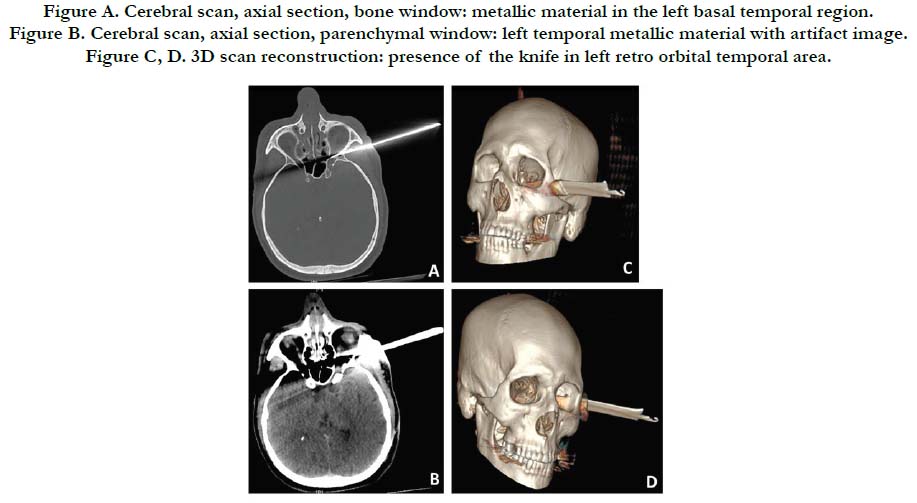
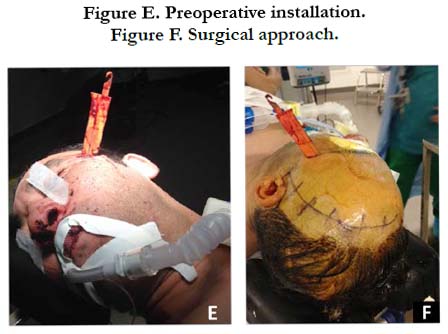
The patient is a 40-year-old male, a pizza delivery man, who was brought to the emergency department on February 17, 2018 by the firefighters for head trauma whose circumstances were not precise. The patient's previous medical history was not known. On clinical examination, there was a knife implanted in the left temporal region (Figure E). The patient had a Glasgow score of 14 with a strong alcohol odor, the pupils were symmetrical and reactive. There were no signs of cranial nerve involvement, no neurological deficit in all four limbs. The emergency brain scan revealed the presence of a knife blade passing through the left temporal muscles, the posterior wall of the lower part of the left orbital cone and ending in the left sphenoidal sinus. The artifacts of the knife did not make it possible to define the limits of the blade inside the skull (Figure A, B, C, D).The bone injury involved the sphenoid bone and the left orbital cone. The brain angio-scan had not been done due to abnormal renal function tests. The toxicological assessment found a blood alcohol level of 3.14 g. The surgical indication of a removal of the foreign body and wound debridement had been decided upon. The problem arose with regard to the choice of the approach and the risk of haemorrhage by vascular injury.
Figure A. Cerebral scan, axial section, bone window: metallic material in the left basal temporal region.
Figure B. Cerebral scan, axial section, parenchymal window: left temporal metallic material with artifact image.
Figure C, D. 3D scan reconstruction: presence of the knife in left retro orbital temporal area.
The surgical approach consisted of a left frontal pterional incision starting from the tragus. The challenge was to preserve the superficial temporal artery and the frontal branch of the left facial nerve. One of the first difficulties encountered was to retract the cutaneous flap because of the presence of the knife (Figure E, F). After completion of a pterionic flap, the entire temporal tip had been milled to find the intracranial end of the knife. The knife had not infiltrated the cerebral parenchyma, thus the removal of the knife implanted in the bone structures was decided. Debridement of the wound had been done followed by putting the bone flap in place and closure of the operative wound. A drain was also put in place.
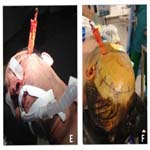
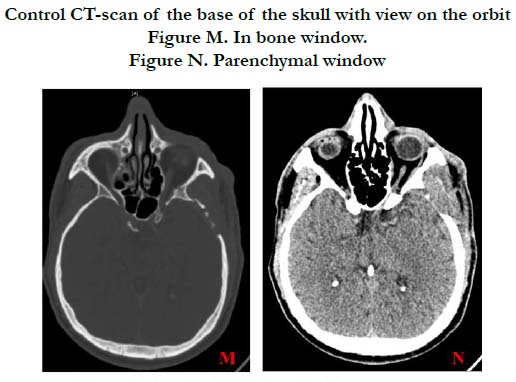
Postoperatively the patient had a Glasgow score of 15, no signs of neurological impairment. The cerebral CT scan revealed an extradural hematoma in the operative site (Figure G, H), and the cerebral angio scan did not find post-traumatic vascular lesions (Figure K, L). The post operative follow up was uneventful. The follow up cerebral CT scan showed a partial regression of the extradural hematoma and the absence of mass effect on the medial structures (Figure I, J). The 45-day control CT-scan of the skull base with orbit view was satisfactory (Figure M, N).
Figure G. Cerebral scan, axial section, parenchymal window: extradural hematoma, postoperative complication.
Figure H. Cerebral Scan, coronal Section, parenchymal Window: postoperative extradural hematoma.
Figure I, J. Cerebral follow upscan on day 2 post operative: Partial regression of the hematoma.
Figure K, L. Cerebral Angiography: Absence of Vascular Stroke on the Arteries of the Willis polygon.
Control CT-scan of the base of the skull with view on the orbit.
Figure M. In bone window.
Figure N. Parenchymal window
Discussion
Non-projectile penetrating head trauma represents only 0.4% of all head injuries [1]. The high mobility of the head means that it is not the first target in case of a knife attack. Cranial stab wounds are very rare and are seen exceptionally in Western countries. They are rarely responsible for death. A study conducted in Germany in 2002 found 13 cases of head injuries involving stab wounds out of which 4 deaths were documented over a 30-year period [2]. The frequency varies according to the country. The victims are overwhelmingly men. In general, the motives for aggression are domestic quarrels, conflicts between friends or colleagues or rarely cases of rape [2]. In the case of a brawl, the assailants are almost always under the influence of the alcoholic [1, 2] or suffering from a psychiatric disorder [3]. Our patient had an altered state of mind due to alcohol consumption.
Most stab wounds occur through the orbit or temporal region [4], where the bone is thin in thickness. The difference in bone thickness is not be the most important parameter for effective intracranial penetration in knife attacks [2]. Sufficient penetration of the knife into the skull requires a certain number of requirements; the sharp and rigid aspect of the blade, the force applied to the object. However, fixing the head would not be a decisive condition. For a successful penetration in the temporal region, it would be necessary to apply to the knife a force 5 times greater than that necessary to penetrate the skin; and for the parietal region a force 11 times greater [5]. Due to the mass of the knife being very low, the force necessary for the penetration of the blade in the skull would come essentially from the muscular power of the assailant. This suggests that most attackers are male.
Head trauma with brain injury by non-projectile objects can be classified into 2 categories. Those who penetrate the skull through the natural orifices (the eye, the nose) and therefore require a velocity of impact less than 100 meters per second (m/s) to reach the brain tissue; and those with higher velocities of sufficient impact to cross the skull's bony barrier, and cause damage to brain tissue [1].
If the diagnosis of the penetrating head trauma is made visually, a brain scan is essential to the assessment the injury. The angioscan looks for false aneurysms or vascular injuries. These two examinations are necessary before the surgery and can sometimes be difficult to interpret because of the artifacts related to the metallic blade of the knife. In our patient, because of an acute renal problem, the angio-scan was performed postoperatively after necessary corrections were made. Although the MRI works well in the diagnosis of brain lesions, it is not indicated in penetrating head injuries because of the risk of a ferromagnetic accident by the metal blade of the knife.
One of the problems in our patient was the surgical approach. An enlargement of the penetration hole of the knife would give the advantage of exploring the path to the tip of the blade and better manage a possible vascular wound. However, the risk of infection by the knife and its non-sterile blade, and the possible scar that the surgery could leave on the face of the patient have been factors to avoid this option. The frontal pterional approach would hide the surgical scar in the hair but does not allow to descend lower than the tragus, thus it remains limited. The difficulty of retracting the skin flap forward due to the presence of the knife was a great inconvenience.
Some authors prescribe antibiotic prophylaxis. This should be broad-spectrum antibiotic to cover gram-positive, gram-negative, and anaerobic bacteria because foreign bodies are thought to be highly septic [6].
Postoperative extradural hematoma was an unexpected complication. The presence of a drain could not prevent the occurrence of this complication. It had avoided anyway the installation of a larger collection that can compress the brain and cause intracranial hypertension. Clinical and radiological follow up had a good result.
Conclusion
Non-projectile penetrating head trauma is very rare. Each case is different in it’s management according to the location of the impact and the damage caused. The CT scan and the cerebral angio-scan are essential in the assessment of the lesions and are a tremendous help in choosing a surgical approach.
References
- de Holanda LF, Pereira BJ, Holanda RR, Neto JT, de Holanda CV, Giudicissi Filho M, et al. Neurosurgical management of nonmissile penetrating cranial lesions. World Neurosurg. 2016 Jun;90:420-429. doi: 10.1016/j. wneu.2016.03.015. PubMed PMID: 26987636.
- Bauer M, Patzelt D. Intracranial stab injuries: case report and case study. Forensic Sci Int. 2002 Sep 26;129(2):122-7. PubMed PMID: 12243881.
- Cemil B, Tun K, Yigenoglu O, Kaptanoglu E. Attempted suicide with screw penetration into the cranium. Ulus Travma Acil Cerrahi Derg. 2009 Nov;15(6):624-7. PubMed PMID: 20037886.
- DiMaio VJ, DiMaio D. Forensic pathology. CRC press; 2001 Jun 28.
- O’Callaghan PT, Jones MD, James DS, Leadbeatter S, Holt CA, Nokes LD. Dynamics of stab wounds: force required for penetration of various cadaveric human tissues. Forensic Sci Int. 1999 Oct 11;104(2-3):173-8. PubMed PMID: 10581723.
- Chibbaro S, Tacconi L. Orbito-cranial injuries caused by penetrating nonmissile foreign bodies. Experience with eighteen patients. Acta Neurochir (Wien). 2006 Sep;148(9):937-41; discussion 941-2. PubMed PMID: 16763734.