HIV Landscape in Bangladesh and a Comparison to the Global Context
Sultana T, Bin Manjur OH, Omar Md, Kabir Y*
Department of Biochemistry and Molecular Biology, University of Dhaka, Dhaka, Bangladesh.
*Corresponding Author
Yearul Kabir, Ph.D,
Professor, Department of Biochemistry and Molecular Biology,
University of Dhaka, Dhaka-1000, Bangladesh.
E-mail: ykabir@du.ac.bd words
Received: April 25, 2019; Accepted: May 28, 2019; Published: May 30, 2019
Citation: Sultana T, Bin Manjur OH, Omar Md, Kabir Y. HIV Landscape in Bangladesh and a Comparison to the Global Context. Int J AIDS Res. 2019;6(2):189-195. doi: dx.doi.org/10.19070/2379-1586-1900036
Copyright: Kabir Y© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The prevalence of HIV in Bangladesh is not alarming but the trend is. Every year the number of newly diagnosed infection is increasing along with the number of death due to AIDS and AIDS associated diseases. Prevalence has been found quite high among the injection drug users and the migrant workers. Particular populations, such as, homosexuals, transgender people are under-represented in the HIV studies and surveillances and these populations are the one most at risk. Due to the conservative society standard, these populations tend to stay underground. Most HIV infected people are unaware of their infections; those who are aware of their infection are not always under treatment. Rather they are outlawed from their families and often they lose their jobs. Initiatives have been taken globally to end HIV by 2030. Bangladesh has been lagged behind in this battle against HIV. Thus, strategies to work on HIV response with detailed action plans on prevention, treatment, service, research, and surveillance have been taken to meet the global challenge.
2.Abbreviations
3.Introduction
4.AIDS Demographics in Bangladesh
4.1 Transmission into Bangladesh
4.2 Prevalence of AIDS associated diseases in Bangladesh
4.3 Alarming recent trend of HIV in Bangladesh
4.4 Treatment facilities in Bangladesh
4.5 Risk Groups
4.6 Dealing with HIV/AIDS
4.7 Factors that contribute to HIV prevalence in Bangladesh
5.Changing the Scenario
5.1 Key Challenges
5.2 4th National Strategic Plan to End AIDS by 2030
6.Future Direction
7.References
Keywords
HIV; AIDS; Bangladesh; Opportunistic Infection (OI); People living with HIV (PLHIV); National Strategic Plan (NSP); Key Population (KP); Sex Workers; Risk Groups; Injection Drug Users (IDU); 90-90-90 Target.
Abbreviations
HIV: Human Immunodeficiency Virus; UNAIDS: United Nations Programme on HIV/AIDS; WHO: World Health Organization; OI: Opportunistic Infection; HAART: Highly Active Anti-Retroviral Therapy; MARPs: Most at Risk Populations; IDU: Injection Drug Users; NSP: National Strategic Plan; PLHIV: People Living with HIV.
Introduction
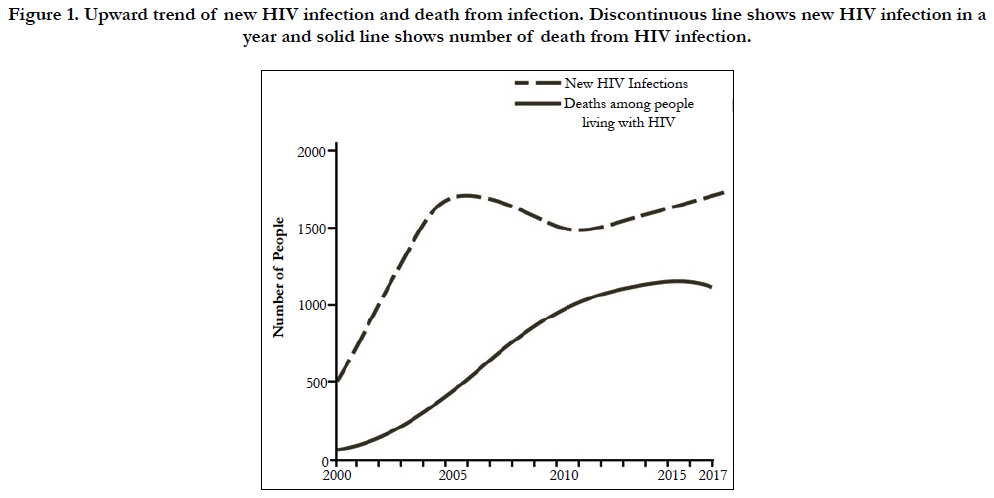
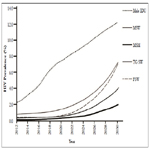
AIDS stands for Acquired Immuno Deficiency Syndrome. In this syndrome, immune system is prone to fail performing its activities due to a lentiviral infection by human immuno deficiency virus (HIV). Bangladesh is low prevalent but extremely vulnerable to HIV. While the conservative ambient contributed to keep the prevalence low, factors such as, poverty, population density, illiteracy, gender gap, frequent immigration, and high prevalence in the neighboring countries have made the country susceptible to HIV epidemic. Bangladesh has managed to keep the prevalence of AIDS less than 0.001% [1] although current trend is upward of both new HIV infections and mortality rate [2] (Figure 1). This may raise concern if the country does not have a proper HIV management set up in case of an outbreak. According to the United Nations Programme on HIV/AIDS (UNAIDS) data 2018, World Health Organization (WHO) has ranked AIDS as the 6th deadliest disease as it has caused around 1.78 million deaths contributing to the 3.1% of the total human death [2]. Young women are particularly at great risk for new HIV infections and AIDS is a leading cause of death among woman at reproductive age (15-49 years) [1]. According to the Global HIV & AIDS statistics by UNAIDS, there were 36.9 million people across the world living with AIDS of whom 9.4 million people were unaware of their infections and 1.8 million were children under 15 years in 2017 [3]. In comparison to the world status, the numbers of HIV infection in Bangladesh is relatively low although the number of people unaware of their infections or not under any treatment is relatively high. Bangladesh belongs to the south-east part of Asia. HIV prevalence varies widely in this region. India, Indonesia, Myanmar, Nepal, and Thailand account for more than 99% of HIV burden in the region while Bangladesh, Bhutan, Maldives, and Sri Lanka together represent less than 1% of all HIV infections [4]. To overcome the worldwide burden of HIV, UNAIDS made a 90-90-90 target according to which by the year 2020, 90% of the HIV infected people will know their HIV status, 90% of the HIV diagnosed people will receive antiretroviral therapy, and 90% of the people receiving antiretroviral therapy will have viral suppression [5]. To achieve this global goal, it is important that each country adopt strategies to reach their respective national goal. Among the neighboring countries, Thailand is supposed to achieve the target ahead of 2020 with its current action and strategies [4]. Unfortunately, it seems likely from the statistics of the last few years that Bangladesh will not reach the goal by 2020.
Figure 1. Upward trend of new HIV infection and death from infection. Discontinuous line shows new HIV infection in a year and solid line shows number of death from HIV infection.
AIDS Demographics in Bangladesh
Evidence strongly suggests that the first transmission from Simian immunodeficiency virus to HIV took place around 1920 in Kinshasa [6], a center for commerce in Congo attracting workers. The earliest proven case of HIV AIDS was found in 1969 in a patient from Kinshasa [7]. Development of the railway led to the initial spread and stride of AIDS. First HIV infection in Asia was detected in 1984 in Thailand. The first in India was found in 1986 when a number of female sex workers in Chennai were diagnosed with AIDS. The frequency of foreigners traveling in and out of India was high at that time. By 1987, AIDS was spread to eleven countries in Asia [8]. The first infection in Myanmar was diagnosed in 1988 and the next year in Bangladesh. Bangladesh shares borders with India and Myanmar and people including migrant workers frequently cross the borders which could be the possible route of HIV transmission into Bangladesh.
In primary HIV infection, only around 50% of infected individuals are symptomatic with mild to severe lymphadenopathy and fever. Depending on HIV subtypes, average endurance time after infection is 9 to 11 years, if untreated [9]. Major symptoms of AIDS include nausea, vomiting, diarrhea, rapid weight loss, chronic fatigue etc. Since the immune system is compromised, patients frequently suffer from opportunistic infections. Fairly common consequence of AIDS is relative progression of microbial infection. The most prominent infectious agents include Toxoplasma gondii, Candida sp., Aspergillus sp., Histoplasma capsulatum [10]. Tuberculosis remains globally the leading cause of death among people living with HIV (PLHIV) accounting for around one in three AIDS-related deaths [2]. Complications can also be viral, for example, cytomegalovirus plays a frequent role in developing neuropathy [11]. In a study conducted in 2014 on 293 HIV patients, tuberculosis (32%) was the most common presumptive opportunistic infection (OI) [12]. In 2016, 11.1% of the patients enrolled in HIV-care in Bangladesh was detected with tuberculosis [2]. Other OIs included esophageal candidiasis (9%), Pneumocystis jirovecii pneumonia (8%), histoplasmosis (7%), and malignancies (3.8%). Types of malignancies found in this study are Non-Hodgkin’s lymphoma, central nervous system tumors, Kaposi’s sarcoma, mediastinal sarcoma, cervical cancer, carcinoma of the tongue and adenocarcinoma of the colon. HIV related diseases were the primary reason for death in most patients, which could be avoided with earlier diagnosis of HIV and proper management of OIs.
Bangladesh showed to understand the threat of AIDS very early. The national AIDS committee was established in 1985, 4 years before the first HIV case was reported in the country [13]. Since the detection of the first HIV-positive person in 1989, the current HIV-statistics of Bangladesh stands with around 13,000 PLHIV of which 4,400 are women, only 2470 infected patients are on antiretroviral therapy, and 1100 died [2]. Less than 0.01% of the population is estimated to be HIV positive which categorizes Bangladesh to be a low HIV-prevalence country. Even in the high risk or key population, the percentage is near 1% [1]. This low rate of HIV can be attributed mostly to a conservative social structure. Polygamy, premarital sex, promiscuous life style, homosexuality is socially unacceptable. As 88.6% of the population is Muslim, males are circumcised mostly. Male circumcision has been found to reduce the risk of female to male transmission of HIV infection by 60% [14]. In 2016, newly identified HIV patients were geographically distributed as following: Dhaka (37.5%), Chittagong (23.5%), Khulna (17.0%) and Sylhet divisions (14.0%) [15]. However, in contrast to the all previous statistics, lately there has been a 10% increase in the number of new infections each year [2]. It was around 1700 new infections in 2017 in comparison to 1600 new infections in 2016, 2015 and 1500 in 2014, 2013, 2012 (Figure 1). In a similar fashion, AIDS related deaths have been doubled in the last 15 years with a 20% increase since 2010 [2].
Complete cure of HIV has not been possible but antiretroviral drugs can reduce the viral load. Opportunistic infections are treated separately as per infection. Treatment in Bangladesh was facilitated primarily by the international NGOs until 2011. Later government started to collaborate with the NGOs in a drug supply program. In 2017, Bangladesh government started antiretroviral therapy centers in 6 institutes across the country [16]. When a single class of drug is used for therapy, HIV often takes over the drug due to their high mutation rate. Thus, after the initial failures, a new strategy of Highly Active Anti-Retroviral Therapy (HAART) was taken in which a combination of different drugs from different drug classes is used targeting different stages of viral life cycle. Drug classes that are currently used include Nucleoside Reverse Transcriptase Inhibitors, Non-Nucleoside Reverse Transcriptase Inhibitors, CCR5 blockers, protease inhibitors, and integrase inhibitors. HAART is costly and acts as a major limiting factor in prolong dose. Currently a good number of different drug regimens in different drug concentrations and formulations are available in the antiretroviral therapy centers of Bangladesh: 1) lamivudine + zidovudine + nevirapine, 2) lamivudine + zidovudine, 3) Efavirenz, 4) Lamivodine, 5) Tenofovir, 6) Tab Lopinavir/Ritonavir, 7) Tenofovir + Emitricitabine + Efavirenz, 8) Tab Atanavir/Ritonavir, 9) Tenofovir + Emtricitabine, 10) Batcaver, 11) Nelfinavir, and 12) Abacavir + Lamivodine. Planning is required to cover the high cost of therapy and to maintain the regularity among the AIDS patients. The procedure for providing drugs to patients varies from country to country. In India, the price of some antiretrovirals has been reduced by 37 - 53% over the last 10 years [17]. The SriLankan government provides drugs to patients free of costs through state protocol [18]. Likewise, Bangladesh has lately taken the initiatives to assure drug supply with minimum cost, more funding for HAART, and prevention of inequalities in treatment accessibility at the community level.
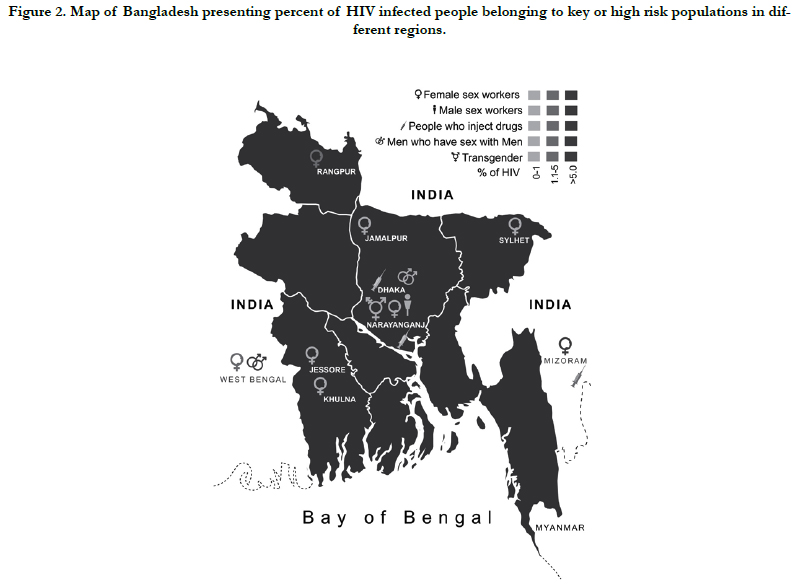
Compared to the general HIV prevalence of 0.1%, Most at Risk Populations (MARPs) the occurrence can rise as high as 2.7% [19]. HIV risk arises primarily from unprotected sex and sharing of used needles leading to higher occurrences among injection drug users (IDU), migrant workers, transportation workers, sex workers, and homosexual males (Figure 2).
Figure 2. Map of Bangladesh presenting percent of HIV infected people belonging to key or high risk populations in different regions.
During the seventh round of serological surveillance conducted between January and June 2006, 10,368 people were sampled and the highest HIV rate was recorded in male IDUs from the capital city Dhaka (7%) [20]. In Dhaka, 10.5% of the HIV-positive IDUs were localized in one particular neighborhood. In the 2007/08 survey, the overall prevalence of HIV was found 1.2% among the IDUs with a concentrated epidemic among the male IDUs in Dhaka. The prevalence of HIV in this cluster increased from 4% in 2002 to 7% in 2007/08 and later declined slightly to 5.3%in 2010 [21]. Serological surveillance in 2011 showed that HIV prevalence among all the key populations remained below 1% with the only exception of IDU population. Stigma linked with IDUs has a negative impact on the social recognition of users and job facilities available to them, inhibiting their rehabilitation into Bangladeshi society [22]. Since female IDU are marginalized and stigmatized; they are more vulnerable to HIV and very little is known about the female IDUs in Bangladesh. It is unfortunate that intervention programs hardly reach out to female IDUs.
The National AIDS/STD program report of 2006 stated that approximately 67% of identified HIV positive cases in the country were returnee migrant workers and their spouses. Labor migration is an increasing source of foreign exchange earnings for Bangladesh. 4% of the country’s GDP comes from remittances according to the International Organization for Migration (2006). Over 5 million Bangladeshis are employed abroad. According to a study on 259 HIV infected patients in 2014, 77% of the HIV positive adults had a history of migrant work or was the spouse of a migrant worker [12]. Rural residence, employment in the Middle East, and longer duration of migrant work, each associated independently to testing HIV positive [23]. Considering the shared border with India, an HIVprevalent country, cross-border movements impose a great threat of HIV [24]. Several agencies working on HIV/AIDS prevention in Bangladesh have shortlisted migrant workers as well as workers from the transport sector, such as dock-workers, truck-drivers and rickshaw-pullers as vulnerable to AIDS [20].
Except for some small clusters of sex workers, the prevalence of HIV has remained <1% for female sex workers [20]. Several reports in Bangladesh has found elevated levels of sexually transmitted disease among commercial sex workers to be as high as 28% for gonorrhea and 57% for syphilis [25, 26]. FSWs are extremely vulnerable to HIV transmission and works as media of transmission as well. It was found in a recent study in Daulatdia where the largest brothel of Bangladesh that 47% of the clients was suggested to use condom during last sexual intercourse and only 21% did so. Alarmingly, only 3.7% of the female sex workers consistently used condoms [27].
Male sex worker and homosexuals have been included in surveillance since 2000-01 by the national HIV and syphilis surveillance. Despite the risky behaviors, HIV rate has remained <1% for both transgender people and male sex workers [20]. The male homosexuals are a hidden population in Bangladesh. A large proportion of male homosexuals had female sex partners or was married. A qualitative study revealed that society pushed these male homosexuals to marriage and fatherhood with women. Thus their female partners are as well at risk of HIV [28]. No study is known to be conducted yet on the female homosexual population of Bangladesh. Transgender people are not usually interested in public exposure for having their ‘inappropriate’ gender and behavioral roles which are judged against by the hetero-dimensional society of Bangladesh. Homosexuality is criminalized under the section 377 of the penal code which works as an effective barrier to HIV/AIDS [29]. However, this type of social attitudes hamper both transgender and homosexual people from using condoms, accessing treatment and counseling for STIs, and adequate testing services [30].
HIV-related stigma negatively affects HIV care, particularly in racial, religious and ethnic minority groups [31]. PLHIV suffer from mental and social health problems, including chronic stress, anxiety and depression [32]. They also feel negative self-worth, social rejection, and apparent interpersonal humility associated with sharp level of distress [33]. As a sexually promiscuous disease, patients and their associates face ostracism and frequent isolation from society as well as family. The robust religious beliefs and social discrimination hinder disease control as people avoid voluntary testing and disclosure. 34.6% of the infected women aged 15-49 years reported discriminatory behaviors towards them while 5% of patients were denied health service [2]. Stigma, prejudice and discrimination are extended to people associated with HIV-positive patients such as health care providers, hospital staffs, friends, and family. Similar to the low-economy countries in sub-Saharan Africa and south Asia, views of health care providers toward the HIV-positive people in Bangladesh is not much different from the mass people [34]. 5% of the Bangladeshi patients reported that care providers violated the confidentiality of patient’s HIV status without their consent [2]. Sometimes, the care providers are strongly discriminated as well and forced to quit their job [34]. As AIDS is often connected with sexual intercourses, the allegation of stigmatization is usually very dominant. Many people have constant belief that only immoral people will get HIV infections. Although raising awareness is essential to fight with HIV, conversation on HIV/AIDS is infrequent in Bangladesh, even in educational arrangements due to cultural taboos [35].
Deep rooted socio-economic constraints of the country, such as, illiteracy, poor knowledge on reproductive health due to the stigmatization of sex, gender inequality, and banishing of people with unusual sexuality, contribute to the spread of HIV. People belonging to low socio-economic status are more vulnerable to both HIV infections and post-infection discrimination. Health programs often do not get in touch with the poorest. A study showed that the richest male group was twice as informed about AIDS-prevention procedures in comparison to the poorest [36]. High number of HIV positive individuals affects the economic state. Majority of the patients in Bangladesh are unemployed or subject to lose their jobs as they face exclusion at working areas and in community life. Unemployed males from rural areas migrate to middle-east and work as labor. These young singles with little or no education are at high risk of unprotected sex with low cost sex workers or other males [36].
Education through media, particularly TV plays a leading role to raise awareness [23]. The inclusion of a book chapter on AIDS in text books from grade 6 to grade 12 has greatly increased the knowledge and awareness of AIDS among students [37]. But intercourse being a taboo in Bangladeshi communities made the introduction of sex education to the national curriculum very challenging. Women are particularly left behind in knowledge about HIV/AIDS. Only 16% of girls aged between 15 and 24 have a comprehensive knowledge of HIV in Bangladesh [38]. Bangladesh Demography and Health Survey conducted in 1999- 2000 reported that the odds of awareness among higher educated women and men were 4.69 and 77.73 times of no educated women and men respectively. In addition, both women and men those who regularly watch TV were 8.6 times more likely to be aware about AIDS compared to those who never watch TV [39]. Given the inferior socio-economic status in patriarchal society, women have less access to education, employment opportunities, health care including opportunities for HIV tests, counseling and medical care. Overall, women’s knowledge about HIV/AIDS has been decreasing over the years [40]. Studies have shown that secondary-higher educated women are 6.6 times more likely to have HIV/AIDS knowledge compared to the uneducated one. A rural-urban gap is noticed in women’s knowledge about HIV/ AIDS. Age, region, religion, socio-economic status, education have significant effects on women’s knowledge about HIV/AIDS [40].
Changing the Scenario
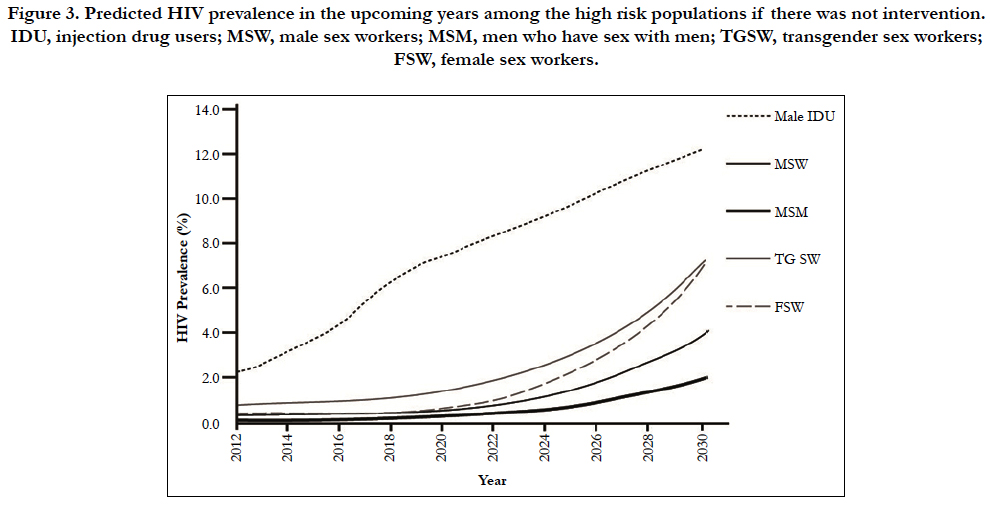
A 90-90-90 target by 2020 was set by the UNAIDS (see introduction). The world status stands as following in 2017, 75% people living with HIV knew their status, among them 79% were accessing treatment and among them 81% were virally suppressed [2]. Altogether, less than half of all PLHIV (47%) were virally suppressed [2]. The values estimated in Bangladesh stands way far from the world and the south Asian status. In 2017, 35% of the HIV-infected people knew their infection status and of them only 53% were on antiretroviral therapy (17% of total infected patients) in Bangladesh which is much less than the neighboring countries, such as, India, Nepal, and Thailand. If the current trend continues, the number of infected people belonging to each key population will increase at least twice or more times (Figure 3) [41]. However, the global target status is not fulfilling similar to the one of Bangladesh [15]. The global commitments have thus been expanded and included regional targets to globally ‘End HIV by 2030’. Keeping the challenges and progresses under consideration, Bangladesh has developed the 4th National Strategic Plan (NSP) for HIV and AIDS Response to act in the year of 2018-2022 with an aim to achieve both the global targets on ending AIDS by 2030 and the treatment target of ’90-90-90’ by 2020 [41].
Figure 3. Predicted HIV prevalence in the upcoming years among the high risk populations if there was not intervention. IDU, injection drug users; MSW, male sex workers; MSM, men who have sex with men; TGSW, transgender sex workers; FSW, female sex workers.
Policy and legal issues stand at the top of the challenge list to overcome AIDS. While there is a number of dedicated functional bodies, advocacy to integrate services from relevant bodies is not effective and adequate yet. Decriminalization of sex work is essential so that workers could be open to condom usage and regular diagnosis. Carrying educational material for HIV prevention may also be a punishable act under the current law [27]. Laws that hinder effective HIV responses impede key population’s access to justice and demands attention. Other challenges include raising awareness, access to prevention, diagnosis, treatment, counseling, and care for HIV by the huge number of key and general population. Since there is a growing risk of HIV in the key populations, enforcement of emergency response protocol is highly demanding.
The action and strategies of 4th NSP 2018-2022 are based on 4 objectives, the first focuses primarily on HIV prevention, second on treatment and services, third on the national response to HIV, and the fourth on research and surveillance for evidence based response.
The first objective was set to prevent new HIV infections by adopting strategies to increase timely case detection, minimizing STI, reducing risk behavior among key populations through intervention. Acts under this objective simultaneously focus on increasing program coverage, provision of services for risk populations and vulnerable groups, raising awareness, and strengthening reproductive health preventing sexually transmitted infections and opportunistic infections of HIV. Fast track approaches have been taken to actualize each of the strategies. 23 of the 64 districts have been prioritized to increase service coverage based on the frequency of key populations and PLHIV. Target setting in both the priority and regular districts is expected to reduce new infections to less than 300 a year by 2020. Provision will be revised to serve the most at risk adolescence population which occupies 13% of the key populations. Strengthened referral system by the caregivers and community involvement for increased access to reproductive health and HIV prevention are approaches underway. Up to 90% service coverage is expected in the 23 priority districts where high impact is needed. By 2022, HIV prevalence among key population is expected to be reduced to <1% for both male and female sex workers, <5% for transgender people, <10% for male IDUs (<40% in Dhaka district), and <5% for female IDUs (<15 in Dhaka district). One crucial target is to provide care and support to 90% of infected people.
The second objective was set to provide universal access to treatment, care and support services to the PLHIV. This is being done by combined approach of government and private sectors through strategies such as early detection and treatment to reduce mortality and morbidity among PLHIV, ensure capacity of service providers, accessible integrated testing, counseling and treatment service across the country. Earlier diagnosis of HIV can extend life expectancy up to 4.5 years [42]. One of the targets under this objective is to increase number of antiretroviral centers from 10 (in 2015-16) to 30 in 2022. Approaches have been taken to update policies and guidelines for treatment and management, provide comprehensive service including psychological support, social and legal support, peer support, financial support etc. Extended care arrangements for people who are ill and support for affected children will be accelerated.
The third objective is concerned about the strong coordination and management capacity of HIV-response bodies at different levels to ensure an effective national multi-sector HIV/AIDS response. Strategies have been adopted such as better structure and functionality of the National AIDS Committee, National AIDS/ STD Control Programme. Coordination between ministries, as well as health and community systems is emphasized to guide the national HIV response. 16 ministries and departments with HIV activities are targeted to set collaboration by 2022.
The fourth and last objective of the NSP program is concerned about monitoring, evaluation, and strategic information. Decisions will be made by finding evidence, their analysis and dissemination. Approaches have been taken to conduct serological and behavioral surveillances, assessments, case reporting, resistance monitoring etc. Response to HIV will be based on these results. It has been targeted to conduct 2 serological and 1 behavioral surveys of key populations in 2022.
Future Direction
AIDS is not only a health concern; it is a socio-economic challenge demanding an integrated management. Bangladesh has a large population with a conservative society. Because of these two contrasting characteristics, Bangladesh can be regarded as an appealing target for HIV with strong resistance. The current facilities are inadequate to prevent the uprising trend of HIV infection. If the country will be able to end AIDS by 2030 will largely depend on the success rate of the national strategic plan.
References
- UNAIDS. UNAIDS Data 2017. 2017:1-248.
- UNAIDS. UNAIDS Data 2018. 2018:1-376.
- UNAIDS. Fact sheet - WORLD AIDS DAY 2018. 2017:6.
- World Health Organization. Fast tracking the HIV response in the South-East Asia Region. WHO Libr Cat data. 2016.
- UNAIDS. 90-90-90 An ambitious treatment target to help end the AIDS epidemic. 2014.
- Faria NR, Rambaut A, Suchard MA, Baele G, Bedford T, Ward MJ, et al. The early spread and epidemic ignition of HIV-1 in human populations. Science. 2014 Oct 3;346(6205):56-61. doi: 10.1126/science.1256739. PubMed PMID: 25278604.
- Zhu T, Korber BT, Nahmias AJ, Hooper E, Sharp PM, Ho DD. An African HIV-1 sequence from 1959 and implications for the origin of the epidemic. Nature. 1998 Feb 5;391(6667):594-7. PubMed PMID: 9468138.
- Moss WJ, Clements CJ, Halsey NA. Immunization of children at risk of infection with human immunodeficiency virus. Bull World Health Organ. 2003;81(1):61-70. PubMed PMID: 12640478.
- UNAIDS/WHO. AIDS Epidemic Update. 2007:1.
- Britton CB, Miller JR. Neurologic complications in acquired immunodeficiency syndrome (AIDS). Neurol Clin. 1984 May;2(2):315-39. PubMed PMID: 6503940.
- Anders KH, Guerra WF, Tomiyasu U, Verity MA, Vinters HV. The neuropathology of AIDS. UCLA experience and review. Am J Pathol. 1986 Sep;124(3):537-58. PubMed PMID: 2876640.
- Shahrin L, Leung DT, Matin N, Pervez MM, Azim T, Bardhan PK, et al. Characteristics and predictors of death among hospitalized HIV-infected patients in a low HIV prevalence country: Bangladesh. PLoS One. 2014 Dec 8;9(12):e113095. doi: 10.1371/journal.pone.0113095. PubMed PMID: 25485634.
- Government of the People's Republic of Bangladesh. 3rd National Strategic Plan for HIV and AIDS Response 2011-2015. 2015.
- Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005 Nov;2(11):e298. PubMed PMID: 16231970.
- UNAIDS. Global AIDS Response Progress Report (GARPR). Annual Progress Report Bangladesh. 2015:38.
- Ahasan HN, Hossain HT, Reza IB. Current Status of Antiretroviral Therapy (ART) for Acquired Immunodeficiency Syndrome (AIDS) in Bangladesh. J Bangladesh Coll Physicians Surg. 2018 Jun 17;36(3):118-22.
- Giuliano M, Vella S. Inequalities in health: access to treatment for HIV/AIDS. Ann Ist Super Sanita. 2007;43(4):313-6. PubMed PMID: 18209264.
- R Rodrigo C, Rajapakse S. Current status of HIV/AIDS in South Asia. J Glob Infect Dis. 2009 Jul;1(2):93-101. doi: 10.4103/0974-777X.56249. PubMed PMID: 20300398.
- Chatterjee S, Kaur N, Sultana MM, Sultana T, Wagle S, Wagle S, Samuels F. Stories of Harassment, Violence and Discrimination: Migrant Experiences between India, Nepal and Bangladesh. 2012 Jan.
- Azim T, Rahman M, Alam MS, Chowdhury IA, Khan R, Reza M. Bangladesh moves from being a low-prevalence nation for HIV to one with a concentrated epidemic in injecting drug users. Int J STD AIDS. 2008 May;19(5):327-31. doi: 10.1258/ijsa.2007.007269. PubMed PMID: 18482963.
- Reddy A, Hoque MM, Kelly R. HIV transmission in Bangladesh: an analysis of IDU programme coverage. Int J Drug Policy. 2008 Apr;19 Suppl 1:S37- 46. doi: 10.1016/j.drugpo.2007.11.015. PubMed PMID: 18207724.
- Knight VC. Drug users at risk to HIV. Documenting our experience 2000-2005. Report. Dhaka: CARE Bangladesh; 2006.
- Urmi AZ, Leung DT, Wilkinson V, Miah MA, Rahman M, Azim T. Profile of an HIV testing and counseling unit in Bangladesh: majority of new diagnoses among returning migrant workers and spouses. PLoS One. 2015 Oct 29;10(10):e0141483. doi: 10.1371/journal.pone.0141483. PubMed PMID: 26513357.
- Datta P, Sadhu S, Bhattacharya NB, Majumdar KP. Demographic Effects of Forced Illegal Migration from Bangladesh to West Bengal: A Qualitative Study. Dialogue. 2008 Oct;10(2).
- Sarkar S, Islam N, Durandin F, Siddiqui N, Panda S, Jana S, et al. Low HIV and high STD among commercial sex workers in a brothel in Bangladesh: scope for prevention of larger epidemic. Int J STD AIDS. 1998 Jan;9(1):45-7. PubMed PMID: 9518015.
- Azim T, Islam MN, Bogaerts J, Mian MA, Sarker MS, Fattah KR, et al. Prevalence of HIV and syphilis among high-risk groups in Bangladesh. AIDS. 2000 Jan 28;14(2):210-1. PubMed PMID: 10708297.
- Hosain GM, Chatterjee N. Beliefs, sexual behaviours and preventive practices with respect to HIV/AIDS among commercial sex workers in Daulatdia, Bangladesh. Public Health. 2005 May;119(5):371-81. PubMed PMID: 15780324.
- Khan SI, Hudson‐Rodd N, Saggers S, Bhuiya A. Men who have sex with men's sexual relations with women in Bangladesh. Cult Health Sex. 2005 Mar;7(2):159-69. PubMed PMID: 16864195.
- Cassese A, Acquaviva G, Fan M, Whiting A. International criminal law: cases and commentary. Oxford University Press; 2011 Feb 24.
- Ahmed S. Social justice and the human rights of MSM in Bangladesh. Human rights in Bangladesh. 2003:235-45.
- Herek GM. AIDS and stigma. Am Behav Sci. 1999 Apr;42(7):1106-16.
- Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry. 2001 May;158(5):725-30. PubMed PMID: 11329393.
- Griffin KW, Rabkin JG. Psychological distress in people with HIV/AIDS: Prevalence rates and methodological issues. AIDS Behav. 1997 Mar 1;1(1):29-42.
- Ahsan Ullah AK. HIV/AIDS-related stigma and discrimination: A study of health care providers in Bangladesh. J Int Assoc Physicians AIDS Care (Chic). 2011 Mar-Apr;10(2):97-104. doi: 10.1177/1545109710381926. PubMed PMID: 21278365.
- Haider M, Ahmed SN, Jaha NK. Bangladesh HIV/AIDS communication challenges and strategies. Bangladesh Med Res Counc Bull. 2008 Aug;34(2):54-61. PubMed PMID: 19119540.
- Khosla N. HIV/AIDS interventions in Bangladesh: what can application of a social exclusion framework tell us?. J Health Popul Nutr. 2009 Aug;27(4):587-97. PubMed PMID: 19761091.
- Sarma H, Islam MA, Khan JR, Chowdhury KI, Gazi R. Impact of teachers training on HIV/AIDS education program among secondary school students in Bangladesh: A cross-sectional survey. PLoS One. 2017 Jul 24;12(7):e0181627. doi: 10.1371/journal.pone.0181627. PubMed PMID: 28742103.
- UNICEF. Children and AIDS Third Stocktaking Report, 2008. 2008.
- Rahman MS, Rahman ML. Media and education play a tremendous role in mounting AIDS awareness among married couples in Bangladesh. AIDS Res Ther. 2007 May 12;4:10. PubMed PMID: 17498310.
- Sheikh MT, Uddin MN, Khan JR. A comprehensive analysis of trends and determinants of HIV/AIDS knowledge among the Bangladeshi women based on Bangladesh Demographic and Health Surveys, 2007–2014. Arch Public Health. 2017 Sep 28;75:59. doi: 10.1186/s13690-017-0228-2. PubMed PMID: 28975026.
- Ministry of Health and Family Welfare, Bangladesh. 4thNational Strategic Plan For HIV and AIDS Response 2018-2022. 2016.
- Nakagawa F, Lodwick RK, Smith CJ, Smith R, Cambiano V, Lundgren JD, et al. Projected life expectancy of people with HIV according to timing of diagnosis. AIDS. 2012 Jan 28;26(3):335-43. doi: 10.1097/QAD.0b013e32834dcec9. PubMed PMID: 22089374.