Male-Female Differences in Sexual Behaviors and HIV Sero Prevalence among Workers in Socializing Places: Results from PLACE Survey, Uganda
Babirye S1*, Atuyambe L2, Kasasa S3, Ssendagire S1, Nattimba M4, Ssengooba F1
1 Department of Health Policy Planning and Management, Makerere University School of Public Health, Kampala, Uganda.
2 Department of Community Health and Behavioural Sciences, Makerere University School of Public Health, Kampala, Uganda.
3 Department of Epidemiology and Biostatistics, Makerere University School of Public Health, Kampala, Uganda.
4 One Health East and Central Africa, Uganda/Makerere University School of Public Health, Kampala, Uganda.
*Corresponding Author
Susan Babirye
Department of Health Policy Planning and Management,
Makerere University School of Public Health, P.O Box 7072 Kampala, Uganda.
E-mail: babiryes2004@gmail.com
Received: May 25, 2018; Accepted: June 23, 2018; Published: June 26, 2018
Citation: Babirye S, Atuyambe L, Kasasa S, Ssendagire S, Nattimba M, Ssengooba F. Male-Female Differences in Sexual Behaviors and HIV Sero Prevalence among Workers in Socializing Places: Results from PLACE Survey, Uganda. Int J AIDS Res. 2018;5(1):161-167. doi: dx.doi.org/10.19070/2379-1586-1800032
Copyright: Babirye S© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Compared to the traditionally defined special populations, little is known about the sexual behaviors and HIV prevalence of workers in socializing places like bars, lodges e.t.c., yet they constitute a subgroup with likely vulnerability and risk of HIV infection. Our aims were to investigate into and compare behavioral characteristics and HIV prevalence among female and male workers of socializing places.
Methods: The data used in this study are part of a large survey conducted in Uganda between 2013 and 2014 using a descriptive cross sectional study design. A total of 3830 workers from 736 socializing places from 29 districts of Uganda were interviewed and tested for HIV. The study employed descriptive univariate analysis.
Results: The burden of HIV was found to be highest among the female workers (11%) although male workers reported more risky sexual behaviors such as multiple sexual partnerships and high sexual partner acquisition. The prevalence of HIV was particularly very high among three categories of female workers namely; 1) those who reported having met a sexual partner on site, 2) those who reported any STI symptoms, and 3) those who reported being divorced/separated or widowed.
Conclusion: Despite the noted differences and similarities in the sexual behaviors and HIV prevalence of the male and female workers of socializing places, HIV prevention interventions must target both male and female workers because of the high sexual mixing prevalent at socializing sites.
2.Abbreviationsx
3.Introduction
4.Methods
4.1 Study Design
4.2 Study Site
4.3 Study Population and Sample
4.4 Data Collection Methods
5.Findings
5.1 Characteristics of Respondents (workers in HTAs)
5.2 Risky Sexual Behavior
5.3 HIV Seroprevalence of Workers at Socializing Places
6.Discussion
7.Conclusions
8.Funding
9.References
Keywords
Workers of Socializing Places; Male-Female Differences; Key Population; HIV Prevalence; HIV Risk Behaviors; HIV Prevention; Sex Work.
Abbreviations
STIs: Sexually Transmitted Infections.
Introduction
With approximately 1.8 million new HIV infections occurring annually, HIV remains a major public health concern world over [1]. Globally, special populations continue to face a disproportionate risk of HIV infection and onward transmission. According to UNAIDS, between 40 and 50 percent of all new HIV infections among adults worldwide occur among people from key populations and their immediate partners. The situation is not any different in Uganda, where 1.2 million people are living with HIV and key populations in particular disproportionately affected [2]. In 2015/16 for example, sex workers and their clients accounted for 18 percent of all new HIV infections in Uganda [2]. Relatedly, HIV prevalence generally remains high among the different special populations in Uganda. For example; HIV prevalence among sex workers, partners of sex workers, men who have sex with men, men in uniformed services, and fishing communities in Uganda was estimated at 37, 18, 13, 18.2 and 22 percent respectively [2]. Among people who inject drugs and plantation workers in Uganda, the prevalence of HIV stands at 16.7 and 7 percent respectively (Commission, 2010; IHRA, 2014).
The risk of HIV acquisition and/or transmission is usually determined by a combination of behavioral, biological and structural factors, such as the frequency of unprotected sexual intercourse, a high number of concurrent sexual partners, the presence of other sexually transmitted infections (STIs), limited access to prevention and treatment services, social stigma and discriminatory legal or regulatory policies [3, 4]. Relatedly, efforts to prevent HIV epidemic in the past have led to a clear understanding that individual behaviors are central in shaping one’s risk and vulnerability to HIV acquisition and transmission [3].
A number of studies have established that high risk sexual behaviors are related to the working environment. For example, a study conducted among commercial sex workers, showed a substantial variation in potential risks of HIV infection by organization of work and working conditions [5, 6]. In Tanzania, women working in bars were considered to be at high risk of HIV infection by local health authorities [7]. Another study in China found that women working in entertainment establishments or personal service (e.g. massage parlours, dance halls, nightclubs, bars, barbershops, beauty salons, etc.) were more likely to engage in risk and non-protective sexual behaviors than women working in non-entertainment establishments (e.g., restaurants, factories, or domestic service, etc.) [8]. The relationship between work setting and an individual behaviors was also supported by the effectiveness of establishment-based HIV/STD prevention intervention activities [3, 9, 10]. It is against this background that this study aimed to survey sexual behaviors and HIV sero prevalence among workers at public socializing places in Uganda. Socializing places are public places where one can go to relax, have fun, drink alcohol or find a sexual partner. Workers in such places constitute a subgroup with likely vulnerability and risk of HIV infection. The vulnerability of workers in socializing places stems from the nature and dynamics of their work and the work lifestyle in which a number of known or hypothesized ‘risk factors’ converge. Because workers in socializing places are a heterogeneous population in terms of gender, exploring their male-female differences in sexual behaviors and HIV sero prevalence may help policy makers and implementers to develop appropriately targeted prevention intervention strategies among this vulnerable subpopulation.
The data used in this study are part of a larger population-based survey conducted in Uganda between 2013 and 2014 using a descriptive cross sectional study design. The study used the PLACE method. The detailed PLACE methodology is described elsewhere [19]. During data collection, we identified places of socialization - especially were new sexual partnerships where known to form and at these places we conducted a survey of those working at the sites. During the survey we interviewed and provided HIV counseling and testing to 3,830 workers across 29 districts of Uganda.
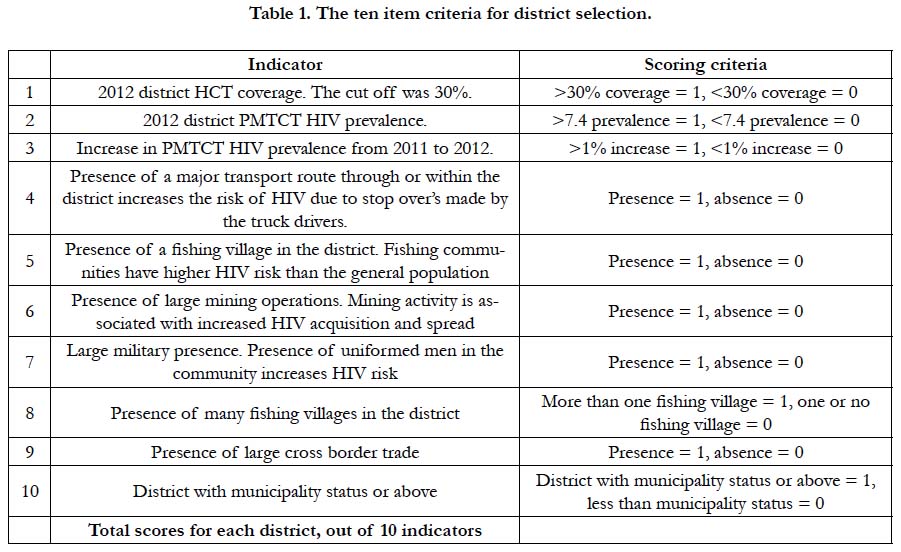
The selection of the 29 districts was based on a 10 item criteria determined by national level HIV stakeholders (UAC, MOH and USAID). This criterion ranked all the 112 districts by HIV risk on a scale of 0 to 10 across each criteria (see Table I). Using the total scores on the criteria, the districts were ranked and categorized into 3 strata namely; high risk, medium risk and low risk. Using STATA software, 15 districts in the high risk strata were selected, nine selected from medium risk districts and five from low risk districts. This was intended to include more of the high risk districts in the study – in part to support the Uganda HIV control programs and Commission to better target district with more risks of HIV transmission. Selected districts included: Jinja, Iganga, Tororo, Mbale, Sironko, Soroti, Kapchworwa, Moroto, Arua, Nebbi, Lira, Pader, Kitgum, Kisoro, Kabaale, Kibale, Mbarara, Kasese, Bushenyi, Masaka, Mpigi, Kayunga, Nakasongola, Hoima, Kamwenge, Kanungu, Kalungu, Kalangala and Dokolo. The study was piloted in Mityana district however; the pilot data was not included in the analysis due to the major changes introduced to the data collection tools after the pilot.
The study population comprised of workers at socializing venues and events in the HTAs. All men and women aged 15 and over who worked at socializing venues and events were considered in the study irrespective of their educational and marital status. The sampling frame was the list of all verified and mapped venues and events from identified by a prior step in the PLACE methodology where community level of key informants were asked to identify public places where people in their community go to socialize and meet new sexual partners. From each district, a sample of 70 workers at socializing venues and events was selected to participate in the study. The 70 workers were drawn from the 30 socializing venues/events that were sampled from all the identified venues/ events across the selected HTAs in the district. All workers at the selected sites were offered the opportunity to participate in the study.
A semi structured questionnaire was used to collect data for this study. The questionnaire included questions about sociodemographic information, sexual behavior, and exposure to HIV prevention programs. The most sensitive sexual behavior questions were administered by the interviewer reading the questions and the respondent marking answers on a separate pre-printed answer sheet, which was later placed in an envelope without the interviewer seeing the responses. Upon arrival at each venue, a field supervisor explained to in-charge of the site the aim of the study and HIV testing and how it will be carried out to potential participants. Supervisors further explained in entail the HIV testing component; free HIV testing and how if one does not want to receive the results on spot, would still have an opportunity to receive them form a health facility in most convenient but accredited to offer VCT. New cases would be linked to HIV care services in the respective districts. They also established the number of workers at the venue/event and sought permission to request the participation of workers. Similarly, the workers were informed about the survey and testing, and asked to participate. To participate, a worker had to consent to both interviews and an HIV test.
The interviews were held at a convenient place (a small distance away from patrons or workers) to enable privacy of the interview, counseling and testing. To generate data on HIV prevalence, all workers who were interviewed were also tested for HIV. The HIV testing and counseling provided included a rapid HIV test, using the standard national testing and counseling protocol. Participants were counseled before and after the HIV test and those who wished to receive their HIV results, received them after the interview. For workers not ready to receive results, an information sheet with contacts and location of the HCT service provider in the district was provided along with a bar code of their blood sample. The bar code assisted in retrieving test results from the HCT provider records. The HIV test results were recorded in the routine records of HCT provider and on a separate sheet was used to record the test results and bar codes for study analysis. The study received ethical approval by the University of North Carolina, Makerere University School of Public Health, and national council of science and technology.
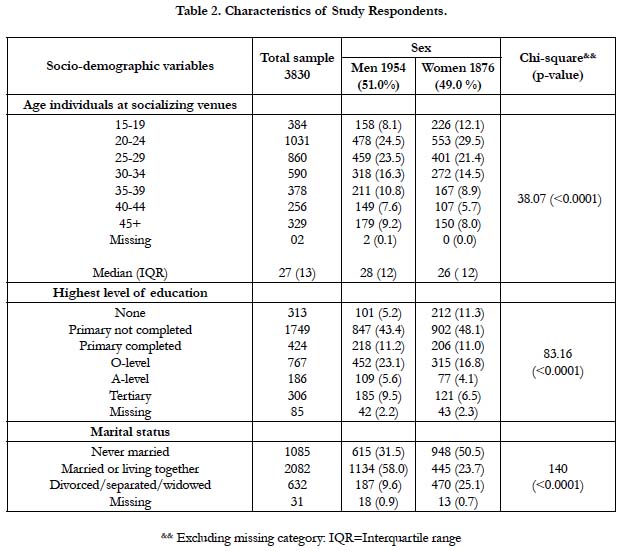
A total of 3,830 workers from 736 socializing places were analyzed in this study. Majority of the study respondents (59.3 percent) were below 30 years. The mean age of the study respondents was 29.5 years (SD=9.7) and the age range was 15-45 years. The sex composition of the study respondents was almost similar; 51 and 49 percent males and females respectively. Majority of all respondents (64.9 percent) had primary education or no education at all while 58 percent of all male workers were married. Among the female workers, 75 percent were not married or living with a partner (details can be seen in Table II).
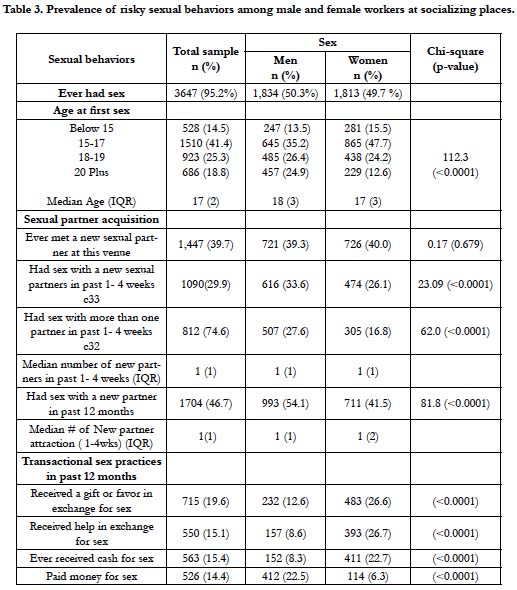
Majority of the respondents reported having initiated sex at an early age. By 15 years, 13.5 and 15.5 percent of male and female workers had initiated sex respectively. Nearly 4 in 10 (39.6 percent) of all the study respondents reported having met a new sexual partner at a socializing place where the interview took place. The frequency of multiple, concurrent and non-marital sexual partnerships was high among the study respondents.
The rate of new sexual partnerships in a population is an important determinant of the course of an HIV epidemic. In the 12 months preceding the study, 54.1 percent of the male workers and 39.2 percent of female workers reported having had sex with a new partner. Of these respondents, 32.9 percent of the male workers and 25.4 percent of female workers had sex with a new partner in the four weeks that preceded the interviews. Transactional sex practices were common among the study respondents but mostly among the female workers. In the previous 12 months, 26.6, 26.7, 22.7 and 6.3 percent of the female respondents had received gifts or favors in exchange for sex, received help with expenses in exchange for sex, had received cash in exchange for sex and paid cash for sex respectively. Twenty two percent of the male workers had paid cash for sex. Generally, women were on the receiving end while men were on the giving end (details can be seen in Table III).
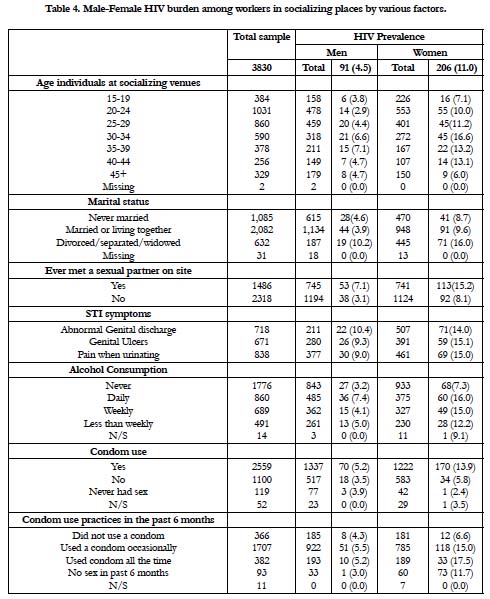
To generate data on HIV prevalence, all workers at socializing places who gave consent were interviewed and tested for HIV. National guidelines for HIV testing and counseling were followed in the study. Overall, the HIV prevalence was high (7.7 percent) among the workers of socializing places. HIV prevalence was highest among the females (11%). In particular, the prevalence of HIV was very high among the female workers who reported having met a sexual partner on site (15.2 percent) and those who reported STI symptoms and regular alcohol consumption (details can be seen in Table IV). When stratified by condom use practice, the study revealed a high HIV prevalence among both male and female workers that ever used condoms in the past 12 months that preceded the study and those who reported.
Discussion
Overall, our results show some similarities and some differences in the sexual behaviours and HIV burden of males and female workers of socializing places in Uganda. First, the female workers of socializing places bear a disproportionately high burden of HIV. Secondly, the male workers of socializing places highly practice risky sexual behaviours compared to their counterparts, the female workers. We found that the prevalence of HIV was particularly very high among three categories of female workers namely; 1) those who reported having met a sexual partner on site, 2) those who reported any STI symptoms, and 3) those who reported being divorced/separated or widowed. This high burden of HIV in the current study (especially among the female workers) coupled with the high prevalence of risky sexual behaviours among both male and female workers of socializing places, points to the potential of this subgroup to transmit HIV to; each other (through co-worker sexual partnerships), and to their patrons (through worker-patron sexual partnerships). In turn, HIV could be transmitted to the general population through the other sexual partners (main or causal) of workers and patrons of socializing places.
We believe that our study is one of the first to report on both sexual behavioral characteristics and HIV burden of workers in socializing places on a large scale (many study districts) worldwide. We found that workers of socializing places highly practiced risky sexual behaviors. Moreover many especially the female workers initiated sex at a very young age. This is of great concern because early initiation of sexual intercourse was earlier noted to put adolescents, particularly females, at elevated risk of acquiring HIV or other sexually transmitted infections (STI), and of other negative social and psychological outcomes [12]. Relatedly, early sexual debut has been associated with a greater number of sexual partners, lower levels of condom use, a greater chance of unintended pregnancy and a higher risk of self-reported STDs, as well as with other risk behaviors, including alcohol and drug use [13-15]. No wonder in the current study, even in the youngest workers (below 20 years), sexual activity and sexual risk behaviors were reported at rates implying substantial risk among both males and women.
We also found that both male and female workers of socializing places equally reported having met a sexual partner on site. The male workers in particular, were two to three times likely to have had sex with a new partner within the past 4 weeks that preceded the study. Likewise, they (male workers) were two times more likely to have had a new sexual partner in past 12 months than their counterparts, the female workers. Our findings on new sexual partner acquisition rates reinforce the findings from other studies that have used the PLACE method [16, 17]. The current study however provides additional insights into the differences and similarities in the sexual behaviors and HIV status of male and female workers i.e. it shows that male workers had more rates of sexual partnerships than the female workers. Although the female workers in the current study tended to report fewer sexual partners/partnerships, they report high transactional sex practices. Female workers were at least twice to three times likely to get involved in transactional sex more than the male workers. This finding is consistent with the findings from a study conducted in Cambodia among entertainment workers; which showed that female workers of socializing places i.e. entertainment places practiced disguised sex work in addition to having multiple sexual relationships [18]. Even though more male workers practiced risk sexual behaviors, prevention programs should not exclude female workers at socializing places, because they bear the highest burden of HIV but also commonly practice transactional sex.
It is not surprising that the prevalence of HIV observed in the present study is higher than the national estimate in Uganda which stands at 6.3 percent [2]. The prevalence of HIV among female workers in the current is two times higher than that of the male workers. This finding speaks to the uneven burden of HIV infections among males and females that has persisted over time. Since the start of the global HIV epidemic, HIV in many regions including sub-Saharan Africa (SSA) has disproportionately affected women. Evidence shows that women living in SSA are disproportionally affected by HIV/AIDS, accounting for 59 % of all infections in this region [1].
In a study in Kisumu (Kenya) and Ndola (Zambia), (Glynn et al., 2001) observed that in both sites HIV prevalence in women was six times that in men among sexually active 15-19 year olds and three times that in men among 20-24 year olds. Others studies Stephan et al., (2012) and Gylynn et al., (2001), have further observed that specific groups of women are disproportionately affected by HIV. For example, the study in Kenya and Zambia by Glynn et al., (2001) noted an equal HIV prevalence among males and females aged 25-49 years. One possible explanation for the uneven burden of HIV infections among the males and females workers in socializing places in the present study could be because majority of the female workers (composition) in the present study are young, unmarried, less educated and impoverished. Previous research has shown that the above factors predispose women to transactional sex practices [19]. Another related possible reason for the high HIV burden among female workers of socializing places could be because many reported meeting sexual partners on site, pointing to a possibility of disguised sex work.
While this study provides information on the sexual behaviors and HIV prevalence of workers of socializing places and also shows a comparison between males and female workers, there are a number of cautionary notes in interpreting its findings. First, the current study used data from a cross-sectional survey, thus time sequence and casual relationships among the variables of interest could not be established. Second, many of the outcomes we present in this study were self-reported by the participants and may thus have been subject to social desirability bias. Although many participants were willing to report on “undesirable” outcomes such as sexual activity, sexual partnership formation, and condom use, the prevalence values we report may underestimate the true values of these sexual behaviors. However, the bio-mark identified HIV positive cases among those who tested are objective measures and not subject to any biases as self-reported responses. Third, although anonymity and confidentiality were emphasized during data collection in PLACE, premarital sex and high-risk sex behaviors are socially unacceptable in Uganda, so the prospect of under reporting should be acknowledged. Nevertheless, our study provides important insight into the differences and similarities in sexual behaviors and HIV burden among workers in socializing places and the general population of Uganda. Our findings make a vital contribution to the understanding of the vulnerabilities of workers in socializing places in terms of HIV acquisition and transmission.
In spite of its limitations, the study has important public health implications. Our findings add to the growing body of evidence suggesting that workers of socializing places urgently need to be prioritized and targeted with HIV interventions that are tailored to their particular prevention needs. The risky sexual behaviors highlighted in our study, coupled with the high HIV burden and high rates of sexual partnerships points to this subgroup as a core population in HIV transmission. Whereas there were notable differences in the sexual behaviors and HIV prevalence of male and female workers of socializing places, HIV prevention efforts should not focus on a single gender given the high rates of sexual mixing at socializing places (venue-based sexual networks). Preventing transmission among this subgroup with high rates of partner change is desirable because it would prevent more secondary cases per primary case. We recommend venue-based HIV interventions. Venue-based approaches to STI prevention are not new, they have been supported by several studies [4, 17, 20]. Venue-based interventions have also been found to be effective [20]. For example, in China, an intervention consisting of outreach visits to sex workers in entertainment venues in five provinces increased condom use and decreased the prevalence of gonorrhea and chlamydia [21]. In general, it is likely that to reach workers of socializing places with venue-based HIV interventions, implementers will need to work closely with venue managers and the workers of socializing places themselves.
Conclusions
Despite the noted differences and similarities in the sexual behaviors and HIV prevalence of the male and female workers of socializing places, HIV prevention interventions must target both male and female workers because of the high sexual mixing prevalent at socializing sites. Whereas the male workers highly practices risky sexual behaviors, the female workers commonly engaged in transactional sex practices and had the highest burden of HIV. These findings reinforce prior evidence that sexual partnerships are often initiated at socializing venues and thus venue-based HIV interventions are necessary (Pitpitan & Kalichman, 2016 [20]; Singh et al., 2012 [4]), and not missing a combination of structural interventions. To the extent possible, venue-based HIV interventions should not exclude the patrons of socializing places as often are included in the venue-based sexual networks.
Funding
The study was supported by USAID Mission through Measure Evaluation, University of North Carolina-Chapel Hill.
References
- UNAIDS .Terminological guidelines. Switzerland; 2011 Oct. p.1-40.
- The Uganda Population-Based HIV Impact Assessment 2016-17. WHO/MOH-UG. 2017.
- Ford K, Wirawan DN, Fajans P, Meliawan P, MacDonald K, Thorpe L. Behavioral interventions for reduction of sexually transmitted disease/HIV transmission among female commercial sex workers and clients in Bali, Indonesia. AIDS. 1996 Feb;10(2):213-22. PubMed PMID: 8838711.
- Singh K, Brodish P, Mbai F, Kingola N, Rinyuri A, Njeru C, et al. A venuebased approach to reaching MSM, IDUs and the general population with VCT: a three study site in Kenya. AIDS Behav. 2012 May;16(4):818-28. doi: 10.1007/s10461-011-0103-z. PubMed PMID: 22198312.
- Ford K, Wirawan DN, Fajans P. Factors related to condom use among four groups of female sex workers in Bali, Indonesia. AIDS Educ Prev. 1998 Feb;10(1):34-45. PubMed PMID: 9505097.
- Jackson L, Highcrest A, Coates RA. Varied potential risks of HIV infection among prostitutes. Soc Sci Med. 1992 Aug;35(3):281-6. PubMed PMID: 1519080.
- Mgalla Z, Pool R. Sexual relationships, condom use and risk perception among female bar workers in north-west Tanzania. AIDS Care. 1997 Aug 1;9(4):407-16. PubMed PMID: 9337885.
- Yang H, Li X, Stanton B, Fang X, Lin D, Mao R, et al. Workplace and HIVrelated sexual behaviours and perceptions among female migrant workers. AIDS Care. 2005 Oct;17(7):819-33. PubMed PMID: 16120499.
- Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. Lancet. 1997 Nov 22;350(9090):1500-5. PubMed PMID: 9388397.
- Miller RL, Klotz D, Eckholdt HM. HIV prevention with male prostitutes and patrons of hustler bars: replication of an HIV preventive intervention. Am J Community Psychol. 1998 Feb;26(1):97-131. PubMed PMID: 9574500.
- Weir S, Tate J, Hileman SB, Khan M, Jackson E. PLACE. Priorities for Local AIDS Control Efforts: a manual for implementing the PLACE method. 2005.
- Hayes CD. Risking the future: Adolescent sexuality, pregnancy, and childbearing, Volume II: Working Papers and Statistical Appendices. National Academies; 1987. PubMed PMID: 25032470.
- Coker AL, Richter DL, Valois RF, McKeown RE, Garrison CZ, Vincent ML. Correlates and consequences of early initiation of sexual intercourse. J Sch Health. 1994 Nov;64(9):372-7. PubMed PMID: 7877279.
- Jakobsen R, Rise J, Aas H, Anderssen N. Noncoital sexual interactions and problem behaviour among young adolescents. The Norwegian Longitudinal Health Behaviour Study. J Adolesc. 1997 Feb;20(1):71-83. PubMed PMID: 9063776.
- Santelli JS, Brener ND, Lowry R, Bhatt A, Zabin LS. Multiple sexual partners among US adolescents and young adults. Fam Plann Perspect. 1998 Nov-Dec;30(6):271-5. PubMed PMID: 9859017.
- Figueroa JP, Dolan CB, Dale D, Hileman SB, Weir S. An assessment of sites where persons go to meet sexual partners in St. James, Jamaica, using the PLACE method. Sex Transm Dis. 2007 Jun;34(6):410-5. PubMed PMID: 17038963.
- Wohl DA, Khan MR, Tisdale C, Norcott K, Duncan J, Kaplan AM, et al. Locating the places people meet new sexual partners in a southern US city to inform HIV/STI prevention and testing efforts. AIDS Behav. 2011 Feb;15(2):283-91. doi: 10.1007/s10461-010-9746-4. PubMed PMID:20614175.
- Examining life experiences and HIV risks of young Entertainment Worker in four Cambodian cities. MoEYS. 2012.
- Mojola SA. Fishing in dangerous waters: Ecology, gender and economy in HIV risk. Soc Sci Med. 2011 Jan;72(2):149-56. doi: 10.1016/j.socscimed. 2010.11.006. PubMed PMID: 21146910.
- Pitpitan EV, Kalichman SC. Reducing HIV risks in the places where people drink: prevention interventions in alcohol venues. AIDS Behav. 2016 Jan;20 Suppl 1:S119-33. doi: 10.1007/s10461-015-1116-9. PubMed PMID: 26099244.
- Rou K, Wu Z, Sullivan SG, Li F, Guan J, Xu C, et al. A five-city trial of a behavioural intervention to reduce sexually transmitted disease/HIV risk among sex workers in China. AIDS. 2007 Dec;21 Suppl 8:S95-101. doi: 10.1097/01.aids.0000304703.77755.c7. PubMed PMID: 18172399.