Medical Emergencies In Dentistry – A Guide To A Successful Practise
Saraswathi Gopal. K1*, Sangavi. R2, Mahesh Kumar .P3
1 Faculty of Dentistry, Department of Oral Medicine and Radiology, Meenakshi Academy of Higher Education & Research; Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
2 Postgraduate student, Department of Oral Medicine and Radiology, Meenakshi Academy of Higher Education & Research; Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
3 Faculty of Dentistry, Department of Oral Medicine and Radiology, Meenakshi Academy of Higher Education & Research; Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
*Corresponding Author
Saraswathi Gopal. K,
Faculty of Dentistry, Department of Oral Medicine and Radiology, Meenakshi Academy of Higher Education & Research; Meenakshi Ammal Dental College, Chennai, Tamil Nadu, India.
Tel: 09940588033
E-mail: sangaviramesh12@gmail.com
Received: July 17, 2021; Accepted: November 10, 2021; Published: November 12, 2021
Citation: Saraswathi Gopal. K, Sangavi. R, Mahesh Kumar .P. Medical Emergencies In Dentistry – A Guide To A Successful Practise. Int J Dentistry Oral Sci. 2021;8(11):4991-4996. doi: dx.doi.org/10.19070/2377-8075-210001005
Copyright: Saraswathi Gopal. K©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Introduction
An emergency is a medical condition that requires immediate
attention and successful management. It is an unforeseen event
that leads to bodily injury, central nervous system stimulation
and depression, respiratory, circulatory disturbances, and allergic
reactions, etc [1]. An emergency is a medical condition that
demands immediate attention and successful management. It is
an unforeseen event that leads to bodily injury, central nervous
system stimulation and depression, respiratory, circulatory disturbances,
and allergic reactions, etc [1]. These are the life-threatening
situations of which every dental practitioner must be aware so
that unwanted morbidity can be avoided. Dentists, through their
knowledge, should be familiar with the prevention, diagnosis, and
management of common emergencies. In addition, the dentist
should be well trained and be aware of what to be done and can
act promptly. As these skills are not used every day, regular review
is necessary at least annually but preferably more often.[2] Emergencies
can be prevented to a certain extent by recording a detailed
medical history, doing a complete physical examination, and
thorough patient monitoring throughout the procedure. Preparation
for an emergency and sound knowledge about the management
of all emergencies, in general, is of major concern to
dental specialists these are the life-threatening situations of which
every practitioner must be aware so that unwanted morbidity can
be avoided. Dentists, through their knowledge, should be familiar
with the prevention, diagnosis, and management of common
emergencies. In addition, the dentist should be well trained and
be aware of what to be done and can act promptly. As these skills
are not used every day, regular review is necessary at least annually
but preferably more often.[2] Emergencies can be prevented
to a certain extent by recording a detailed medical history, doing
a complete physical examination, and thorough patient monitoring
throughout the procedure. Preparation for an emergency and
sound knowledge about the management of all emergencies, in
general, is of major concern to dental specialists.
Basic Principles Of Management Of Medical Emergencies
For salivary contamination, Fresh human saliva collection was
done from one healthy nonalcoholic, nonsmoking individual who
had refrained from eating and drinking 2h before saliva collection,
and with the informed consent of the donor.
The basic algorithm in managing any emergency is rendering basic
life support (BLS) measures and cardiopulmonary resuscitation
(CPR). This is done by following the basic principles: Position
(P), Airway (A), Breathing (B), Circulation (C), and Definitive
therapy (D) [1]. The basic positions to manage an emergency are
supine position, Trendelenburg position, and semi-erect position.
Maintaining a patent and functioning airway is the first and important
procedure in managing an emergency. This is achieved
usually by the head tilt-chin lift maneuver. [4] If the patent airway
is not achieved, then invasive procedures like direct laryngoscopy
and cricothyrotomy can be carried out. The next priority is to
check for the presence of adequate breathing is assessed by the
look-feel and listen-to technique.[2] If spontaneous breathing is
not evident then rescue breathing should be initiated immediately
either by the mouth-to-mouth technique or the bag-valve-mask
technique. Once patent airway patent and breathing is established,
circulation is assessed. The ideal and reliable method is by palpating
the carotid pulse at the region of the sternocleidomastoid
muscle. In case of absence of pulse, then CPR is initiated immediately.
When airway, breathing, and circulation are maintained,
definitive treatment is initiated. Definitive therapy involves the
administration of an ideal drug to relieve symptoms. The medical
emergencies that are commonly encountered in dental practice
such as syncope, airway obstruction, anaphylaxis, local anesthetic
toxicity, asthmatic attack, chest pain, hemorrhage, and seizure.
Analysis of the history, patient counseling, and motivation plays a key role in reducing emergencies.
Syncope
Syncope is a general term referring to a sudden, transient loss
of consciousness that usually occurs secondary to a period of
cerebral ischemia.[3] The predisposing factors for syncope are
of two types 1) psychogenic factors and 2) nonpsychogenic. The
psychogenic factors for syncope are Fright, Anxiety, Emotional
stress, undesirable news, Sight of blood/surgical/dental instruments
Non -Psychogenic factors are Erect sitting or standing,
posture, starvation or a missed meal, Exhaustion, Poor physical
condition humid, crowded environment. Before going into syncope
patient will have certain signs and symptoms such as Warm
feeling in face and neck, pale or ashen coloration, sweating, feels
cold, abdominal discomfort, lightheadedness or dizziness, mydriasis
(Pupillary dilatation.), Yawning, Increased heart rate, a slight
decrease in blood pressure this is termed as known as presyncope
period. During syncope, the patient loses consciousness. Generalized
muscle relaxation will happen, Bradycardia (Weak thready
pulse.,Seizure (Twitching of hands, legs, and face.),Eyes open
(Out and up gaze.) Once the patient recovers during the post syncopal
period there will be a Variable period of mental confusion,
Heart rate increases (Strong rate and rhythm.), Blood pressure
back to normal levels.
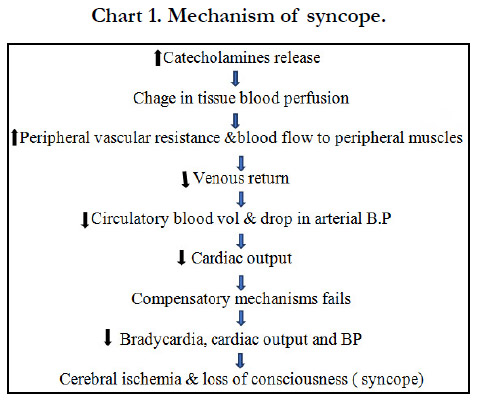
Pathophysiology of syncope
The critical level of cerebral blood flow to maintain consciousness
is 30ml per 100gm per min when this level is not achieved
patient experiences syncope. When the body experiences Stress
the Catecholamines get released into the blood, this is the body’s
response to stress it is known as the “ fight or flight “ response.
Increased catecholamines will lead to changes in tissue blood perfusion
and decrease peripheral vascular resistance and increase
the blood flow to many tissues especially the skeletal muscles for
the muscular action to take place. If the expected muscular action
takes place the muscle will pump the blood back to the heart so
the blood pressure remains at a base level so the signs of syncope
don’t occur. when the muscular activity doesn’t take place, the patient
remains static in the dental chair. The blood starts pooling in
the periphery which leads to decreased cardiac output followed by
decreased in circulating blood volume and decreased arterial BP
this ultimately leads to decreased cerebral blood flow.[3]
Management of syncope
Check ABC Assess & open airway (head tilt &chin lift); assess
airway patency& breathing; assess circulation (palpation of carotid
pulse). Move on to definitive management administer 02.
Monitor vital signs. Administer aromatic ammonia vapor which is
a respiratory stimulant that helps to increase breathing and muscular
movement. Administer atropine 0.5mg either in IV or IM if
bradycardia persists. Once the patient recovers dental treatment
should be postponed [4].
Postural Hypotension
Postural hypotension also known as orthostatic hypotension is
defined as a drop in systolic blood pressure (BP) of at least 20
mm Hg or of diastolic BP of at least 10 mm Hg within 3 minutes
of standing erect when compared with blood pressure from the
sitting or supine position. The predisposing factors of postural
hypotension are Drugs such as anti-hypersensitive, opioids and
histamine blockers, Prolonged period of recumbency or convalescence,
Inadequate postural reflex, Late-stage pregnancy, Advanced
age, Venous defects in legs Physical exhaustion and starvation,
Chronic postural hypotension (Shy – Drager syndrome).
The patient will experience feeling lightheaded or dizziness, Blurry
vision, Weakness, Confusion, Nausea. All these ultimately lead
to fainting after standing up [3].
Pathophysiology of postural hypotension
When the patient is in the supine position the blood pressure is
equally distributed throughout the body When the body alters the
position to Semi supine the BP decreases by 2mm Hg for every 1
inch when the patient moves into supine to upright the Influence
of gravity in CVS is increased. Baroreceptor will sense this variation
in BP and increase the heart rate and venous constriction this
aids in the return of blood to the right side of the heart.
Management
The patient must be placed in a supine position with feet elevated.
ABC Assessed following which oxygen is administered at the rate
of 8-15ml per minute. patients vital signs are monitored and chair
reposition should be done slowly.
Foreign Body Airway Obstruction
Airway obstruction is generally caused due to accidental slippage,
aspiration of foreign objects, or laryngeal spasm. During dental
treatment, there is great potential for tiny objects to drop into
the posterior portion of the oral cavity and subsequently into the
pharynx.[3] Usage of Rubber dam, Gauze, Suction, Magill’s intubation
forceps, Ligature using dental floss Can help in preventing
the intraoral objects from slipping inside the airway.[5]
Signs and symptoms
The patient will Gasp for breath, grabs at the throat, Panic, Suprasternal
or supraclavicular retraction, Inability to speak, breathe,
cough these are general signs and symptoms. When there is partial
obstruction patient might experience Snoring, Wheezing, Crowing
sound on inspiration, Forceful cough, wheezing between
cough, Absent or altered voice sounds, disorientation, when there
is complete obstruction patient will not be able to make any noise.
[3, 4]
Management
If the object is visible with the help of the assistant place the
patient in a supine position or Trendelenburg position, the object
is retrieved using Magill intubation forceps, in the absence of an
assistant instruct the patient to bend over the arm of the chair
with their head down and Encourage the patient to cough to expectorate
the object. If it fails Kneel or stands behind the victim
and wraps arms around the victim’s waist and makes a fist with
one hand, Place the thumb side of the fist against the victim’s abdomen
[3, 6]. The hand should rest in the midline, slightly above
the umbilicus, and well below the tip of the xiphoid process Fist is
held with the other hand and pressed into the patient’s abdomen
with a rapid, forceful upward thrust. This can be repeated until
the object is expected. In the case of infants Back slaps can be
performed the infant is straddled over the rescuer’s arm with the
head lower than the trunk. Using the heel of the hand, the rescuer
delivers up to five back slaps forcefully between the infant’s
shoulder blades to dislodge the foreign body. If the foreign body
is not recovered Radiologist should be consulted and Obtain appropriate
radiographs and initiate medical consultation and Perform
bronchoscopy to visualize and retrieve the foreign body [3].
Asthma
Asthma is a chronic inflammatory disorder of the airways it is
characterized by recurrent and often irreversible airflow limitations
due to underlying inflammatory processes. Due to the inflammatory
reaction airway is filled with inflammatory cells will
lead to the deposition of collagen, mast cells will degranulate, and
leads to increased capillary permeability and edema formation
which leads to bronchospasm.[7] Patients might experience Intermittent
wheezing, Feeling of chest tightness, Dyspnea, Cough,
Agitations, Tachypnea. Precautions to be taken before treating
asthma patients. Confirm that they have taken their most recent
scheduled dose of medication, The patient’s metered-dose inhaler
bronchodilator should be on hand, Procedure should be done late
morning/afternoon, Emergency kit with a bronchodilator and
oxygen should be available, Avoid L. A with sodium metabisulphite,
avoid using dental materials that may elicit an asthmatic attack
i.e., dentifrices, fissure sealants, methyl methacrylate, fluoride
trays & cotton rolls which can trigger asthmatic events should be
avoided [8].
Management
The patient is positioned upright with arms thrown forward. A,
B, C is assessed. O2 and bronchodilators are administered via inhalation.
If the episode continues, epinephrine is administered
subcutaneously 0.01mg/kg up to 0.3 mg. When the episode subsides
discharge the patient and postpone the dental treatment if it
continues activate EMS.[9]
Diabetes Mellitus
Diabetes is the most common endocrine disorder. It is marked
by high levels of blood glucose resulting from defects in insulin
production, insulin action, or both.
Cardinal Features
polydipsia, polyuria, polyphagia, weight loss, poor wound healing,
weakness, frequent infections, obesity are the general symptoms
of diabetes.[7] xerostomia, burning sensations, gingival hyperplasia,
dental caries, periodontal disease, and candidal infections,
fruity (acetone) breath, the thickness of saliva are Oral manifestations
of diabetes.
Management
Patient with known diabetes Enquires about the Type, Medication,
dosage, date of the last visit, and HbA1c values. When a
patient is under control without serious complications dental procedures
can be carried out with precautions, Morning appointments
are preferred, during the procedure should be short, source
of glucose must be available in the dental office.[10] Insulin shock
occurs when blood glucose drops below 60 mg/dL in this condition.
confusion, sweating, tremors, agitation, anxiety, dizziness,
tingling or numbness, and tachycardia. Severe hypoglycemia may
result in seizures or loss of consciousness are the signs a patient
will develop in a dental chair during insulin shock. If the patient
is conscious administer 15g of oral carbohydrate. In unconscious
patients, 50ml of dextrose is given in 50% concentration or 1mg
glucagon intravenously, or give 1ml glucagon intramuscularly
at almost any body site. Following the treatment, the signs and
symptoms of hypoglycemia should resolve in 10 to 15 minutes,
once stabilized, the patient is transported to a hospital for definitive
care and observation. Postpone the dental procedure. When
the condition doesn’t cease activate EMS [3].
Seizures
Seizures are a paroxysmal event due to abnormal, excessive, hypersynchronisation
discharge from neuronal aggregates in the
CNS. Seizures are not considered to be life-threatening except
when followed by one another closely for an extended period.
Emergency management of a patient experiencing a seizure is
essentially preventing injury during the seizure and supportive
therapy post-seizure There are three main types of seizures Focal-
partial seizure, Generalized. A generalized seizure is further divided into three types Grand mal (tonic-clonic seizure), Petit
Mal (absence seizure), Status epilepticus [11].
Clinical features
During the prodromal phase, the patient may exhibit changes that
may be evident only to a relative, such as increased anxiety or
depression. A patient with a history of seizures may recognize the
development of an “aura” consisting of olfactory, visual, gustatory,
or auditory changes, during aura, treatment should be terminated
immediately before it progresses to the preictal phase. In
the preictal phase, patients will experience, myoclonic jerks, Diaphragmatic
muscles go into spasm. The ictal phase has Alternating
muscular relaxation and violent contractions along with frothing
and bleeding at the mouth Bleeding lasts for 2 to 5 minutes.
In the postictal phase, Tonic-colonic movements cease. Breathing
returns to normal. Consciousness gradually returns with disorientation,
relaxation occurs. These patients will have total amnesia
of the seizure [7].
Management
Recognize the problem (lack of response to stimulation). Place
the patient's supine position in the dental chair. Once the seizure
ceases (<5 minutes) reassure the patient. If intravenous access is
available diazepam (Valium) IV is administered at a dose of 0.2-
0.5mg for Child lesser than 5 years 0.2-0.5 mg slowly every 2-5
minutes with a maximum of 5mg, above 5 years [3, 7].
When the episode terminates allow the patient to recover, discharge
the patient with attender, postpone dental procedures. If
the condition pertains to more than 5mins activate EMS and start
with BLS until the medical help reaches.
Allergic reactions
Allergy has been defined as a hypersensitive state acquired through
exposure to a particular allergen, reexposure to which produces a
heightened capacity to react., involving the release of mediators
from mast cells. which occur within minutes, or up to a few hours,
after exposure to a provoking agent.[13] It can be mild, moderate,
or severe. The majority of cases are mild but any anaphylaxis has
the potential to become life-threatening" Anaphylaxis develops
rapidly, reaches peak severity within 5-30 min. It is usually lifethreatening
due to respiratory embarrassment.
Symptoms and signs include
The sensation of warmth, itching especially in the axilla and
groin, feeling of anxiety. Angioedema of the lip and tongue is
seen at early stages. Later these may progress into an erythematous
rash(urticaria), edema of the face and neck, bronchospasm,
and laryngeal edema.[3]
Pathophysiology of an anaphylactic reaction.
When an antigen and allergen invade the body for the first time,
the B cells will produce IgE antibodies against that particular antigen.
The IgE antibody binds to the surface of mast cells and basophils
when there is a subsequent exposure to the same antigen,
the antigen will bridge the gap between to IgE molecule which
will lead to degranulation of the cell and release of histamine and
other inflammatory mediators. The sudden release results in a
drop in blood pressure, flushing, itching, potentially respiratory
compromise, and potential death.[15]
Management
The first step is to Identify an anaphylactic reaction and to remove
the potential. The patient is shifted to supine position. If
breathing is difficult, allow them to sit Airway, breathing, circulation
is should be assessed. A Dose of 0.3-0.5mg epinephrine
(1:1000) is administered intramuscularly and repeat every 5 minutes
as needed [14].
Angina
Angina is defined as a characteristic thoracic chest pain usually
substernal precipitated by exercise, emotion, and relived by vasodilator
drugs.[20] The major clinical characteristic of angina is
chest pain. The sensation is defined as dull, aching, discomfort,
constricting, suffocating, crushing, heavy, and squeezing.
Dental therapy consideration
Prevention of acute episodes of angina during dental treatment
is achieved by minimizing stress so that the myocardial oxygen
demand of the patient is met. The stress reduction protocol is
particularly important in the management of the anginal patient.
Specific consideration must be given to the length of the appointment,
pain control during the treatment, and the use of sedation.
[18]. Patients with unstable or daily anginal episodes should be
considered for dental care limited to emergency treatment only
after consultation with the patient’s physician. Local Anaesthesia
without a vasoconstrictor is advised for these patients to avoid
angina episodes.
Management
Recognize the problem and terminate the dental treatment. Position
the patient comfortably on the dental chair perfectly supine
position. Assess A, B, C. Administer oxygen via nasal cannula and
nitroglycerine sublingually around 0.3-0.6mg [6]. Nitroglycerine
eliminates the pain in 2-4 mins, when pain resolves allow the patient
to rest and postpone the dental treatment. If the pain doesn’t
resolve administer aspirin around 160-325mg, monitor the vital
signs, and active EMS.
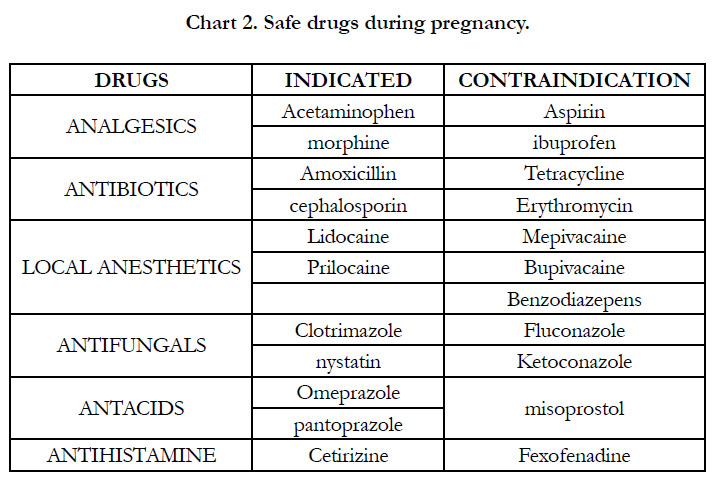
Management Of Pregnant Patients
Treatment of pregnant patients has the potential to affect the
lives of two separate individuals. Certain principles must be considered
in the treatment of pregnant patients so that, it benefits
the mother while minimizing the risk to the fetus.
Dental treatments can be modified but need not be withheld, provided
that the risk assessment is made properly.
The most commonly encountered problem in treating pregnant
women is a supine hypotensive syndrome, when a pregnant
woman is placed on a dental chair for a prolonged period it will
compress the inferior vena cava this leads to a decrease in arterial
oxygen tension and decreased uteroplacental perfusion with
Increased risk of developing deep vein thrombosis.[18] To avoid this patient should be tilted laterally around 5-15% on her left
side.
During the first Trimester rapid cell division and active organogenesis
occur between the second and the eighth week of postconception.
Therefore, there is a high risk of susceptibility to
stress and teratogens. 50% to 75% of all spontaneous abortions
occur during this period. So, the dental treatments are limited to
periodontal prophylaxis and emergency treatments only.[20]
During the second trimester the risk to the fetus is low as organogenesis
gets completed. Few elective and emergency dentoalveolar
procedures are more safely accomplished during the second
trimester.[20]
During the third trimester, the pregnant mother may experience
discomfort on the dental chair. Short dental appointments should
be scheduled with appropriate positioning in the chair. It is safe
to perform routine dental treatment in the early part of the third
trimester.[20]
A radiation dose of 10 Gy causes congenital fetal abnormalities.
The exposure of any radiographic films required for the management
of the pregnant patient in most situations should not
place the fetus at increased risk. Adequate shielding and protective
equipment must be used at all times.[19]
Haemorrhage
A hemorrhage is referred to as Prolonged or uncontrolled bleeding.
Hemorrhage is most commonly encountered in a dental setup
during extractions and minor surgical procedures. The medical
history of the patient plays an important role in the Management
of these patients. Make sure whether the patient is hematologically
normal or suffers from some disturbance in the normal clotting
mechanism. Uncontrolled and prolonged bleeding can occur
in some healthy patients after dental extraction.[7]
Local causes of hemorrhage originate in either soft tissue or bone
it is either arterial, venous, or capillary. Systemic causes include
patients with hereditary conditions such as hemophilia, Von
Willebrand’s disease, thrombocytopenia are susceptible to hemorrhage
following oral surgical procedures.
Local Management
Ligation of blood vessels, use of pressure packs, electrocautery,
hemostatic agents like vasoconstrictors in L.A. are used for local
management.
Systemic Management
Patients with mild bleeding disorders can be treated in a primary
care setting after consultation with the hematologist.Patients with
a moderate to severe level of bleeding disorder require invasive
dental procedures are best treated in a hospital setting. Before any
extractions or minor oral surgical procedures, a Complete blood
count should be performed. There is an 80% chance that a hemophilic
patient to develop a hematoma following the administration
of an inferior alveolar nerve block. The hematoma could be fatal
if it accumulates in the mediastinum and compromises the airway.
Preoperative prophylactic coverage should be discussed with the
hematologist.[23] Mental nerve block injection is considered safe
and requires no hematologic coverage before administration. A
mild form of hemophilia A and vWD are normally treated preoperatively
by desmopressin acetate. It can be administered intravenously,
subcutaneously, intranasally.[22] In severe forms before
dental extractions, patients require replacement therapy with factor
VIII as a prophylactic option and/or as emergency treatment
in case of prolonged bleeding. It is recommended to deliver the
intended dental treatment within 30-60 minutes following its administration.
It is necessary to measure the level of factor VIII in
patients with hemophilia A before any invasive dental procedures.
Tranexamic acid is given in the form of mouthwash with a concentration
of 15-25 mg/kg 4 times a day for 7-10 days; or oral
administration of tablets of 1 g, 3 times a day for 7-10 days. This
helps to add stability to the clot.
Conclusions
When we are prepared for an emergency, the emergency ceases to
exist. Measures should be taken to make sure the dental team is
well prepared to meet any medical crisis. Thorough knowledge is
required to understand the patient’s medical conditions to determine the risk factors associated with the condition. Modifications
of the treatment protocol are essential to handle patients with a
known history of certain medical conditions this helps to minimize
the risk. The dental team should exercise extreme caution to
identify the early signs and symptoms of an impending medical
emergency and render early and rapid treatment. Prompt recognition
and efficient management of medical emergencies by a wellprepared
dental team help to save lives.
References
-
[1]. Prasad KD, Hegde C, Alva H, Shetty M. Medical and dental emergencies
and complications in dental practice and its management. Journal of Education
and Ethics in Dentistry. 2012 Jan 1;2(1):13.
[2]. Council R. Medical emergencies and resuscitation: standards for clinical practice and training for dental practitioners and dental care professionals in general dental practice. Resuscitation Council (UK); 2008.
[3]. Malamed SF. Medical Emergencies in the Dental Office-E-Book. Elsevier Health Sciences; 2014 Oct 27.
[4]. Oujwoswini A. Management of Medical Emergencies in Dental Office. Indian Journal of Public Health Research & Development. 2019;10(9):1701-4.
[5]. Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: a 10-year institutional review. J Am Dent Assoc. 2004 Sep;135(9):1287- 91. PubMed PMID: 15493393.
[6]. Prasad KD, Hegde C, Alva H, Shetty M. Medical and dental emergencies and complications in dental practice and its management. Journal of Education and Ethics in Dentistry. 2012 Jan 1;2(1):13.
[7]. Burket’s Textbook of oral medicine-12th edition.
[8]. Steinbacher DM, Glick M. The dental patient with asthma. An update and oral health considerations. J Am Dent Assoc. 2001 Sep;132(9):1229-39. PubMed PMID: 11665347.
[9]. Claramunt Lozano A, Sarrión Pérez MG, Gavaldá Esteve C. Dental considerations in patients with respiratory problems.
[10]. Malik S, Singh G. deNtal MaNaGeMeNt OF diaBetiC PatieNtS: a CliNi- Cal RevieW. International Arab Journal of Dentistry. 2014 Feb 14;5(1).
[11]. Aragon CE, Burneo JG. Understanding the patient with epilepsy and seizures in the dental practice. J Can Dent Assoc. 2007 Feb;73(1):71-6. Pub- Med PMID: 17295949.
[12]. Continue CP. AAGBI Safety Guidelines.
[13]. Reed KL. Basic management of medical emergencies: recognizing a patient's distress. J Am Dent Assoc. 2010 May;141 Suppl 1:20S-4S. PubMed PMID: 20436086.
[14]. Thyssen JP, Menné T, Elberling J, Plaschke P, Johansen JD. Hypersensitivity to local anaesthetics--update and proposal of evaluation algorithm. Contact Dermatitis. 2008 Aug;59(2):69-78. PubMed PMID: 18759873.
[15]. Reber LL, Hernandez JD, Galli SJ. The pathophysiology of anaphylaxis. J Allergy Clin Immunol. 2017 Aug;140(2):335-348. PubMed PMID: 28780941.
[16]. Textbook of physiology Ak jain,2nd edition.
[17]. Samulak-Zielinska R, Dembowska E, Lizakowski P. Dental treatment of post-myocardial infarction patients: A review of the literature. Dent Med Probl. 2019 Jul-Sep;56(3):291-298. PubMed PMID: 31577073.
[18]. Kurien S, Kattimani VS, Sriram RR, Sriram SK, Rao V K P, Bhupathi A, et al. Management of pregnant patient in dentistry. J Int Oral Health. 2013 Feb;5(1):88-97. PubMed PMID: 24155583.
[19]. Giglio JA, Lanni SM, Laskin DM, Giglio NW. Oral health care for the pregnant patient. J Can Dent Assoc. 2009 Feb;75(1):43-8. PubMed PMID: 19239743.
[20]. Silk H, Douglass AB, Douglass JM, Silk L. Oral health during pregnancy. Am Fam Physician. 2008 Apr 15;77(8):1139-44. PubMed PMID: 18481562.
[21]. Dinkova A, Kirova DG, Delev D. Dental management and bleeding complications of patients on long-term oral antiplatelet therapy. Review of existing studies and guidelines. Journal of IMAB–Annual Proceeding Scientific Papers. 2013 Jun 4;19(2):298-304.
[22]. McCord C, Johnson L. Oral Manifestations of Hematologic. Oral Manifestations of Systemic Diseases, an Issue of Atlas of the Oral & Maxillofacial Surgery Clinics, E-Book. 2017 Aug 17;25(2):149.
[23]. Adeyemo TA, Adeyemo WL, Adediran A, Akinbami AJ, Akanmu AS. Orofacial manifestations of hematological disorders: anemia and hemostatic disorders. Indian J Dent Res. 2011 May-Jun;22(3):454-61. PubMed PMID: 22048588.