Evaluation Of The Effectiveness of High Insertion Torques on Implant Stability Quotient (ISQ) and Marginal Bone Loss of Implants in Posterior Mandible
Somar Dahdal1, Isam Alkhori2, Safaa Shihabi3*
1 Phd student in Department of Oral & Maxillofacial Surgery, Faculty of Dentistry, Damascus University, Syria.
2 Professor in Department of Oral & Maxillofacial Surgery, Faculty of Dentistry, Damascus University, Syria.
3 MSc in Pediatric Dentistry, Faculty of Dentistry, Damascus University, Syria.
*Corresponding Author
Safaa Shihabi,
DDS, MSc in Paediatric Dentistry, Damascus University, Syria.
E-mail: safaa2671991@gmail.com
Received: August 28, 2021; Accepted: October 15, 2021; Published: October 30, 2021
Citation: Somar Dahdal, Isam Alkhori, Safaa Shihabi. Evaluation Of The Effectiveness of High Insertion Torques on Implant Stability Quotient (ISQ) and Marginal Bone Loss of Implants in Posterior Mandible. Int J Dentistry Oral Sci. 2021;8(10):4887-4891. doi: dx.doi.org/10.19070/2377-8075-21000988
Copyright: Safaa Shihabi©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Implant stability is an indicator of the osseointegration of dental implants, as it affects the healing process and
success of osseointegration and it is usually related to the insertion torque during implant placement. As a matter of concern,
implants inserted with torques greater than 50 N/cm can cause excessive pressure on the surrounding bone with temporary
local bone necrosis.
Aim: Comparison the effect between high and low insertion torques on implants stability quotient and marginal bone loss of
implants in posterior mandible.
Methods: Twenty implants were inserted in 10 patients. Implants were divided into two groups according to high insertion
torque (Group A) and low insertion torque (Group B). ISQ was measured by ostell device and the marginal bone loss was
measured by CBCT.
Results: P.value was much lower than the value 0.05 after six months of implantation in the (Group A) according to the
thickness of the vestibular plates (in mm). also, the values of (ISQ) immediately after implantation and after 6 months in the
(Group A) were greater than in the (Group B).
Conclusion: High insertion torque(above 50 N/cm) leads a higher Implant Stability Quotient(ISQ) immediately after implantation
and after 6 months, compared with low IT (25-35 N/cm), and leads to higher buccal bone plate loss after 6 months
compared with low IT.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Dental Implants; Insertion Torque (IT); Implant Stability Quotient (ISQ); Bone Loss.
Introduction
The use of dental implants to replace missing teeth has become a
safe treatment method over the past decades [1]. The initial stability
of implants is one of the clinical factors that influencing the
success of the implant [2].
In 2006, Cochran presented a recent description of osseointegration,
which reflects the biodynamic process of the implant-bone
area, where the stability of the implant is represented by a dynamic
equilibrium between the existing bone (primary contact), and the
formation and remodeling of new bone (secondary contact) [3].
Bone healing around the implant involves a series of cellular and
extracellular life events that play a role on the implant surface with
the bone until the implant surface is covered by the new formed
bone [4].
During the first hours, the surface of the implant is covered with
serum proteins, followed by adherence of platelets, and the formation
of a fibrin clot, which is a reservoir for growth factors and
cytokines, providing a physical barrier that prevents the continuation
of bleeding. The shape of the outer surface of the implant is
also responsible for maintaining the stability of this blood formed
between the implant and the bone [5].
Implant stability is an indicator of the osseointegration of dental
implants, as it affects the healing process and success of osseointegration,
and it is a measure of the clinical movement of the
implant, and plays a role in the long-term success of dental implants, and its importance increases when it is used in the modern
treatment protocol as acceleration of treatment, where it is relied
on the stability of Implant when deciding to immediately load
implants [4].
The initial stability results from the mechanical attachment to
the cortical bone, and depends on the quantity and quality of the
bone at the recipient site, the design of the implant used, and the
surgical technique used to place the implant. The secondary or
vital implant stability is the increase in stability resulting from [6]
[7], and the process of bone formation and remodeling in the area
where the implant meets the surrounding bone [8].
The initial stability of the implants is usually related to the insertion
torque during implant placement. In addition, several studies
have suggested that the insertion torque (between 25-45 N/cm)
can prevent reversible microscopic movements (threshold level
between 50-100 µm), and this allows The healing process by osseointegration
[9].
It is clear that the high insertion torque of the implants gives the
surgeon a comfortable feeling that the implant is initially stable.
However, it may cause dangerous pressure on the bone surrounding.
Several studies have shown that high insertion torque may
cause micro-fractures with some absorption in the cortical region
and consequently a delayed healing process. Also, there are several
laboratory studies on animals that showed that high insertion
torque did not cause any bone necrosis or implant failure [10].
Even if the initial stability and insertion torque are not significantly
bound, implants inserted with torques higher than 20 N/cm
show higher success rates than implants with lower torques [11].
Although the available information is not clear or sufficient about
the ideal insertion torque to obtain good initial stability, it is clear
that the insertion torque is related to the initial contact between
the implant and bone surface [12].
As a matter of concern, implants inserted with torques greater
than 50 N/cm can cause excessive pressure on the surrounding
bone with temporary local bone necrosis. Excessive insertion
torque may also be responsible for the phenomenon of osteoporosis
due to pressure, such an effect may result in high failure rates
or delayed excessive loss of the cortical bone [12].
Materials And Methods
The sample consisted of 20 implants divided into 2 groups, the
group A included 10 implants of high torque (>50 N/cm) and
the group B included 10 implants of low torque (25-35 N/cm),
implant type is (Megagen, anyone). The patient's personal and
written consent to participate in the research was documented.
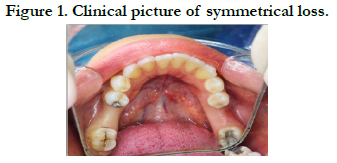
The inclusion criteria were:implant sites should be symmetrical
in the posterior mandible (Figure 1), the implant receiving socket
should be more than 6 mm wide, more than 6 months have
passed since the extraction at the implantation sites, length range
of implant is (10-11.5mm), Diameter range is (3.5-4.5mm), the
patient should have a good jaw relation between the jaws, absence
of severe abnormal oral habits, patients should be committed to
oral care, and have healthy periodontal tissues, Finally the patients
were non-smoker and non-alcoholic.
Furthermore the patients with acute and chronic periodontitis
and who have diseases that constitute a general contraindication
to implantation or surgery (such as uncontrolled diabetes patients,
osteoporotic patients, patients with hemorrhagic diseases, patients
who are not interested in oral health, and patients who are
taking any medication that affects bone healing) were excluded
from the study.
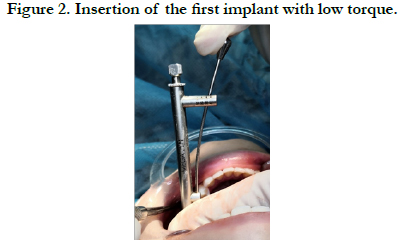
Surgical method of operation in the high torque
group:(Figure 3)
After performing local anesthesia, a crestalincision was made
without vertical incisions, and full thickness mucoperiosteal flap
was raised to gain access to the bone. A small round bur was used
to localize the sites where implants will be placed, The implant
cradle was drilled with burs 0.9 mm less than the implant diameter
as megagen implants were used. It is designed primarily for insertion
with high torques above 45N/cm, featuring a conical body, spaced helixes and a self-tapping type.
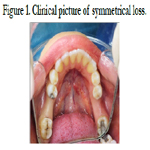
Surgical method in low torque group: (Figure 2)
After performing local anesthesia, a crestalincision was made
without vertical incisions, and full thickness mucoperiosteal flap
was raised to gain access to the bone. A small round bur was used
to localize the sites where implants will be placed,the cradle of
the implant was excavated and the burs reached the diameter of
the planned implant, where MEGAGEN implants were also used.
Postoperative recommendations.
- Maintaining the compressive gauze on the surgical area for an
hour.
-Apply cold compresses to the cheek skin corresponding to the
work area on the day of the surgery.
- Start using antiseptic rinses from the day following the surgery.
- the recall appointment should be after a week to remove the
surgical stitches.
The patient is also given a prescription that includes the following:
An antibiotic (amoxicillin + clavulanic acid) oral tablets at an
amount of 625 mg three times daily for a week.
A non-steroidal anti-inflammatory drug (ibuprofen) oral tablets
of 600 mg three times daily.
Oral rinse (chlorhexidine 0.12%) twice a day for a week starting
from the day after the operation to maintain the cleanliness of the
surgical site.
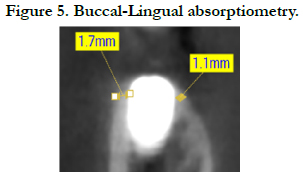
Radiological evaluation method for bone resorption. (Figure
5)
Immediately, after implantation, and after 6 months, a three-dimensional
image using conebeam computed tomography (CBCT)
were taken to evaluate bone resorption (buccal- lingual).
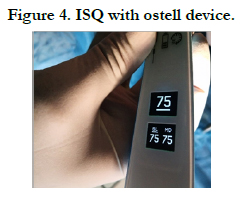
ISQ evaluation method: (Figure 4)
After the implants are inserted into the posterior symmetrical loss
areas of the lower jaw, the initial stability of the implant is measured
at both ends by means of the OSTELL device after inserting
an implant with a high torque and an implant with a low insertion
torque. Evaluation is done immediately after transplantation and
monitoring is done after 6 months.
Results
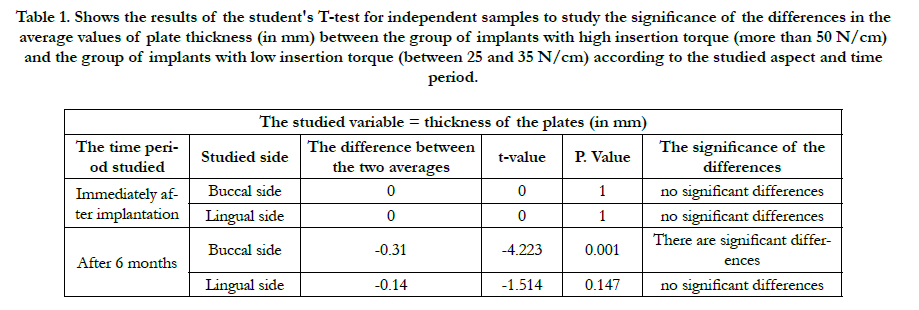
Studying the effect of the insertion torque applied to the implant
on the values of the plates thickness according to the studied side
and the studied time period:
P. value was much lower than the value 0.05 after six months of
implantation in the group of measurements made in the vestibular
side, so, at the 95% confidence level, there were statistically
significant differences in the average values of the thickness of
the vestibular plates (in mm) after six months. We conclude that
the values of the thickness of the vestibular plates (in mm) after
six months in the group A were smaller than in the group B.
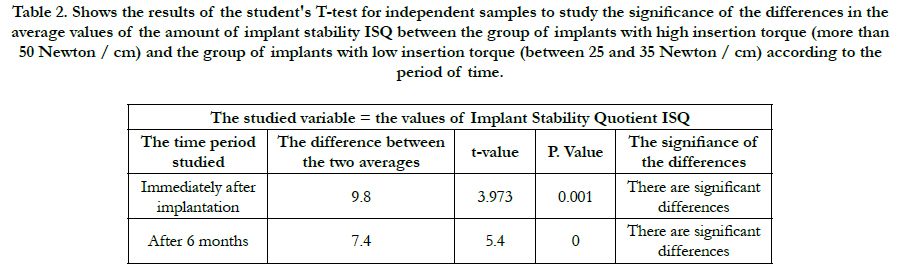
Studying the effect of the IT applied to the implant on the values
of the implant stability ISQ according to the studied time period:
P.value was much lower than the value 0.05 regardless of the time
period studied, so, at the 95% confidence level, there were statistically
significant differences in the average values of the amount
of implant stability between 2 groups immediately after implantation and after 6 months. We concluded that the values of (ISQ)
immediately after implantation and after 6 months in the group A
were greater than in the group B.
Table 1. Shows the results of the student's T-test for independent samples to study the significance of the differences in the average values of plate thickness (in mm) between the group of implants with high insertion torque (more than 50 N/cm) and the group of implants with low insertion torque (between 25 and 35 N/cm) according to the studied aspect and time period.
Table 2. Shows the results of the student's T-test for independent samples to study the significance of the differences in the average values of the amount of implant stability ISQ between the group of implants with high insertion torque (more than 50 Newton / cm) and the group of implants with low insertion torque (between 25 and 35 Newton / cm) according to the period of time.
Discussion
Osseointegration is a complex biological phenomenon directed
by a series of biochemical events that stimulate angiogenesis,
osteoblasts, mesenchymal cell differentiation, extracellular tissue
placement and ultimately the mineralization process [13].
The primary stability of the implants during implant insertion is
essential for obtaining stability, especially when masticatory pressures
are applied. It is a key factor in obtaining high rates of implant
durability [13].
There are several theories that concluded that the high insertion
torque of the implants may cause severe pressure on the bone,
which leads to bone necrosis as a result of cracks and pressure on
the bone [14]. On the other hand, many studies have shown that
to obtain a high rate of implant durability, we need a torque of at
least 20 N/cm [14].
Several studies in the medical literature demonstrated the relationship
between insertion torque and initial stability of the implant.
In the study of Ottoni et al 2005, it was found that a higher insertion
torque can improve implant stability rates. In a study conducted
by Trisi et al 2009, it was shown that the insertion torque
(higher than 80 N/cm) may cause micromovements that lead to
the failure of the implant in the end [9].
Antonio Barone and his colleagues demonstrated that implants
inserted with high-IT (>= 50 Ncm) group showed greater marginal
bone loss in the mandible than in the maxilla. This could be
attributed to the higher bone compression effects on the cortical
and poorly vascularized crystal bone, which is more represented
in the mandible than in the maxilla [15].
Khayat et al, did not observed any significant differences between
the low and high insertion torque groups and concluded that high
IT (up to 176) could not jeopardize the osseointegration healing
or increase the peri-implant bone loss [16].
The theory that high insertion torque can promote excessive bone
compression, generation dangerous micro-cracks, or pressure necrosis,
which disturb micro circulation and lead to bone resorption
was not confirmed because the meta-analysis indicated no
significant differences in terms of marginal bone level between high and regular or low insertion torque of the implant [17].
Moreover, many studies as (Moher D et al, Grandi T et al, Khayat
PG et al) did not show significant difference between high and
regular or low insertion torque [18, 19], except one study (Marconcini
S et al) that reported significantly high marginal bone loss
for implants placed with high insertion toque in the maxilla and
mandible [20].
According to the results of our current study, which included 20
implants, were performed in patients with symmetrical loss in the
posterior mandible in terms of the missing location and the quality
of the recipient bone. Thereby, our study disagrees with previous
studies as (Moher D et al, Grandi T et al, Khayat PG et al) and
this could be attributed to difference in implants sites between
jaws, different insertion torques and type of the used implant.
There are studies that showed a close relationship between insertion
torque of implants and initial stability, including (Baldi d. et
al 2018, Degidi M. et al 2012, Park KJ. et al 2012, Sarfaraz H. et al
2018), while other studies concluded that there is no association
between The insertion torque and the initial stability of implant,
including (Santamaría-Arrieta G. et al 2016, Açil Y. et al 2017),
and this difference in results is due to the different methodologies
between these studies [21].
In the study (JP do Vale Souza et al 2021), it was found that there
is a close correlation between the insertion torque and the initial
stability of the implant (P-Value = 0.022), which means that the
high insertion torque is the same as the initial high stability of the
implant and vice versa. This result is important because it indicates
two different variables in terms of the initial stability, but
they are compatible together, because the initial stability quotient
(ISQ) refers to the resistance to bending forces, while the insertion
torque refers to the resistance to the shear forces [21].
According to the results of our current study, in which 20 implants
were performed in patients with symmetrical loss in the
lower posterior region,We agree with the results of the study (JP
do Vale Souza et al 2021) that a higher insertion torque corresponds
to a higher initial stability of the implants. While we have
disagreed with several studies (MR Norton et al 2017, A. Simunek
et al 2012, AK de Oliveira Nicolau Mantovani 2018, FS Lages et
al 2018), this is due to the different type of implant placed, the
different places of loss and bone densities between the jaws and
within One jaw, and also a difference in the diameters and lengths
of the implants.
Conclusion
We conclude from our current study that a high IT (above 50
N/cm) leads a higher (ISQ) immediately, after implantation and
after 6 months compared with a low IT (25-35 N/cm), and leads
to higher buccal bone plate loss after 6 months compared with
low IT.
Acknowledgment
This research was funded by Damascus University.
References
-
[1]. Sclar A. Ridge preservation for optimum esthetics and function. The Bio-Col
technique. Postgrad Dent. 1999;6(1):3-11.
[2]. Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, Nedic M. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. Journal of periodontology. 1998 Sep;69(9):1044-9.Pubmed PMID:9776033.
[3]. Aimetti M, Romano F, Griga FB, Godio L. Clinical and histologic healing of human extraction sockets filled with calcium sulfate. International Journal of Oral & Maxillofacial Implants. 2009 Oct 1;24(5). PubmedPMID: 19865631.
[4]. Van der Weijden F, Dell'Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. Journal of clinical periodontology. 2009 Dec;36(12):1048-58.
[5]. Sclar AG. The Bio-Col Technique. In: Soft Tissue and Esthetic Considerations in Implant Therapy. Carol Stream, IL: Quintessence Publishing Co., 2003:75-112.
[6]. Norton MR, Wilson J. Dental implants placed in extraction sites implanted with bioactive glass: human histology and clinical outcome. International Journal of Oral & Maxillofacial Implants. 2002 Mar 1;17(2).
[7]. Tonetti, MS, Hammerle, CH. European Workshop on Periodontology Group C. Advances in bone augmentation to enable dental implant placement: Consensus Report of the Sixth European Workshop on Periodontology. Journal of Clinical periodontology., 2008; 35(Suppl): 168–172. PubmedPMID: 18724849.
[8]. Chen, ST,Buser, D. Clinical and esthetic outcomes of implants placed in postextraction sites. The International Journal of Oral & Maxillofacial Implants., 2009 ;24(Suppl): 186–217. PubmedPMID:19885446.
[9]. Dohan DM, Choukroun J, Diss A, DohanSL, Dohan AJ, Mouhyi J, et al.Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral RadiolEndod., 2006; 101:e37-44. PubmedPMID:16504849.
[10]. Wang HL, Kiyonobu K, Neiva RF. Socket augmentation: rationale and technique. Implant Dentistry. 2004 Dec 1;13(4):286-96.
[11]. Gupta D, Gundannavar G, Chinni DD, Alampalli RV. Ridge Preservation done ImmediatelyfollowingExtraction using Bovine Bone Graft, Collagen Plugand Collagen Membrane. International Journal of Oral Implantology and Clinical Research. 2012 Jan 1;3(1):8-16.
[12]. Sabelman EE. Biology, biotechnology and biocompatibility of collagen. Biocompatibility of tissue analogs. 1985:21-66.
[13]. Postlethwaite AE, Seyer JM, Kang AH. Chemotactic attraction of human fibroblasts to type I, II, and III collagens and collagen-derived peptides. Proceedings of the National Academy of Sciences. 1978 Feb 1;75(2):871-5. [14]. Sakka S, Coulthard P. Bone quality: a reality for the process of osseointegration. Implant dentistry. 2009 Dec 1;18(6):480-5. Pubmed PMID: 20009601.
[15]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2006 Mar 1;101(3):e45-50.
[16]. Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Scacco S, Inchingolo AD, et al. Trial with Platelet-Rich Fibrin and Bio-Oss used as grafting materials in the treatment of the severe maxillar bone atrophy: clinical and radiological evaluations. Eur Rev Med Pharmacol Sci. 2010 Dec 1;14(12):1075- 84.
[17]. Schwartz-Arad D, Chaushu G. The ways and wherefores of immediate placement of implants into fresh extraction sites: a literature review. Journal of periodontology. 1997 Oct;68(10):915-23.
[18]. Iyer S, Weiss C, Mehta A. Effects of drill speed on heat production and the rate and quality of bone formation in dental implant osteotomies. Part I: Relationship between drill speed and heat production. Int J Prosthodont. 1997; 10:411–414. Pubmed PMID:9495159.
[19]. Iyer S, Weiss C, Mehta A. Effects of drill speed on heat production and the rate and quality of bone formation in dental implant osteotomies. Part II: Relationship between drill speed and healing. Int J Prosthodont., 1997; 10:536–540. Pubmed PMID:9495174.
[20]. Tehemar S. Factors affecting heat generation during implant site preparation: a review of biologic observations and future considerations. Int J Oral MaxillofacImplants., 1999; 14:127–136. Pubmed PMID:10074763.
[21]. Garg AK. The use of osteotomes: a viable alternative to traditional drilling. Dent Implantol Update. 2002; 13:33-40. Pubmed PMID:12060956.
[22]. Saadoun AP, Le Gall MG.Implant site preparation with osteotomes: principles and clinical application. Pract Periodontics Aesthet Dent. Jun-Jul 1996;8(5):453-63.Pubmed PMID:9028267.
[23]. Yin XM, Dai JX, Wang XH, Xu DC, Zhong SZ. Observation of blood supplies system to mandible in transparent specimen. Shanghai kouqiangyixue= Shanghai journal of stomatology. 2003 Aug 1;12(4):266-8.
[24]. Hahn J. Clinical uses of osteotomes. Journal of Oral Implantology. 1999 Jan;25(1):23-9.