Computerised Tomographic Evaluation of Structural Variations in Sinonasal Region and its Clinical Correlation
Sahu A1*, Mukherjee SN2, Rabin S3, Praneeth K1, Sahu V4, Kavita G5
1 Pursuing DNB ENT, Department of ENT and HNS, downtown hospital, Guwahati, Assam, India.
2 Senior consultant, Department of ENT and HNS, downtown hospital, Guwahati, Assam, India.
3 Senior consultant, Department of radiology, downtown hospital, Guwahati, Assam, India.
4 Assistant professor, Department of oral & maxillofacial surgery, Government dental college and hospital, Nagpur, India.
5 Consultant Oral & maxillofacial surgeon, Nagpur, India.
*Corresponding Author
Abhishek V Sahu,
Department of ENT and HNS, downtown hospital,
Guwahati, Assam, India.
E-mail: sahuabhishekngp@gmail.com
Received: July 11, 2017; Accepted: August 17, 2017; Published: August 24, 2017
Citation: Sahu A, Mukherjee SN, Rabin S, Praneeth K, Sahu V, Kavita G. Computerised Tomographic Evaluation of Structural Variations in Sinonasal Region and its Clinical Correlation. Int J Clin Exp Otolaryngol. 2017;3(5):78-86. doi: dx.doi.org/10.19070/2572-732X-1700015
Copyright: Sahu A©2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: The endonasal as well as paranasal anatomy is highly variable and can encroach upon the osteomeatal complex and narrow the osteomeatal channels.
Aims And Objectives: To study on CT scan, the incidence of structural variations in sinonasal region and its correlation with sinusitis.
Material And Methods: It’s a cross sectional study on 106 cases done over 1 year.
Results And Observations: On the basis of clinical diagnosis chronic sinusitis was seen in 90 (84.9%) cases and gross polyposis in 16 (15.1%) cases. CT scan anatomical variations seen were as follows: Concha bullosa 64 (60.37%), aggernasi cell in 58 (54.7%), PMT in 28 (26.41%), Large ethmoidal bulla in 18 (16.98%), uncinate pneumatization in 12 (11.3%), haller cell in 18 (16.98%) and onodi cell in 12 (11.35 %) cases. Maxillary sinus was most commonly involved in 90 (84.9%) cases and least common involved was sphenoid sinus in 14 (13.2%) cases. Among the 5 different patterns of CRS on CT scan most common was OMC pattern noted in 32 (30.18%) cases followed by infundibular pattern in 31 (29.24%), sporadic or unclassified unit pattern in 25 (23.58%), sinonasal polyposis in 10 (9.43%) cases and SER pattern in 08 (7.54%) cases.
Conclusion: Rhinosinusitis commonly affects working population with female preponderance. Anatomical variation is observed to be one of the predominant causes for OMC block as well as sinusitis and CT is the paramount modality to study and analyze them.
2.Introduction
3.Materials and Methods
4.Results and Observations
5.Discussion
6.Conclusion
7.Acknowledgement And Declarations
8.References
Keywords
Computed Tomography (CT); Paradoxical Middle Turbinate (PMT); Osteo-Meatal Complex (OMC); Spheno-Ethmoidal Recess (SER).
Introduction
Human beings are individualistic and this is reflected in their anatomy, which is subject to a large number of anatomical variations. The endonasal as well as paranasal anatomy is highly variable [1] and the variations like septal deviations, concha bullosa, aggernasi, PMT, pneumatized uncinate etc. can encroach upon the OMC and narrow their channels [2]. This leads to impaired drainage and ventilation of the paranasal sinuses which primarily cause sinusitis.
Stammberger and Hawke in 1993 have shown that CT scan of PNS provide a road map to identify significant anatomic abnormalities, exact location of obstruction and severity of the disease [3]. It has the ability to optimally display bone, soft tissue and air. It provides an accurate description of both anatomy and extent of disease in and around PNS. CT scan is gold standard investigation for CRS diagnosis [4].
1. To study on CT scan, the incidence of structural variations in sinonasal region.
2. To study the correlation between sinonasal anatomical variations and sinusitis.
3. To compare the results of this study with the results of the previous workers.
Material and Methods
Study Area: ENT department, down town Hospital, Guwahati, Assam.
Study Population: Patients fulfilling the inclusion criteria and attending the ENT OPD and IPD of downtown hospital were included in the study.
Study Design: Cross Sectional Study.
Sample Size: 106 cases.
Sample Period: 1 year from 4th December 2015 to 3rd December 2016.
• Chronic Rhinosinusitis diagnosed as per the criteria by AAOHNS Task Force 1997
• Patients more than 12 years of age
• Septal pathologies like DNS
• Sinonasal polyposis
• Nasal obstruction due to different causes like anatomical variation
• Headache due to nasal pathology
• Acute and Subacute Rhinosinusitis
• Patients less than 12 years age
• Septal pathologies like abscess, hematoma and perforation
• Facial trauma and fracture nasal bone
• Sinonasal malignancies
• Previous nasal surgeries
• Granulomatous nasal conditions
• Fungal nasal diseases
• Complicated sinusitis
• Known disorder of ciliary motility like immotile ciliary syndrome, Kartageners syndrome, Down syndrome and cystic fibrosis
• Those not willing for CT scan
During a 1-year period, a total of 106 cases were evaluated who had attended the OPD or IPD of ENT, downtown hospital, Guwahati, Assam. The patient’s clinical features were noted as per AAO-HNS Taskforce 1997 parameters into major and minor. 2 major factors or 1 major factor and 2 minor factors constitute a strong history for CRS.
A thorough clinical examination was done and the diagnosis of rhinosinusitis was established. All the patients in acute phase of the disease were treated conservatively with a course of antibiotics, topical and oral decongestants, antihistaminics and steroids. The patients who returned for follow up were again clinically evaluated for subjective relief in symptoms and objectively by thorough clinical examination. The patients with persistent symptoms and signs were counseled regarding imaging of nose and PNS by CT scan and also about the need for further endoscopic evaluation and surgery.
Written informed consent was taken and data regarding the patient was collected in a case proforma as per annexure.
Before undergoing CT scan, the patient was instructed to clean their noses by blowing out any secretions and/or suction clearance of the nose and PNS was done. CT scan was done using a 16 slice CT machine.
Supine position with head extended. In patients in whom head extension was contraindicated due to cervical spondylosis, gantry tilt was suitably adjusted.
In the coronal study, taking hard palate as reference axis, the plane of section was perpendicular to this structure. Direct scans 3 mm in thickness were made, from the anterior walls of the frontal sinuses (nasion) to the posterior wall of the sphenoid sinus. 0.6 mm high resolution coronal and axial scans were then reconstructed and reviewed.
120 kV, 80 mA with 23 second scan time, window width of 2500 to 3000 HU.
Pattern of disease on CT scan was noted as described by Sonken et al., (1991) and includes:
1. Infundibular pattern
2. Osteomeatal complex pattern
3. Sphenoethmoid recess pattern
4. Sinonasal polyposis pattern
5. Sporadic (unclassifiable) pattern
The data was processed using Microsoft Excel software. For statistical analysis of the data showing relationship of anatomical variation and presence of sinusitis, χ2 test was used as tests for significance. The statistical analysis was done using SPSS-16 software.
Results and Observations
Present study included 106 patients of which 90 (84.9%) cases were of chronic rhinosinusitis and 16 (15.1%) of gross polyposis on clinical examination. Maximum patients i.e. 42 (39.62%) cases were of 21-30 years age group followed by 28 (26.4%) cases between 31-40 years. Youngest patient was 13 years old and eldest was 68 years old. We found a female preponderance with a ratio of 1.52:1.
Various clinical features presented by all patients were categorized into major and minor factors as per task force 1997. Among major factors, most common was nasal obstruction seen in 96(86.7%) cases, followed by nasal discharge in 84(79.2%) cases, least common was hyposmia or anosmia seen in 16(15.09%) cases. In minor factors, headache was the most common presenting factor seen in 74(69.81%) cases, followed by fatigue in 34(32%) cases and fever in 24(22.6%) cases. Least common among the minor factors was halitosis seen in 14(13.2%) cases.
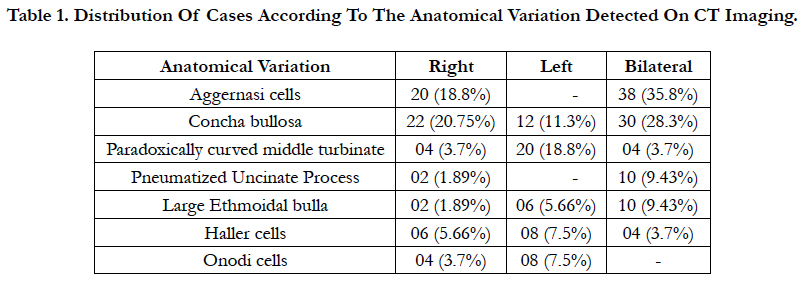
In present study most common septal variation was septal deviation seen in 88 (83%) cases and more towards left side in 52 (62.5%) cases. Severe type of septal deviation was most common, seen in 46 (43.3%) cases of which 24 (22.6%) were to left and 22 (20.7%) to right followed by moderate septal deviation in 30 (28.3%) cases and mild in 12 (11.3%) cases. Septal deviation with spur is seen in 40 cases (37.73%) of which 24 were on left side and 16 on right side. Septal pneumatization is seen in 50 (47.1%) cases. (Table 1)
In present study we noted presence of aggernasi cells in 58 (54.7%) cases, of which 20 (18.8%) were on right side & 38 (35.8%) had bilateral. Concha bullosa was seen in 64 (60.37%) cases. It was bilateral in 30 (28.3%) cases, on right side in 22 (20.75 %) cases and on left side in 12 (11.3 %) cases.
Paradoxically curved middle turbinate was reported in 28 (26.41%) cases which included 20 (18.8%) cases on the left side, 4 (3.7%) cases on the right side and bilaterally in 4(3.7%) cases. Uncinate pneumatization was seen in 12 (11.3%) cases, 10 (9.43%) cases of which were bilateral and only 2 (1.89%) cases were to right side.
Ethmoid bulla was seen to be enlarged in 18 (16.98%) cases. It was encountered bilaterally in 10 (9.4%) cases, on the left side in 06 (5.6%) cases and on the right side in 02 (1.89%) cases. Haller cells were found in 18 (16.98%) cases, mainly on left side in 08 (7.5%) cases followed by 06 (5.66%) cases on right side and 04 (3.7%) cases on both sides. Onodi cells were seen in 12 (11.35%) cases of which 08 (7.5%) cases had it on left side and 04 cases had it on right side.
In present study we found concha bullosa in 64 (60.3%) cases of which most common was lamellar type seen in 40 (37.73%) cases that was bilateral in 18 (16.98%) cases and unilateral in 22 (20.75%) cases. This was followed by bulbous and extensive type seen in 12 (11.32%) cases each and both types were bilateral in 06 (5.67%) cases and unilateral in 06 (5.67%) cases.
In present study we found superior attachment of UP mainly to lamina papyracea in 70 (66%) cases on left side and 48 (45.2%) on right side. This was followed by attachment to middle turbinate in 40 (37.2%) cases on right and 28 (26.4%) cases on left. Attachment to skull base was seen in 18 (16.9%) cases on right and 08 (7.54%) cases on left.
In present study, frontal cells were seen in 30(28.30%) cases where type I is most commonly seen in 16 (53.3%) cases followed by type II in 8 (26.6%) cases, type III in 04 (13.3%) cases and least common type IV in only 02 (6.6%) cases.
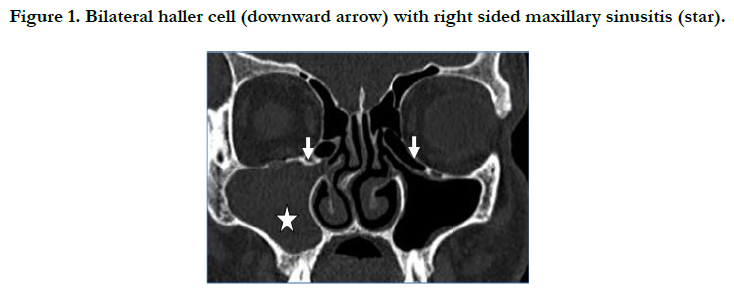
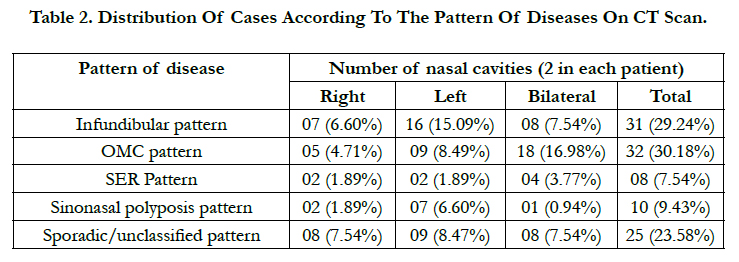
In present study, we found sinus opacification as most common in maxillary sinuses in 90 (84.9%) cases followed by anterior ethmoidal air cells in 54 (50.94%) cases and frontal sinus in 20 (18.9%). Posterior ethmoid sinuses were opacified in 16 (15.09%) cases and sphenoid sinus in 14 (13.2%) cases being the least common. (Figure 1, Table 2)
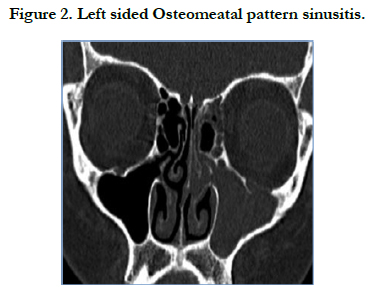
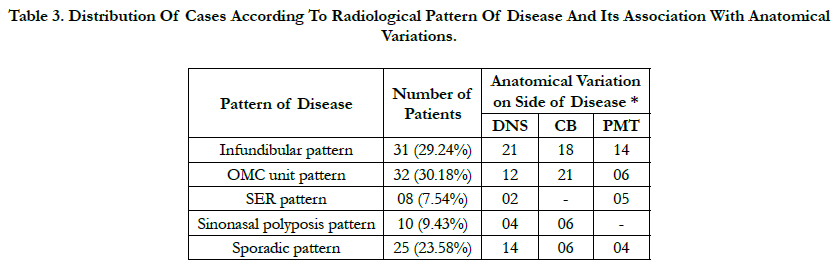
In present study of 106 patients we have noted different patterns of disease on CT imaging as described by Sonken et al., (1991). OMC pattern of disease was most commonly noted in 32 (30.18%) cases followed by Infundibular pattern in 31 (29.24%) cases and sporadic/unclassified in 25 (23.58%) cases, sinonasal polyposis pattern was seen in 10 (9.43%) cases and least common was SER pattern noted in 08 (7.54%). (Figure 2, Table 3)
Table 3. Distribution Of Cases According To Radiological Pattern Of Disease And Its Association With Anatomical Variations.
In present study we found infundibular pattern was associated with septal deviation on same side of disease in 21 (67.74%) cases, concha bullosa in 18 (58.06%) cases and PMT in 14 (45.16%) cases.
In OMC pattern, septal deviation was noted in 12 (37.5%), concha bullosa in 21 (65.62%) and PMT in 6 (18.75%) cases on same side of disease. In SER pattern, septal deviation was seen in 2 (25%) and PMT in 5 (62.5%) cases on same side of disease. In sinonasal polyposis pattern, septal deviation was seen in 4 (40%) and concha bullosa in 6 (60%) cases on same side of disease. Sporadic pattern of disease was associated with septal deviation in 14 (56%), concha bullosa in 6 (24%) and PMT in 4 (16%) cases on same side of disease.
In present study, we found left sided septal deviation was associated with right sided concha bullosa in 14 cases and right side septal deviation with left sided concha bullosa in 7 cases. Septal deviation with concha bullosa on same side was found in 9 cases. But there was no significant association between side of septal deviation and presence of concha bullosa on contralateral side [P = 0.25 which is not significant because P > 0.05].
In present study we found septal deviation in 88 (83%) cases where moderate septal deviation was more frequently associated with sinusitis on same side in 21 (70%) cases. Among severe septal deviations, we found sinusitis on the same side in 26 (56.52&) cases and among mild septal deviations in 6 (50%) cases. We found significant association of moderate septal deviation with sinusitis [chi-square test x2 = 4.8, DF= 1, P = 0.02].
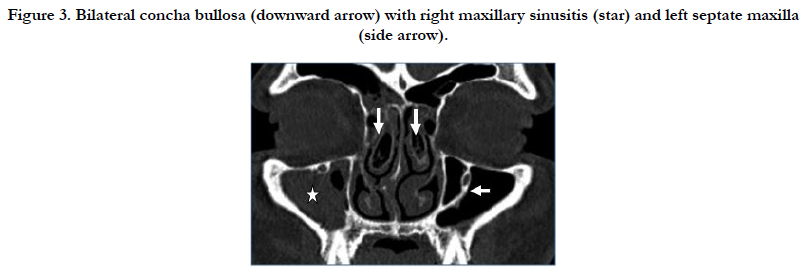
In this study, we found concha bullosa in 64 (60.3%) cases of which 40 (37.73%) were lamellar and 25 (62.5%) of those were seen on side of disease. Bulbous and extensive types were seen in 12 (11.32%) cases each. 5 cases in the bulbous concha and 8 cases in extensive concha were associated with sinusitis on same side. There was no significant association between the type of concha bullosa and sinusitis on same side of disease [P > 0.05] (Figure 3).
Figure 3. Bilateral concha bullosa (downward arrow) with right maxillary sinusitis (star) and left septate maxilla (side arrow).
Discussion
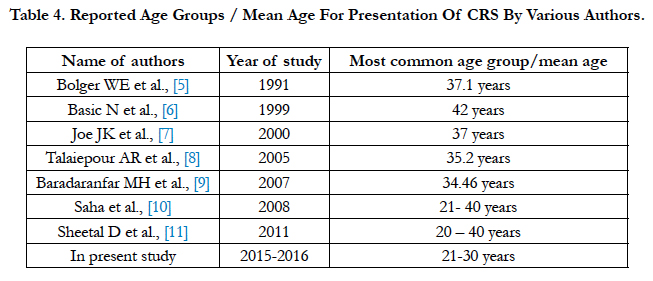
In present study out of 106 cases, maximum patients were between the age group of 21- 30 years i.e. 42 (39.62%) cases followed by 28 (26.4%) cases in 31-40 year age group. The findings in the present study correlate well with the other studies listed below having most of their presentation in the same age group. This is the most active age group and comprises the most productive age group of society (Table 4).
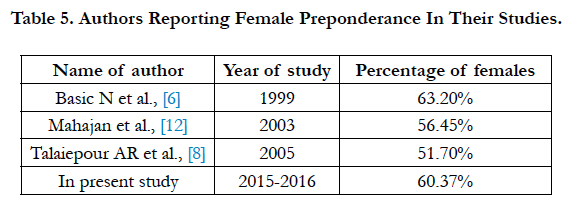
In present study we found female preponderance in cases of CRS with ratio of 1.52:1 which correlate well with the other studies listed below. It was reported that female dominance was due to hormonal changes that occurs during puberty, pregnancy, menstruation and sexual excitement due to vasomotor imbalance leading to frequent sinusitis. (Table 5)
Present study included 106 patients where 90 (84.9%) chronic sinusitis and 16 (15.1%) gross polyposis cases found on clinical examination, while study conducted by Jones et al (1997) had 75% CRS and 25% diffuse polyposis [13].
The most common major symptom seen in the present study is nasal obstruction in 96 (86.7%) cases, followed by nasal discharge/ post nasal drip in 84 (79.2%) cases. Least common presenting symptom was hyposmia or anosmia seen in 16 (15.09%) cases. In minor symptoms, most common was headache seen in 74 (69.81%) cases, followed by fatigue in 34 (32%) cases and fever in 24 (22.6%) cases. Least common symptom among the minor factors was halitosis in 14 (13.2%) cases.
Rohit Saxena et al., (2010) studied 60 patients of CRS and reported post nasal drip as most common major symptom seen in 46 (76.7%) cases followed by nasal obstruction in 43 (71.7%) cases. Among minor symptoms headache was seen in 36 (60%) cases followed by cough in 20 (33.3%) and earache in 8 (13.3%) cases [14]. In present study most common septal variation was septal deviation seen in 88 (83%) cases, more common on left side 52 (62.5%) cases and right side seen in 36 (33.96%) cases. Mamatha in 2010 in his study showed the prevalence of DNS ranging from 14.1% to 80% [15] as reported by other workers: Dutra and Marchiori 14.1%; Kinusi et al. 23.3%; Arslan et al. 36%; Asruddin 38% ; Earwaker 44%; Maru 55.7% and Pinas P et al., 80%. In other studies, these findings are Zinreich SJ et al., (1988) [16] 21%, Bolger WE et al., (1991) [5] 18.8%, Jareoncharsri et al., (1999) [17] 72.33% cases and Talaiepour AR et al., (2005) [8] 63% cases. Our results of septal deviation are comparable to higher range reported.
In present study we have classified septal deviation depending upon the severity of deviation as mild, moderate and severe [18]. We found severe type of septal deviation as most common in 46 (43.3%) cases, moderate in 30 (28.3%) cases and mild in 12 (11.3%) cases. Septal deviation with spur is seen in 40 cases of which 24 were on left side and 16 on right side. The prevalence of septal spur in our study was 37.73% and as reported by Danese et al., [19] is 33% and by Jareoncharsri et al., [17] is 25.3%. In present study septal pneumatization is seen in 50 (47.1%) cases which are higher than those reported by Wang RG et al., (2003) in 18% cases [20] and Chao TK (2005) in 2% cases [21].
Aggernasi cells were seen in total 58 (54.7%) cases of which 20 (18.8%) had prominent aggernasi on right side & 38 (35.8%) had bilateral aggernasi. These findings correlates with studies of Talaiepour AR et al., (2005) [8] and Baradaranfar MH et al., (2006) [9] which reported the prevalence as 56 % and 36% respectively.
In present study, concha bullosa was seen in 64 (60.37%) cases that was bilateral in 30 (28.3), only right side in 22 (20.75%) and only left side in 12 (11.3%). The prevalence in our study correlates well with those reported by Bolger WE et al., [5] (1991) as 53%, John Earwaker (1993) [22] as 55% and Perez P et al., (2000) 73% [23].
Paradoxically curved middle turbinate was reported in 28 (26.41%) cases which included 20 (18.8%) cases on left side and 4 (3.7%) cases each on right side and bilaterally. These correlated well with study conducted by Bolger WE et al., (1991) who reported PMT in 26.1 % cases 5; Hosemann WG et al., (2000) [24] in 24% and RohitSaxena et al., (2010) 14 in 32%.
In our study, uncinate pneumatization was seen in 12 (11.3%) cases of which 10 (9.43%) were bilateral and only 02 (1.89%) were on the right side. These findings correlated to Lloyd GAS et al (1991) who reported 16 % cases of uncinate pnuematization [25].
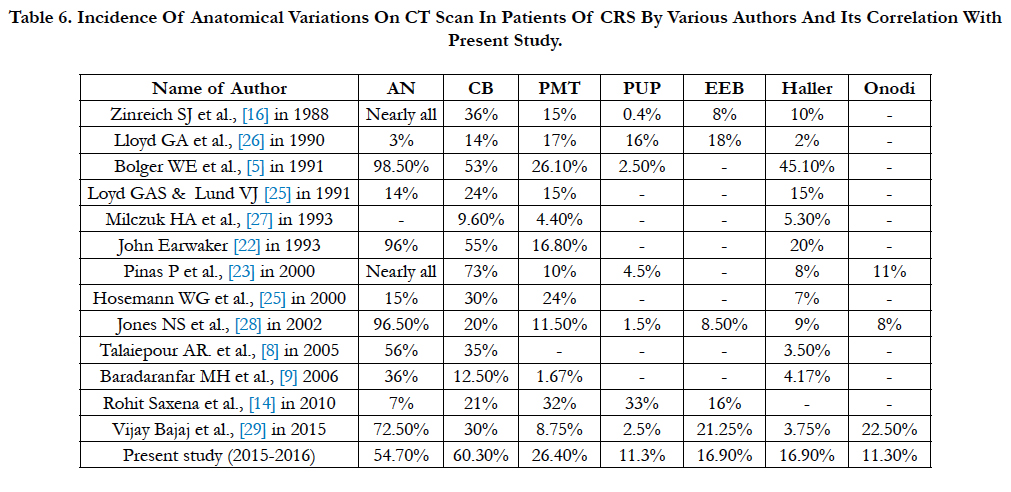
Ethmoid bulla was seen to be enlarged in 18 (16.98%) cases where it was bilateral in 10 (9.4%), only left side in 6 (5.6%) and only right side in 2 (1.89%). Incidence in present study correlated with the study of Lloyd GAS et al., [25] (1991) who reported enlarged ethmoid bulla in 18% and RohitSaxena et al., [14] (2009) in 16%. (Table 6)
Table 6. Incidence Of Anatomical Variations On Ct Scan In Patients Of Crs By Various Authors And Its Correlation With Present Study.
Haller cells were found in 18 (16.98%) cases. These findings correlated with other studies such as 10% in Zinreich SJ et al (1988) [16], 8% in Pinas P et al., (2000) [23], 7% in Hosemann WG et al., (2000)24 and 9% in Jones NS et al (2002) [28].
Onodi cells were seen in 12 (11.35%) cases which correlated well with other studies. Pinas P et al., in 2000 studied CT of 110 patients suspected of inflammatory disease and reported onodi cells in 11% cases [23].
In present study, superior attachment of UP found mainly to lamina papyracea in 70 (66%) cases on left side and 48 (45.2%) on right side. This was followed by attachment to middle turbinate seen in 40 (37.2%) cases on right and 28 (26.4%) on left. Attachment to skull base was seen in 18 (16.9%) cases on right and 08 (7.54%) on left.
Sheetal D et al., (2011) also reported superior attachment of UP most commonly to lamina papyracea (70% on right side and 66% on left side) followed by the middle turbinate (24% on right and 31% on left side) [11].
In present study we have found the most common appearance of frontal cell type I seen in 16 (15.9%) cases followed by type II in 8 (7.5%) cases, type III in 4 (3.7%) and type IV in only 2 (1.8%) cases.
Meyer TK et al., studied 768 scans and found type I frontal cells in 14.9% cases, type II in 1.3%, type III in 1.7% and type IV in 2.1% [30]. Del Gaudio JM et al., (2005) studied 106 CT PNS and found type I frontal cells most common in 18.1% followed by type III in 6.1%, type IV in 2.4% and type II in 1.4% cases [31]. Finding of our study correlated well with those studies.
In present study, we found 94 concha bullosa in 64 (60.3%) cases. Lamellar concha was most commonly seen in 40 (37.73%) cases, bulbous and extensive concha bullosa seen in 12 (11.32%) cases each. In 1991, Bolger WE et al., studied 202 patients and found lamellar concha in 46.2% cases, bulbous concha in 31.2% cases and extensive i.e. true concha bullosa in 15.7% cases [5]. Uygur T et al., in 2003 studied 100 consecutive patients of chronic sinusitis and found lamellar concha 55.3%, bulbous in 33.97% and extensive in 10.8% cases [32].
Keles et al., in 2010 studied 90 patients of concha bullosa and found lamellar concha in 14.3% cases, 30% cases of bulbous concha and 44.4% cases were extensive or true concha bullosa [33]. The incidence of appearance of lamellar concha in present study correlated with Bolger WE et al., (1991) and Uygur et al., (2003).
In present study we found septal deviation and concha bullosa related to each other in its appearance. Concha bullosa with septal deviation on opposite side was found in 21 cases and on same side was found in 9 cases. But there was no significant association between side of septal deviation and presence of concha bullosa on contralateral side [P = 0.25 which is not significant because P> 0.05].
The study conducted by Stallman et al., (2002) found significant association between the septal deviation and concha bullosa. They found that in patients with left sided unilateral concha, 117 (70%) cases had right sided nasal septal deviation, 11 (7%) cases had left sided nasal septal deviation and 38 (23%) cases had no septal deviation [34].
Keles et al., (2010) evaluated relationship between nasal septal deviation and concha bullosa and reported that concha occurs more frequently on the opposite side of septal deviation (50%) than to the side of septal deviation (17.8%) cases [33]. Thus our findings correlates well with finding reported by Stallman et al. and Keles et al.,
In present study we found most common sinus involved was maxillary, seen in 90 (84.9%) cases followed by anterior ethmoids in 54 (50.94%), frontal in 20 (18.9%) and posterior ethmoids in 16 (15.09%). Least common involved sinus was sphenoid in 14 (13.2%) cases.
Calhoun et al., (1991) studied coronal CT sinus of 82 patients and found maxillary to be most commonly involved in 43% cases followed by anterior ethmoids in 34% and frontal sinus least [35].
Rohit Saxena et al., (2010) in his study of 60 cases found anterior ethmoids most commonly involved in 31 (51.7%) followed by maxillary in 29 (48.3%) cases [14]. Our findings correlated with Calhoun et al and RohitSaxena et al in involvement of sinuses.
In present study, OMC pattern was most commonly noted in 32 (30.18%) cases followed by infundibular pattern in 31 (29.24%), sporadic or unclassified unit pattern in 25 (23.58%), sinonasal polyposis in 10 (9.43%) and SER pattern in 8 (7.54%) cases.
Sonkens et al., (1991) in 500 patients reported 26% infundibular pattern, 25% OMC pattern, 6% SER pattern, 10% sinonasal polyposis and in 24% cases, sporadic pattern [36].
Lerdlum S et al., in 2005 evaluated screening sinus CT of 133 patients with inflammatory sinus disease and found that pattern I to be most common pattern of inflammatory disease (33.1%) followed by pattern II in 25.6%, pattern III in 24.4%, pattern IV in 10.5% and pattern V in 19.9% [37].
Naimi M et al., in 2006 studied 200 coronal CT scans and reported OMC pattern as most common in 34% cases followed by sporadic pattern in 32%, SER pattern in 24%, sinonasal polyposis pattern 16% and least common infundibular pattern in 6% [38].
Eggesbo in 2006 studied patients undergoing sinonasal CT for suspected inflammatory sinonasal disease and reported infundibular and OMC patterns as most common (25% each). The SER and sinonasal polyposis patterns are less common, and each is found in less than 10%. The sporadic pattern is reported in 24% [39]. Our findings correlates well with these studies.
In the present study in bilateral cases of sinusitis presence of anatomical variation on each side was considered separately. OMC pattern was seen in 32 (30.18%) cases which was associated with nasal septal deviation seen in 12, concha bullosa in 21 and PMT in 6 cases on same side of disease.
Infundibular pattern was seen in 31 (29.24%) cases which were associated with deviated nasal septum in 21, concha bullosa in 18 and PMT in 14 cases on same side of disease. Out of 25 (23.58%) cases of sporadic pattern, 14 cases were associated with nasal septal deviation, 6 cases with concha bullosa and 4 cases with PMT on same side of disease.
In 10 (9.43%) cases of sinonasal polyposis pattern, we found septal deviation in 4 cases and concha bullosa in 6 cases, on same side of disease. In least common sphenoethmoidal recess pattern, we found 2 cases of septal deviation and 5 cases of PMT on same side of disease. OMC, infundibular and sporadic pattern were frequently associated with anatomical variation on same side.
Lerdlum S et al., (2005) studied 133 patients with inflammatory sinus disease and found that OMC pattern was associated with concha bullosa in 10 cases, infundibular pattern was associated with haller cells while aggernasi cells was associated with nasofrontal duct pattern [37].
Out of 12 cases of mild septal deviation, 6 (50%) cases were associated with sinusitis on same side. Out of 30 cases of moderate septal deviation, 21 (70%) cases were associated with sinusitis on same side. Severe septal deviation was seen in 46 cases and in 26 (56.52%) cases, it was associated with sinusitis on same side. The finding in this study shows strong association between moderate septal deviation and sinusitis on same side which was statistically significant [Chi-square test x2 = 4.8, DF= 1, P < 0.02].
In present study we found lamellar concha bullosa in 40 (37.73%) cases, bulbous concha bullosa in 12 (11.32%) cases and extensive concha bullosa in 12 (11.32%) cases. 62.5% (25 out of 40) cases of lamellar concha, 41% (5 out of 12) cases of bulbous concha and 66.66% (8 out of 12) cases of extensive concha were associated with disease on the side of concha. There was no significant association between the type of concha bullosa and sinusitis on same side of disease [P > 0.05].
In 2005, Hatipoglu et al., found no significant difference between the type of concha and association of sinusitis on same side. They found sinusitis on same side in 58.34% lamellar concha, 81% extensive concha and 37% bulbous concha [40].
Conclusion
Rhinosinusitis commonly affects the working population with female preponderance. Anatomical variation is observed to be one of the predominant etiologies for osteomeatal complex block as well as sinusitis. Computed tomography is the paramount modality to study and analyze these anatomical variations.
There is a significant association of moderate septal deviation with sinusitis and no association of any single type of concha with sinusitis. Though anatomical variations are important in pathogenesis of sinusitis, their association could not be statistically proven.
Acknowledgement And Declarations
We would like to thank Dr. N.N. Dutta, CMD of downtown hospital for supporting us. We would also like to confirm that there are no conflicts of interest.
References
- Stammberger H. Functional Endoscopic Sinus Surgery: The Messerklinger Technique. 1988;134(3)-23.
- Stammberger H, Wolf G. Headaches and sinus diseases: The endoscopic approach. Ann OtolRhinolLaryngol Suppl. 1997;134:3-23.PubMed PMID:3140703.
- Komisar A. Nasal obstruction due to benign and malignant neoplasm. OtolaryngolClin North Am. 1989;22(2):351-65.PubMed PMID: 2664656.
- Tondon PL, Gulati J, Mehta N. Histological study of polypoidal lesions in nasal cavity. N. Ind. J. Otol. 1971September;23(1):3-11.
- Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony an anatomic variation and mucosal abnormalities: CT analysis of endoscopic sinus surgery. Laryngoscope 1991;101(1 Pt 1):56-64.PubMed PMID:1984551.
- Basic N, Basic V, Jukic T, Basic M, Jelic M, Hat J. Computed et al. Computed tomographic imaging to determine the frequency of anatomical variations in pneumatization of the ethmoid bone. Eur Arch Otorhinolaryngol. 1999;256(2):69-71. PubMed PMID: 10068893.
- Joe JK, Ho SY, Yanagisawa E. Documentation of variations in sinonasal anatomy by intra-operative nasal endoscopy.Laryngoscope.2000Feb;110(2 Pt1):229-35. PubMed PMID: 10680921
- Talaiepour AR, Sazgar AA, Baghe A. Anatomic Variations of the Paranasal Sinuses on CT scan Images. Journal of Dentistry, Tehran University of Medical Sciences. 2005;2(4):142-146.
- Baradaranfar MH, Labibi M. Anatomic variations of paranasal sinuses in patients with chronic sinusitis and their correlation with CT scan staging. ActaMedicaIranica 2007;45(6):77-480.
- Saha KL, Taous A, MdRahman Z. Functional endoscopic sinus surgery for the management of sinonasal diseases. Bangladesh Journal of Otorhinolaryngology 2008;14(2):46-50.
- Sheetal D, Devan P P, Manjunath P, Martin P, Satish Kumar K, Sreekantha, et al.– Do We Really Require Before Fess? Journal of Clinical and Diagnostic Research. 2011 Apr5(2):179-181.
- Mahajan SB, Kochhar LK, Gupta AK. Sinugenic Headache and Nasal Endoscopy. Med J Armed Forces India2003 April59(2):121–124.PubMed PMID: 27407484.
- Rowe-Jones JM, Shembekar M, Trendell-Smith N, Mackay IS. Polypoidal rhinosinusitis in cystic fibrosis: A clinical and histopathological study. ClinOtolaryngol Allied Sci. 1997;22(2):167-171.PubMed PMID: 9160933.
- Saxena R, Vivek K, Mohit S. Role of CT paranasal sinuses and diagnostic nasal endoscopy inthe treatment modification of chronic rhinosinusitis. Gujarat Journal of Otorhinolaryngology and Head& Neck Surgery 2010 June-July7(1):7.
- Mamatha H, Shamasundar NM, Bharathi MB, Prasanna LC. Variations of osteomeatal complex and its applied anatomy: A CT scan study. Indian Journal of Science and Technology 2010 Aug3(8):904-907.
- Zinreich SJ, Kennedy DW, Rosenbaum AE, Gayler BW, Kumar AJ, Stammberger HParanasal sinuses: CT imaging requirements for endoscopic surgery. Radiology 1987;163(3):769-75. PubMed PMID:3575731
- Jareoncharsri P, Thitadilok V, Bunnag C, UngkanontK, Voraprayoon S, Tansuriyawong P Nasal endoscopic findings in patients with perennial allergic rhinitis. Asian Pac J Allergy Immunology. 1999 December 17(4): 261-7.
- Janardhan Rao J, Vinay Kumar E. C, Ram Babu K, SathavahanaChowdary V, Jaswinder Singh, VineetaRangamani S.Classification of nasal septal deviation- relations to sinonasal pathology. Indian Journal of Otolaryngology and Head Neck Surgery 2005 July- September 57(3): 199-201.
- Danese M, Duvoisin B, Agrifoglio A, Cherpillod J, Krayenbuhl M. Influence of naso-sinusal anatomic variants on recurrent, persistent or chronic sinusitis. X-ray computed tomographic evaluation in 112 patients. J Radiology. 1997 September78(9):651-7. PubMed PMID: 9537184.
- Wang RG, Zou YH, Han DY, Zhang W. Pneumatization of perpendicular plate of the ethmoid bone and mucocele. ZhonghuaEr Bi Yan HouKeZaZhi2003August38( 4):279-81. PubMed PMID: 14743638.
- Chao TK. Uncommon anatomic variations in patients with chronic paranasal sinusitis. Otolaryngol Head Neck Surg2005 February 132(2):221-5. PubMed PMID: 15692530.
- Earwaker J. Anatomic variants in sinonasal CT. Radiographics 1993;13(1):381-415.PubMed PMID: 8460226.
- Pinas P, Sabate J, Carmona A, Catalina C J, Jimenez J. Anatomical variations in the human paranasal sinus region studied by CT. J Anat2000;197:221- 227.PubMed PMID: 11005714.
- Hosemann WG, Weber RK, Keerl RE, Lund VJ. Minimally Invasive Endonasal Sinus Surgery,Thieme, Stuttgart, New York. 2000; 3.
- Lloyd GAS, Lund VJ, Scadding GK. CT of the paranasal sinuses and functional endoscopic surgery: a critical analysis of 100 symptomatic patients. J LaryngolOtol1991;105 (3):181-185. PubMed PMID: 2019802
- Lloyd GA. CT of the paranasal sinuses: study of a control series in relation to endoscopic sinus surgery. J LaryngolOtol1990;104 (6):477-481.PubMed PMID: 2376707.
- Milczuk HA, Dalley RW, Wessbacher FW, Richardson MA. Nasal and paranasal sinus anomalies in children with chronic sinusitis. Laryngoscope 1993Mar103(3):247-52.PubMed PMID: 8441311.
- Jones NS. CT of the paranasal sinuses: A review of the correlation with clinical, surgical and histopathological findings. ClinOtolaryngol Allied Sci. 2002Feb27(1):11-7.PubMed PMID:11903365.
- Vijay B, Bhoopendra S, Purohit JP. Prevelance of anatomical variations of lateral wall of nose in chronic sinusitis patients. Journal of Evolution of Medicine and Dental Sciences2015April32(4):5492-5505.
- Meyer TK, Kocak M, Smith MM, Smith TL. Coronal computed tomography analysis of frontal cells. American Journal of Rhinology and allergy 2003May-June17(3)163-8.
- Del Gaudio JM, Hudgins PA, Venkatraman G, Beningfield A. Multiplanar computed tomographic analysis of frontal recess cells: effect on frontal isthmus size and frontal sinusitis. Arch Otolaryngol Head Neck Surg. 2005Mar131(3):230-5.PubMed PMID: 15781763.
- Uygur K, Tüz M, Doğru H. The correlation between septal deviation and concha bullosa. Otolaryngol Head Neck Surg2003;129(1):33-36.PubMed PMID: 12869913.
- BaharKeleş, KayhanÖztürk, DenizÜnaldı, HamdiArbağ, BedriÖzer. Is There any Relationship Between Nasal Septal Deviation and Concha Bullosa? European Journal of General Medicine 2010;7(4):359-364.
- Jamie S Stallman, Joao N Lobo, Peter M Som. The Incidence of Concha Bullosa and Its Relationship to Nasal Septal Deviation and Paranasal Sinus Disease. American Journal of Neuroradiology October2004;25:1613-1618.
- Calhoun KH, Waggenspack GA, Simpson CB, Hokanson JA, Bailey BJ. CT evaluation of the paranasal sinuses in symptomatic and asymptomatic populations. Otolaryngol Head Neck Surg1991 April104(4):480-3.PubMed PMID:1903859
- Sonkens JW, Harnsberger HR, Blanch GM, Babbel RW, Hunt S. The impact of screening sinus CT on the planning of functional endoscopic sinus surgery. Otolaryngology Head Neck Surgery 1991December105(6):802-13.
- Lerdlum S, Vachiranubhap B. Prevalence of Anatomic Variations Demonstrated on Screening Sinus Computed Tomography and Clinical Correlation. J Med Assoc Thai 2005; 88(4):110-5. PubMed PMID:16623013.
- Naimi M, Bakhshaei M. The major obstructive inflammatory patterns of the sinonasal diseases in 200 candidates of functional endoscopic sinus surgery. The Iranian Journal of Otorhinolaryngology winter -2006;17(42):9-14.
- Eggesbø HB. Radiological imaging of inflammatory lesions in the nasal cavity and paranasal sinuses. European Radiology 2006April16(4):872-88.
- HaticeGülHatipoğlu, Mehmet Ali Çetin, EnisYükse. Concha bullosa types: their relationship with sinusitis, osteomeatal and frontal recess disease. Diagnostic and Intervention Radiology 2005;11(3):145-149.