Outcome Measurement Between Transtympanic and Tympanomeatal Flap Elevation Approach in Myringoplasty: A Day Care Procedure
Sahu A1*, Talukdar J2, Datta DJ2
1 Pursuing DNB ENT, Department of ENT and HNS, Downtown Hospital, Guwahati, Assam, India.
2 Senior Consultant, Department of ENT and HNS, Downtown Hospital, Guwahati, Assam, India.
*Corresponding Author
Abhishek Sahu,
Pursuing DNB ENT, Department of ENT and HNS,
Downtown Hospital, Guwahati, Assam – 781006, India.
E-mail: sahuabhishekngp@gmail.com
Received: November 19, 2016; Accepted: December 29, 2016; Published: December 30, 2016
Citation: Sahu A, Talukdar J, Datta DJ (2016) Outcome Measurement Between Transtympanic and Tympanomeatal Flap Elevation Approach in Myringoplasty: A Day Care Procedure. Int J Clin Exp Otolaryngol. 2(6), 51-55. doi: dx.doi.org/10.19070/2572-732X-1600010
Copyright: Sahu A© 2016. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Transtympanic myringoplasty is an alternate technique that allows graft placement medial to tympanic membrane remnant through the perforation without the need for tympanomeatal flap elevation.
Objectives: The aim of this study is to evaluate the efficacy and compare the results of transtympanic myringoplasty without tympanomeatal flap elevation with the usual method of graft placement by the elevation of a tympanomeatal flap.
Materials and Methods: This is a prospective study done on fifty patients divided into two groups, each consisting of 25 patients. Group I patients underwent transtympanic myringoplasty without elevation of tympanomeatal flap and group II patients underwent tympanomeatal flap elevation myringoplasty. Both the procedures were done by underlay technique through transcanal approach using only tragal perichondrium as graft material.
Results and Observations: Graft uptake was successful in 88% and 92% ears while hearing improvement was seen in 84% and 91.3% in the group I and II patients respectively. The mean hearing gain was 15.04 dB and 15.57 dB in group I and II respectively.
Conclusion: Transtympanic myringoplasty is a simple and less traumatic yet equally effective approach for the repair of tympanic membrane perforation. It has the added advantages of minimal post-operative pain, cost-effectiveness, no potential risk of injury to chorda tympani and results comparable to conventional techniques of myringoplasty.
2.Introduction
2.1. Need for Study
3.Material and Methods
3.1.Aims and Objectives
3.2.Inclusion Criteria
3.3.Exclusion Criteria
3.4.Procedure
4.Results
5.Discussion
6.Conclusion
7.References
Keywords
Transtympanic Myringoplasty; Tympanomeatal Flap; Underlay Technique; Tragal Perichondrium.
Introduction
Although repairing TM perforations has always been considered a straight forward procedure in otology [1], new approaches should be carefully evaluated to improve the quality of our services. Myringoplasty was described by Berthold in 1878 as a surgical procedure to close tympanic membrane perforations of many different causes [2]. The most widely accepted underlay technique of tympanomeatal flap elevation myringoplasty (TMM) was described by Austin and Shea in 1961 [3].
Transtympanic myringoplasty (TTM) is essentially an underlay technique and was proposed by Shea in 1960 [4]. It is an alternate technique that allows graft placement medial to tympanic membrane remnant through the perforation without the need for tympanomeatal flap elevation.
Published literature on transtympanic myringoplasty is spare, also all related work on this topic is done using temporalis fascia only and there is no related work done in this topic in the north east part of India.
The aim of this study is to evaluate the efficacy and compare the results of transtympanic myringoplasty without tympanomeatal flap elevation with the usual method of graft placement by the elevation of a tympanomeatal flap.
This is a prospective study done on fifty patients attending the ENT OPD in Downtown Hospital, Guwahati, Assam from July 2015 to June 2016. We randomized the patients into 2 almost identical groups by allotting them odd and even numbers such that patients with even numbers were in group I and patients with odd numbers were in group II and then compared their results accordingly. All patients were subjected to full history taking, general and local examination, including otoscopic ear examination. The local ethics committee approved the study protocol and informed consent was obtained from each patient.
Group I patients underwent TTM without elevation of the tympanomeatal flap and Group II patients underwent usual method of graft placement by TMM. We recorded the pure tone audiogram readings at 0.5, 1 and 2 kHz for all patients preoperatively and postoperatively and calculated the air-bone gap in all the cases. The mean gain in hearing was then evaluated for audiologic success. Pain score in the post operative period was calculated using visual analogue scale after an observation period of 4 hours.
Success in terms of closure of the perforation was defined as an intact eardrum at 12th week postoperatively and in terms of hearing gain was defined as an improvement in AC thresholds by 10 dB or more in comparison with the preoperative audiogram.
• Patients with small and medium size central perforation with more than 2 mm margin present to the edge of the perforation.
• Dry for more than 3 month
• Absence of ossicular or mastoid pathology (conductive hearing loss of less than 40 db)
• Wide external auditory canal with visible access to entire tympanic membrane.
• Patient aged between 18-45 years to remove age bias and tolerate local anaesthesia.
• Central perforation with ill-defined margins, margins adhesive to promontory or perforation with less than 2 mm margin present to the edge of the perforation.
• Actively discharging ear or dry perforation for less than 3 month.
• Large, subtotal, total, attic or marginal perforation.
• Patients with revision ear surgery.
• Suspected ossicular pathology with air bone gap of more than 40 dB.
• Otitis externa.
• Sensorineural or mixed HL.
All patients were operated under local anesthesia. Tragal perichondrium was used as the graft material in all the cases, the size of which was larger in diameter than of the size of perforation. Using transcanal approach and under microscopic vision the margins of the perforations were freshened and undermined to promote good capillary blood. Insertion of the graft was performed by one of 2 methods.
In TTM, after freshening of margins, gel foam pieces were placed in the middle ear cavity till they caused a slight bulge in the tympanic membrane (TM) remnant. Tragal perichondrium graft was inserted through the TM perforation and uniformly spread out with the help of micro-elevators to close all margins of the perforation and to rest between the gel foam medially and the remnant margins of the TM perforation laterally. Gel foam pieces were then placed laterally in the external auditory canal (EAC) to stabilize the graft and a small medicated wick was inserted over gel foam and box dressing was done.
In TMM, posterior tympanomeatal incision was taken, tympanomeatal flap along with the annulus was elevated and middle ear explored. Gel foam placed into the middle ear over which tragal perichondrium graft was placed using underlay technique. The tympanomeatal flap was then repositioned and stabilized with gel foam on the lateral surface in the EAC. A small
medicated wick was placed in the EAC and box dressing done.
Operative blood loss was minimal during both the procedure. Pain score was recorded in the post operative period after which the patients were discharged. Postoperatively, the patients were put on antibiotics, antihistamine and analgesic. Box dressing and ear pack was removed at 1 week, after which antibiotic ear drops were prescribed. The patients were then reviewed on 3rd, 6th and 12th post operative week.
On each visit, patients were evaluated for level of discomfort, success of graft uptake, alteration of taste and complication if any. During postoperative follow up no retraction pocket and no lateralization of the graft was observed in both the groups. Repeat audiogram to check the hearing improvement was carried out at 12th week post-operatively. No deterioration of hearing was observed in any case in our series.
Results
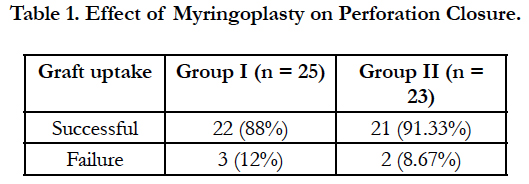
The age of the patients ranged from 18 to 45 years (mean age 32 years). Two patients in group II did not return for follow up at 12 week and hence were excluded from the study. In group I patients, perforation closure was successful in 22/25 ears (88%) and 3 ears (12%) had a residual small perforation. In group II patients, perforation closure was successful in 21/23 ears (91.3%) and 2 ears (8.67%) had residual small perforation (Table 1).
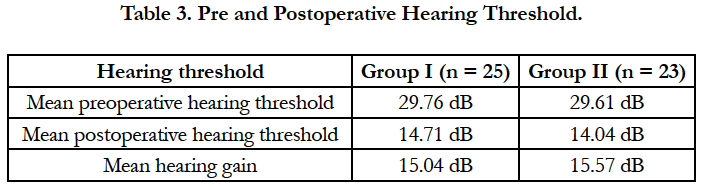
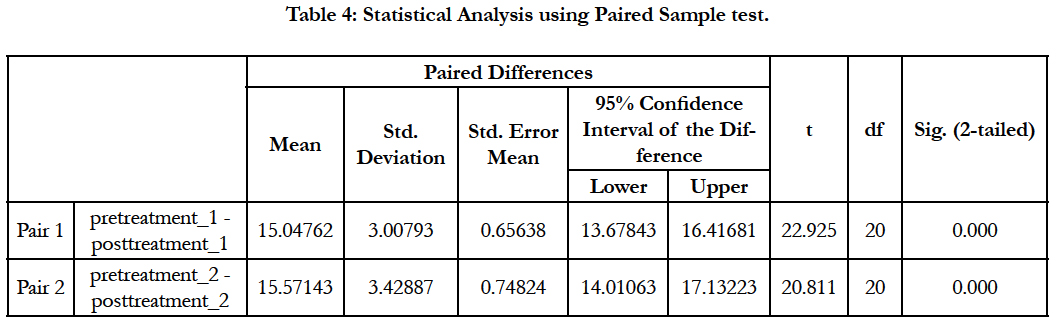
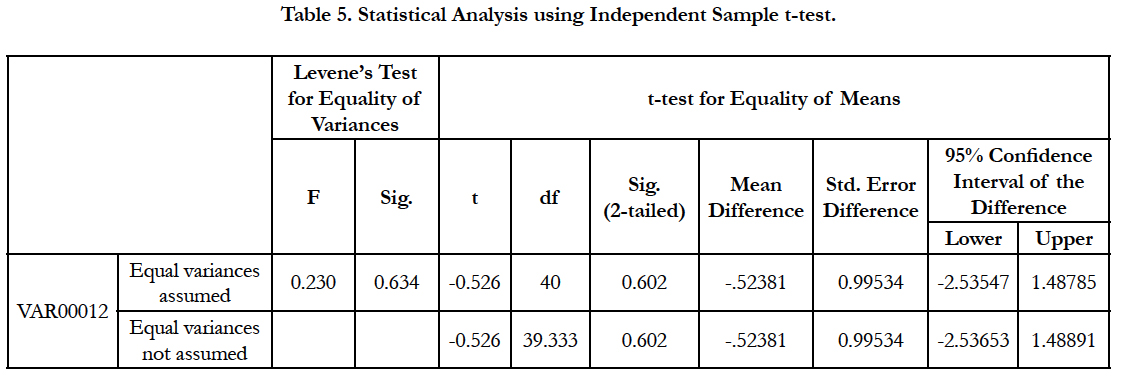
Hearing gain of more than 10 dB was achieved in 21/25 patients in group I and 21/23 patients in group II (Table 2). Pre and post-operative hearing threshold and mean hearing gain for successfully operated ears in group I and group II is listed in Table 3. To compare the pre and post operative ABG and the mean hearing gain in the two groups, paired Sample test and independent sample t-test was applied (Table 4). Both the group shows significant difference between pre operative and post operative ABG at 1% level P ≤ 0.01. There was no statistically significant difference found in the mean hearing gain between the two groups P > 0.05 (Table 5).
Time consumed in our TTM was approximately 40 minutes as compared with approximately 70 minutes for TMM. This reduction in operating surgical time improves the use of theater and decreases bearing on the patient when cases are done under local anaesthesia.
The mean pain score after the operation was 4.76 and 6.08 in group I and II patients respectively. The score was less in group I, mostly likely due to less manipulation of tissue (no elevation of flap) in these patients.
Discussion
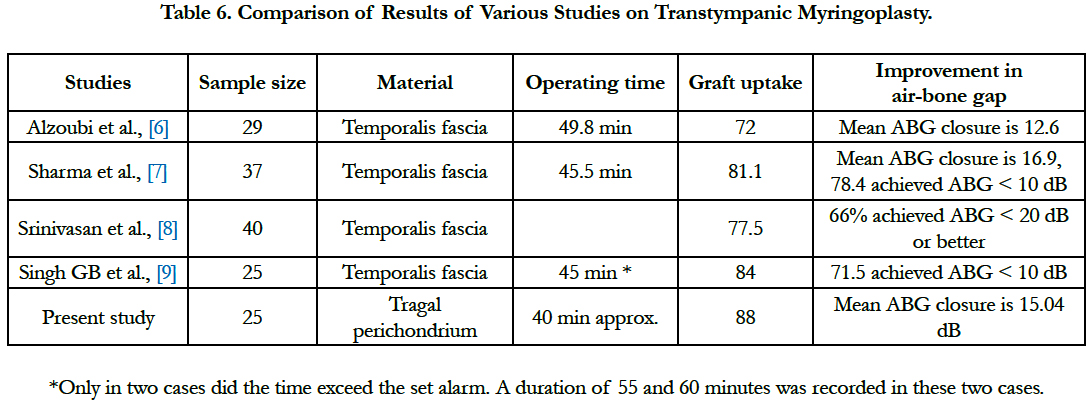
Graft uptake was seen in 22/25 ears (88%) and 21/23 ears (91.3%) in group I and II respectively. Naganuma et al., reported a 78% success rate in adults using homologous temporalis fascia as the graft material by the transtympanic method [5]. Our result of the transtympanic group is comparable to the other similar studies listed in Table 6.
Tapio and colleagues and El-Guindy used the transtympanic technique with endoscopes instead of a microscope. The Study by Tapio and colleagues revealed a success rate of 80% and 90% in terms of perforation closure and hearing improvement respectively [10] whereas El-Guindy reported a graft uptake of 91.7% and hearing improvement of 80% [11].
Hearing gain of more than 10 dB was seen in 21/25 patients (84%) in group I and 21/23 patients (91.3%) in group II. The mean hearing gain was 15.04 dB in the transtympanic group which is comparable to the study done by Alzoubi et al., [6] and Sharma et al., [7].
Also of importance is the fact that the time consumed in our TTM was approximately 40 minutes as compared with approximately 70 minutes for TMM. Felix in his study on 17 patients showed that the mean operating time for the Transtympanic group is 44.8 minutes [12]. Our findings are comparable to Felix and other similar studies listed in Table 6.
In our study the pain score was found to be 4.76 and 6.08 in group I and II patients respectively. Felix in his study showed that the mean pain score immediate after the operation is 3.2 for the transtympanic group and 2.9 for the tympanomeatal flap elevation group [12].
The advantages of this technique are less operating time and less post-operative pain. It also has no potential risk of injury to chorda tympani nerve and no chances of tympanomeatal flap tear unlike the tympanomeatal flap elevation technique. At times small size of perichondrial graft from one side of the tragal cartilage would be sufficient enough to cover the perforation.
The disadvantages associated with this technique are the chances of graft rejection because of a limited bed size for the graft and a limited area of mucosa that can be denuded blindly through the perforation to serve as a graft bed, supplying poor vascularity.
The demerits in our study design were the small sample size, some may regard the follow-up period of 3 months as short, and a detailed cost effective analysis was not carried out.
Conclusion
Transtympanic myringoplasty is a simple and less traumatic yet equally effective approach for the repair of perforated TM. It has the added advantages of minimal post-operative pain, costeffectiveness, no potential risk of injury to chorda tympani, no chances of tympanomeatal flap tear and results comparable to conventional techniques of myringoplasty.
References
- Fukuchi I, Cerchiari DP, Garcia E, Rezende CE, Rapport PB (2006) Tympanoplasty: surgical results and a comparison of the factors that may interfere in their success. Braz J Otorhinolaryngology. 72(2): 267-71.
- Golz A, Goldenberg D, Netzer A, Fradis M, Westerman T, et al., (2003) Paper patching for chronic tympanic membrane perforations. Otolaryngol Head Neck Surg. 128(4): 565-70.
- Austin DF, Shea JJ Jr (1961) A new system of tympanoplasty using vein graft. Laryngoscope. 71: 596-611.
- Shea JJ Jr (1960) Vein graft closure of eardrum perforations. J Laryngotol Otol. 74: 358-62.
- Naganuma H, Okamoto M, Shitara T, Tokumasu K, Fujino A, et al., (1994) Myringoplasty in outpatient clinic. Acta Otorhinolaryngology Belg. 48(1): 59-65.
- Firas Q Alzoubi, Amjed A Tarifi, Yousef Khader, John de Carpentier (2010) Comparison between transtympanic and elevation of tympanomeatal flap approaches in tympanoplasty. Otology Neurotol. 31(5): 773-775.
- Vishal Sharma, Krishna Chandra Rizal, Brijesh Sathian (2015) Comparative Results of Trans-Tympanic Pop-In Myringoplasty. Res J Pharm Biol Chem Sci. 6(5): 1497-1500.
- Srinivasan V, Toynton SC, Mangat KS (1997) Transtympanic myringoplasty in children. Int J Pediatr Otorhinolaryngol. 39(3): 199-204.
- Singh GB, Sharma A, Singh N (2006) Role of transtympanic myringoplasty in modern otology. J Otolaryngol. 35(6): 408-12.
- Tapio SK, Jaana HI, Heikki JP (2001) Tympanoscope-assisted myringoplasty. ORL J Otolrhinollaryngol Relat Spec. 63(6): 353-8.
- El-Guindy A (1992) Endoscopic transcanal myringoplasty. J Laryngology Otol. 106(6): 493-5.
- Comparison between transtympanic and tympanomeatal flap elevation approaches in myringoplasty. Dr Felix Tak-Yin LAU ENT, New Territories West Cluster, Hospital Authority.