Can Bi-levels Stairs and Two-Step Stool Climbing be Efficient Tools of Breathing Retraining in Overweight Dyspneic patients? (Effects on Hypertension, Dyspnea, breathing pattern, exercises and weight loss)
Gimenez M1*, Lantaron EM2, Polu E3, Aranda A4, Sierra V5, Lonsdorfer J6
1 Departments of Physical Medicine and Rehabilitation and Respiratory Physiotherapy, University Hospital of Gran Canaria Dr. Negrín, Bco de la Ballena
s/n, University of E-35020-Las Palmas de Gran Canaria, Spain.
2 Faculty of Physiotherapy- Universidade de Vigo, Campus of Pontevedra, A Xunqueira, Pontevedra, Spain.
3 Former Regional Institute of rehabilitation, University of Nancy, Nancy, France.
4 Alicia Senior Center, Renueva Street, Villamaňàn, León (Spain) Head of Service, Physiotherapy of aging and training muscular, Spain.
5 Departments of Physical Medicine and Rehabilitation and Physical Therapy, Respiratory, Gran Canaria University Hospital Dr. Negrín, Bco de la Ballena s/n, University of E-35020- Las Palmas de Gran Canaria, Spain.
6 Professor (ER) of the Faculty of Medicine, Physiology and Functional Explorations Strasbourg University Hospitals, 12 rue du Marais, Schiltigheim, France.
*Corresponding Author
Dr. Manuel Gimenez, MD, PhD,
Departments of Physical Medicine and Rehabilitation and Respiratory Physiotherapy,
University Hospital of Gran Canaria Dr. Negrín, Bco de la Ballena s/n,
University of E-35020- Las Palmas de Gran Canaria, Spain.
Tel: (00 34) 928260686
E-mail: gimen3@hotmail.com
Received: August 25, 2017; Accepted: October 24, 2017; Published: October 27, 2017
Citation:Gimenez M, Lantaron EM, Polu E, Aranda A, Sierra V, Lonsdorfer J. Can Bi-levels Stairs and Two-Step Stool Climbing be Efficient tools of Comprehensive Directed Breathing Retraining in Overweight Dyspneic Patients? (Effects on Dyspnea, Breathing Pattern, Exercises, Hypertension, and Weight Loss). 2017; Int J Resp Dis Care Med. 2(5):35-47. doi:dx.doi.org/10.19070/2577-4409-170007
Copyright: Gimenez M© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Improvements in exercise tolerance diminish with time upon cessation of the exercise program. Incremental Bi-levels “Two-stepstool test” (TSST) and Bi-level Stairs Climbing (BiSC) 30-45 minute session have routinely been used in pulmonary rehabilitation since 1968.
Introduction: Structured exercise rehabilitation programs of six to eight weeks duration have been reported to improve quality of life, increase exercise tolerance, and boost maximal oxygen consumption (VO2max) and endurance by 20 to 40%.
Objective: The purpose of this study was: (1) to analyze and assess subjective, physical, and some physiological responses to TSST; (2) to join the TSST (speed x20 times) with BiSC of 30 min, designed for endurance training at home; (3) to compare both tests at the maximal responses with those of incremental cycle-ergometry (30 W/3 min); (4) to analyze subjective, psychological and functional parameters of Dyspnea.
Design: This is a longitudinal study on 15 consecutive subjects with Dyspnea and overweight (39-66 yrs, BMI = 32.46 ± 6.77 kg/m2). Each subject performed the TSST at increasing speeds (10, 20, 30, times/min), on two 15 cm steps and, and 3 times the BiSC in 1 floor, up and down (20 steps 15 cm high each) under breathing education: Exertional dyspnea (ED), leg pain (LP), oxygen uptake (VO2), Ventilation (VE), respiratory rate (RR), tidal volume (VT), heart rate (HR), and peripheral oxyhemoglobin saturation (SpO2), were measured during TSST. Multivariate analysis for each parameter was analyzed according to a mixed model.
Results: All subjects increased significantly (p ≤ 0.01) the speed in the TSST (x60 times), and the BiSC (from 3 floors to 8 floors) and could maintain the speed (20/min) on the TSST and more than 15 min on the BiSC. After training, HR reached 80 to 96% of values at VO2max, thus high intensity. All parameters ED, LP, VE, RR, VO2 (p ≤ 0.01) and the weight (-16%). decreased to the same level of exercises, while VTand diaphragmatic mobility increased (p ≤ 0.01); Subjects found it simple, practical, and easy to perform the TSST and BiSC at home. There were no complications.
Conclusions: 1) The incremental TSST and BiSC are cost-effective exercise to assess subjective, physical, and physiological responses if used separately; 2) When combined (TSST with BiSC endurance of 30-40 minute session), they provide an efficient tool for endurance training at home (with HR and SpO2 controls).
2.Introduction
3.Methods
4 Subjects
5 Questionnaire and Physical Examination
6 Breathing Education
7 Measurements
7.1 Maximal Incremental Ergometry Test
7.2 Bi-level Stair Climbing Test (BiSC)
7.3 Two-Step Stool Exercise 10
7.4 How to Determine the 30 min Session Training using with Two Steps Tool and BiSC?
7.5 Statistical Analysis
8.Results
9.Discussion
9.1 Efficiency of the Maximal Level Exercise
9.2 Beneficial Choice of the 12 s-Peak Phase
9.3 Ventilatory Pattern
9.4 But, who is teaching Pulmonary Rehabilitation? And, in what Department are they teaching at the Hospital?
10.Conclusion
11.Acknowledgments
12.References
Keywords
Two-Step Stool Test; Bi-Level Stairs Climbing; Endurance, VO2max; Exertional Dyspnea; Leg Pain; Heart Rate; Oxygen Uptake; Ventilation; Respiratory Rate; Tidal Volume.
Introduction
Structured exercise rehabilitation programs of six to eight weeks duration have been reported to improve quality of life, increase exercise tolerance, and boost maximal oxygen consumption (VO2max) and endurance by 20 to 40%.
Significant benefits can be gained and maintained with just 45 minutes of daily maximal training on cycloergometry [4] for pulmonary and cardiac as well as for subjects with overweight and Dyspnea in pulmonary rehabilitation centers [1, 5]. Such ways could be stairs climbing [5-7], self-paced walking, and the Shuttle test (ISWT) [4]. Besides, many European chest physicians and oncologists often use stairs climbing to screen patients for impaired pulmonary function and subrogate of VO2max prior to surgery [7].
Concerning the overweight subjects [1, 5], the major respiratory complications of obesity 9 include heightened demand for ventilation, elevated work of breathing, respiratory muscle inefficiency and diminished respiratory compliance 5. In addition, patients with overweight may have arterial hypertension and, commonly develop alveolar hypoventilation with attenuated hypoxic and hypercapnic ventilatory responsiveness [4-6].
The weight loss program appears to be an effective therapeutic measure [4, 7]. However, pulmonary rehabilitation (PR) and especially training exercise, even without weight loss, appears to be as an extremely useful part of treatment [4, 6]. Exertional dyspnea (ED) appears faster in obese subject than in healthy ones 4. Body overload, especially abdominal fat, is the reason not only of his breathlessness, but also custom-diaphragmatic asynchrony treatment [3, 5-7]; the finding of ventilatory difficulty in obese subjects, does not neccesarily reflect the existence of respiratory or ventilatory disorders [7, 8].
Also Hypertension, which is common among obese patients with android obesity [4, 5], contributes to the increase of exertional dyspnea and ventilatory effort 8. Stair climbing is an economical option to provide both aerobic and resistance training without the need for specialized equipment [10-13]. Recently, we studied two Bi-level exercises: stair climbing (BiSC) [11] and Two-step stool [10, 12] (TSST) which involved climbing-descending to exhaustion [10, 11]. Nine cycles of submaximal BiSC [5] can provide, in healthy subjects, 30 minutes of aerobic endurance training at home [12].
The purpose of this study was: (1) To apply, at rest and exercises, Comprehensive Directed Breathing in the first phase of Pulmonary Rehabilitation (PR); (2) to develop 30 minute session training for TSST and BiSC, designed for endurance training at home; (3) to compare TSST and BiSC to maximal responses to those of incremental maximal cycleergometry [6, 10].
Methods
This study was approved by the institution’s ethics committee and was conducted according to Declaration of Helsinki standards. All subjects gave informed consent.
Subjects
Fifteen non medicated, active overweight males (BMI = 32.46 ± 6.77), who consulted our clinic for cardiopulmonary screening of exertional dyspnea (ED) and therapeutic exercise recommendations (training), were recruited for the study.
The inclusion criteria were: age over 25; active; no history of bronchospasm based on responses to the European Community for Steel and Coal (ECSC) questionnaire [14, 15], to have the stairs at home (building), clinical assessment at rest and after exercising to VO2max, and absence of wheezing and symptoms after maximal cycle ergometry testing; sufficient cardiopulmonary, neuromuscular, medical, and physical condition to permit strenuous exercise [10]. Exclusion criteria were abnormal spirometry, abnormal chest radiographs or electrocardiogram [10], wheezing or any other limiting cardiopulmonary symptoms. The target sample size of 15 subjects was pre-determined to achieve 80% power.
Questionnaire and Physical Examination
The physical examination included observation for nasal patency, mouth ventilation, and paradoxical breathing [14-16]. Analysis of breathing movements was made, by visual inspection, the subject standing in front of a mirror. Mouth breathing, shoulder elevation, and paradoxical chest/abdominal movements were demonstrated by a video recording.
Breathing Education
The program of the Comprehensive Directed Breathing (CDB) [6, 10, 12, 13] included enhancement of awareness of abnormal (asynchronous, paradoxical, and shallow) and normal breathing patterns. The subject watched himself breathing in a mirror; then he observed graphic representations of his ventilatory rhythm that were recorded on a spirogram; and finally, he watched a diaphragmatic breathing instructional film. The patients were also taught basic notions of the anatomy and physiology of ventilation and were trained in establishing nasal, diaphragmatic, and ventilatory synchrony. The patient learned to correct breathing dyssynchronism by looking in the mirror and breathing deeply with encouragement from the Physiotherapist to breathe slower and deeper with less accessory muscle participation and to avoid apneas. “Breathe through your nose and fill your lungs slowly and carefully, expanding your abdomen without moving neither your shoulders nor your chest; and now exhale the air slowly through your mouth, deflating your abdomen, and contracting your abdominal muscles, until the last of the air is expelled, and again this is repeated more than 50 times during each session” [6, 16, 17].
Measurements
Slow vital capacity (VC), forced expiratory volume in the first second (FEV1) and maximum voluntary ventilation (MVV) (Jaeger’s Oxycon Champion, Jaeger GmdH & Co., Wurzburg, Germany) calibrated with a 1L pomp before and after each use [19]. Bronchodilator (i.e. Salbutamol 0.2 mg) was administered in a second round of measurements, and the intra-subject difference had to be less than 15% for all parameters. The lower limit of normal spirometry values were calculated by subtracting the value 1.64 from the residual standard deviations, the so-called 5th percentiles [15]. VC 5th percentile was obtained by subtracting 0.92 liter from the classic formula value [15], and for FEV1 by subtracting 0.82 liter, to avoid false-negatives [15].
Exertional dyspnea was measured using the modified Borg scale, a 0-10 Liker scale whereby 10 represents the most severe ED ever experienced [18]. It was assessed (see below for more details) at the end of each single flight increment of BiSC until the maximal level, at the end of maximal speed on the Two-step stool, and after the cycle exercise to peak work rate (PWR).
Six minute walks (6-MWT) were performed over a straight, level surface of 50 meters marked at 5 meter intervals with a cone at each end. The test was carried out under the supervision of a therapist who measured peripheral oxyhemoglobin saturation (SpO2), RR, HR, ED, and leg pain in the beginning and at the end of the 6th minute [10, 12]. The subject could take breaks ad-lib within the defined testing time.
The subject was connected to a cardiac monitor (Multiscriptor EK; Hellige-France Inc, Strasbourg, France) while pedaling an electronically-braked cycle-ergometry (model 1000S, Medifit Inc, Maarn, The Netherlands). The initial 40 watts/min work rate for 10 minute was gradually increased by 30 watts every 3 minutes [13]. The PWR was estimated to be the maximum rate achieved in the last full 3 min before exhaustion [13], and the ventilatory anaerobic threshold (VAT) was calculated using established methods [13]. VO2max (Oxycon Champion, Eric Jaeger GmBH & Co.) was the highest value achieved over the last 30-sec collection period [10]. Minute ventilation (VE); tidal volumes (VT); RR; respiratory exchange, that is, oxygen uptake (VO2), and carbon dioxide output (VCO2) were measured with a Jaeger’s Oxycon Champion [13]. The SpO2 and HR were also continuously monitored (Biox Pulse Oximetry; Ohmeda, Louisville, CO) [13]. Dyspnea and leg pain levels were assessed using the Borg scale [18].
After the cycle ergometry test, subjects were randomized to take part in either of the two stair climbing and Two-step stool tests on the following day. The study took place in a 10-story building with uniformed floor-to-floor height of 3 meters. Permission to use the stairs was obtained. Each flight had 20 steps of 15 cm height and 25 cm breadth each [11]. Handrails were present and subjects permitted to use them ad lib. The stairs were sufficiently wide so there was no obstruction to traffic during the exercise. For BiSC [11] the subject was instructed to alternate between climbing and descending a single flight until exhaustion and the total number of flights was recorded. The stair climbing rate was standardized to 12 second and 8 second for down per flight of stairs [11] and initially paced by metronome, based on our previous work [6, 11].
Arterial pressure (AP), systolic (SAP) and diastolic (DAP), was measured at the end of all maximal tests. SpO2, HR, RR, ED, and leg pain (LP) were measured 10 minutes prior to both tests [10, 12] and after climbing each flight; then descending each flight for BiSC [12]. Dyspnea and leg pain were assessed at the end of each cycle. One physiatrist and one physiotherapist who were selected for their ability to keep up with the subjects performed the measurements during the 10 sec rest bits between flights. One person auscultated breath sounds for 10 seconds and extrapolated RR for one minute. The second person recorded HR and SpO2 while inquiring about Dyspnea and leg pain [18]. The time for each cycle was, therefore, a constant 30 second.
All subjects performed the BiSC [11] six weeks later to explore reproducibility. Subjects were surveyed after completing both protocols (before and after) on each of the quality measures: ease, reproducibility, safety, simplicity, and intensity [11]. The protocol that resulted in the greatest number of total flights climbed, or the maximal speed on the Two-step stool [10, 18]: faster heart rate, and that was considered the most tolerable and practical was chosen as the home exercise program.
Incremental Two-step exercise using 15-cm steps provided sufficient exercise while avoiding injuries [10]. The patients were told to stand in front of the first step with feet together, then to (1) place the right foot on the first step, (2) to place the left foot on the second step, (3) to place the right foot on the second step and join the feet together, (4) to place the left foot on the first step, (5) to place the right foot on the ground, and (6) to place the left foot on the ground and join the feet together, and to continue doing this repeatedly at the standardized increments.
There were slow-speed 5-min warm-up and cool down periods. The subjects were taught to coordinate climbing to speeds controlled by a metronome at the beginning breathing without paradoxical movements [19, 20]. Each subject performed 30-min TSSTs at 10, 20, until maximal times per minute, with 30-min rest periods between speed increases. The maximal speed was the highest tolerated by subjects. Physiologic parameters such as the SpO2, HR, VE, RR, exertional dyspnea (ED), and VO2 were measured continuously; tidal volume was calculated (VE/RR);
The maximum climbing rate sustainable for 30 min. determined by the TSST was used [10]. After completion of the protocol, the subjects were surveyed on their feedback by answering the following questions: is the TSSE rapid, reproducible, safe, easy to understand, maximally intense, home-use friendly, and economical [11].
On cycle ergometry [13] and the BiSC [11], it was relatively easy, because the maximum levels in both tests were elevated [11-13]. In the first case [13], the levels are in watts according to the ventilatory anaerobic threshold [13]. For the BiSC [11] and TSST [10], by the number of floors or steps that subjects could climb from which, it was established a session of regarding 30 minutes with the submaximal level BiSC-5 [12].
For the BiSC [15] the maximal level was only on the third floor. We have retained the following considerations:
1) The rise and the descent of a flight takes, for 20 steps:
2) 20 steps x 10 times = 200 steps + (x 1/3 = 67 down steps) [11]; Total = 267 Steps
3) 20 steps x 20 times = 400 steps + (x 1/3 = 133 down steps); Total = 533 steps
4) 20 steps x 30 times = 600 steps + (x 1/3 = 180 down steps, Total = 780 steps
5) 20 steps x 80 times = 1600 steps (x 1/3 = 533 down steps; Total = 2133 steps.
It is known [11] that going up and down a Flight takes 30 seconds, timed (12s to go up and 8s to go down), plus 10 s for controlling the variables; this is 30s per floor.
From the point of view of time:
Time 30 "x 15 Floors x 1 time = 450" (/ 60s) = 7 min 50 "for one cycle”;
7 min 50 "x 15 Floors x 2 times = 15 minutes two cycles
7 min 50 "x 15 Floors x 3 times = 22.5 minutes three cycles
7 min 50 "x 15 Floors x 4 times = 30 minutes four cycles
(total 30 cm) on 1 trip), in 6 seconds; the energy of the dawn was previously [10] calculated as 1/3 of the climbed. Thus,
1) The rise and the descent of a flight takes, for 20 steps:
2) 20 steps x 10 times = 200 steps + (x 1/3 = 67 down the steps) [11]; Total = 267 Steps
3) 20 steps x 20 times = 400 steps + (x 1/3 = 133 down the steps); Total = 533 steps
4) 20 steps x 30 times = 600 steps + (x 1/3 = 180 down the steps, Total = 780 steps
5) 20 steps x 80 times = 1600 steps (x 1/3 = 533 down the steps; Total = 2133 steps.
6) Speed x 60 times/minute : 120 steps + 40.2 down Total = 160.2 steps
After completion of the protocol, the subjects were surveyed on their feedback by answering the following questions: is the TSST rapid, reproducible, safe, easy to understand, maximally intense, home-use friendly, and economic?
It is know [11] that going up and down a Flight takes 30 seconds, timed (12s to go up and 8s to go down), plus 10 s for controlling the variables; this is 30s per floor.
From the point of view of time:
Time 30 "x 15 Floors x 1 time = 450" (/ 60s) = 7 min 50 "for one cycle”;
7 min 50 "x 15 Floors x 2 times = 15 minutes two cycles 7 min 50 "x 15 Floors x 3 times = 22.5 minutes three cycles 7 min 50 "x 15 Floors x 4 times = 30 minutes four cycles.
For the TWO-STEP STOOL [10]: Speeds for climb and down Two steps of 15 cm each (total 30 cm) on the 1 trip, in 6 seconds; the energy of the dawn was previously 10 calculated as 1/3 of the climbed. Thus,
1. Speed x 10 times/minute; 20 steps + 6.7 down Total = 26.7 steps
2. Speed x 20 times/minute: 40 steps + 13.4 down Total= 53.4 steps
3. Speed x 30 times/minute: 60 steps + 20 down Total = 80 steps
4. Speed x 40 times/minute: 80 steps + 26.8 down Total = 106.8 steps
5. Speed x 50 times/minute: 107steps + 35.5 down Total = 142.2 steps
6. Speed x 60 times/minute: 120 steps + 40.2 down Total = 160.2 steps.
After completion of the protocol, the subjects were surveyed on their feedback by answering the following questions: is the TSST rapid, reproducible, safe, easy to understand, maximally intense, home-use friendly, and economical.
The measured responses were summarized as means and standard deviations or medians and interquartile ranges (IQR) based on the data distribution [21]. T-test and Wilcoxon test for independent variables were used for BiSC data [21]. Statistical significance was set at p <0.05. The attained SAP, DAP, and HR values at rest, after the 10th floor of the BiSC, and from a previously report [16] “Two-Step Stool exercise protocol” [18], and at PWR of the incremental cycling [10, 13], were compared. The means were also estimated by means of confidence intervals at 95%. All statistical analyses were performed using the R package, version 3.0.1 (R Development Core Team, 2013) [21].
Results
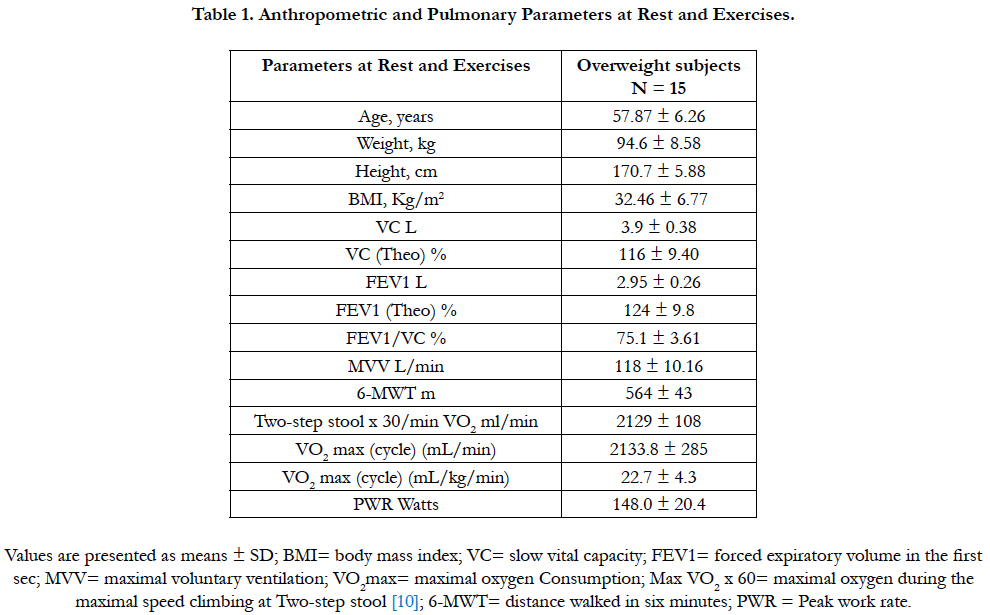
Fifteen subjects were qualified. They were all males, aged described in Table 1, and had an average body mass index elevated (see Table 1). They were no smokers.
All 15 subjects climbed 3 flights of stairs prior to exhaustion on the BiSC [11] protocol, and for the speed on Two-step stool [10] they stop at the speed x30 with a ventilation at 55 l/min (healthy subjects around 30 l/min) [10] i.e. overbreathing at + 45% of VE. The maximal attained levels are henceforth designated as BiSC-3 and TSST x30 times. Both maximal levels allowed the subjects to reach 80-95% of the heart rate observed in the PWR attained on the incremental cycle ergometry test [13].
Table 1 summarizes the subjects’ demographic, pulmonary function, and exercise data. VO2max was 34.0 ± 5.5 ml/(kg. min). All subjects completed the test without stopping and only SpO2 was mildly decreased. This decrease is significant (p≤ 0. 001) compared to that found at the end of disc 10th (Table 2), and has been previously reported [11, 13].
Table 2. Right and Left Diaphragmatic Mobility after Pulmonary Rehabilitation in 15 Dyspneic Overweight Subjects.
After CDB and training, there was an increase of MVV (142 ± 9.3; +20%), PWR (178 ± 17 watts, +19%), VO2 peak (27.2 ± 3.9 mL/kg/min; +20%), all three significantly (p ≤ 0.01), and discrete increase for 6MWT (592 ± 36 m; + 5%, Non Significant).
Table 2 shows the Right and Left Diaphragmatic mobility before and after Respiratory Rehabilitation. There was an important reduction at the baseline in both sides. After Rehabilitation, there are significantly changes on the right (+ 169 %) and on the left (+136%).
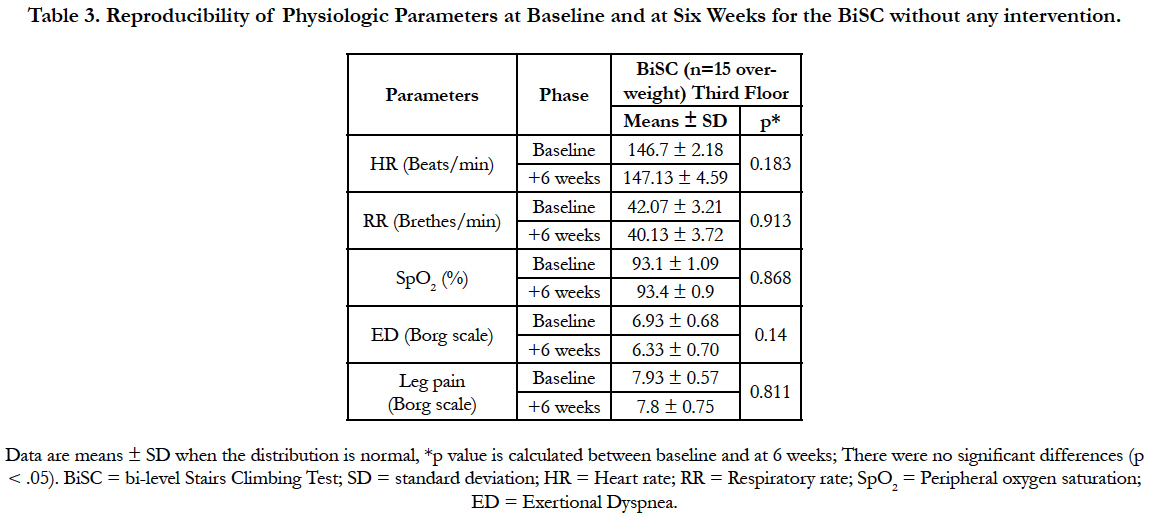
Table 3 summarizes the stair climbing exercise data for BiSC to analyze its reproducibility; for the five variables, there were no significant differences.
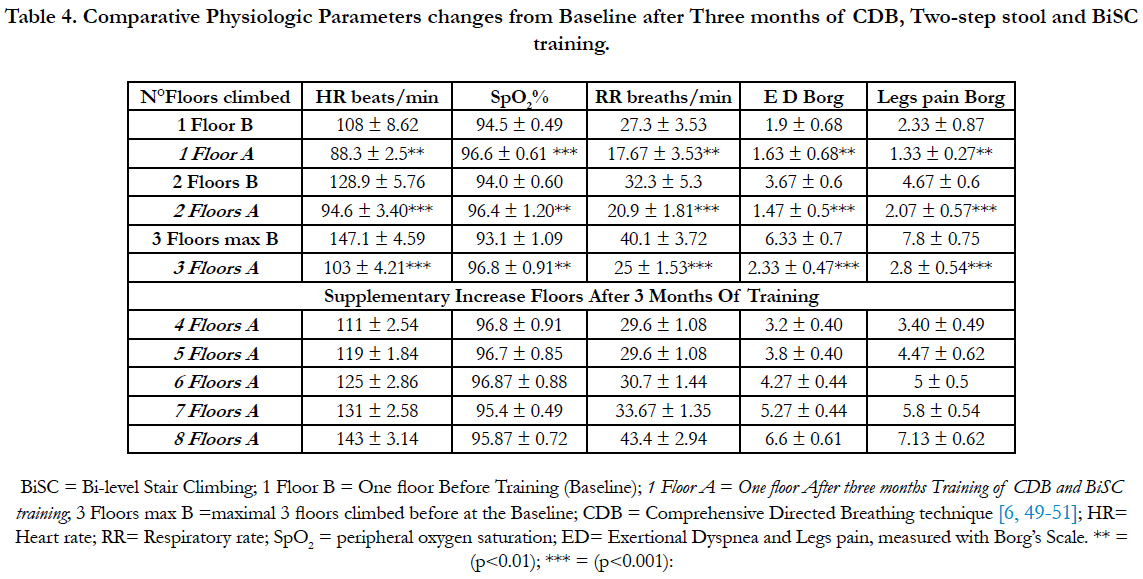
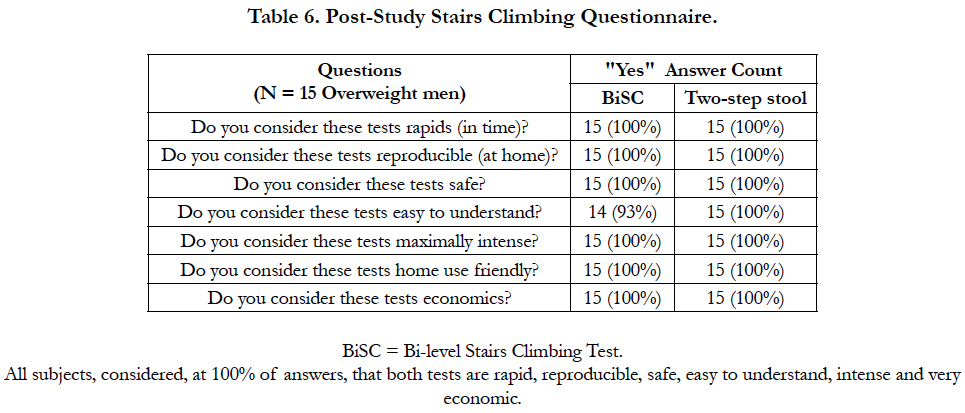
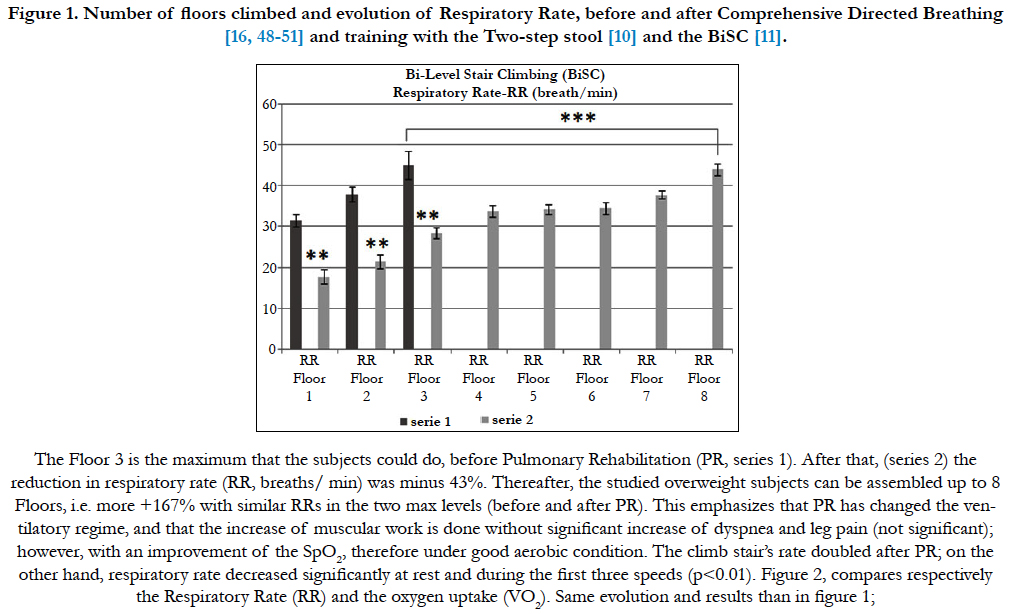
Table 4 Compares: (a) the parameters HR, SpO2, RR, ED, and legs pain, before and after three months of Respiratory Rehabilitation; (b) values at baseline and after a three months evolution; (c) and shows the mean values of these parameters, for the five complementary floors, gained after Pulmonary Rehabilitation protocol. There are important and significantly ***= (p<0.001) reduction of all variables. Moreover, comparing both maximal floors observed before (3 flights) and after (8 flights), figure 1, the increase is +167% (p<0.001).
Table 3. Reproducibility of Physiologic Parameters at Baseline and at Six Weeks for the BiSC without any intervention.
Table 4. Comparative Physiologic Parameters changes from Baseline after Three months of CDB, Two-step stool and BiSC training.
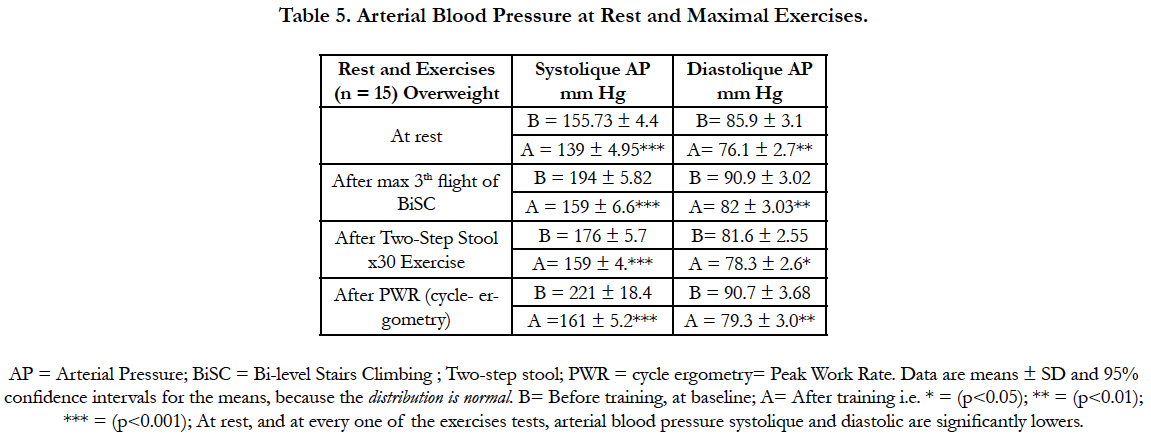
Table 5: Compares arterial blood gases at rest and maximal exercises i.e. 3 flights max before PR and 8 flights after Rehabilitation PR; for the Two-step stool the speed was before (x30 times) and after (x60 times), and before and after Peak Work Rate. In all comparisons Systolic and Diastolic blood pressures are significantly reduced (p≤0.01).
after (x60 times), and before and after Peak Work Rate. 1n all comparisons Systolic and Diastolic blood pressures are significantly reduced (p≤0. 01).
Figure 1: The Floor 3 is the maximum that the subjects could do before Pulmonary Rehabilitation (PR). After that, the reduction in respiratory rate (RR) was minus 43%. The studied overweight subjects can be assembled up to 8 Floors, i.e. more +167% with similar RRs in the two max levels (before and after PR).
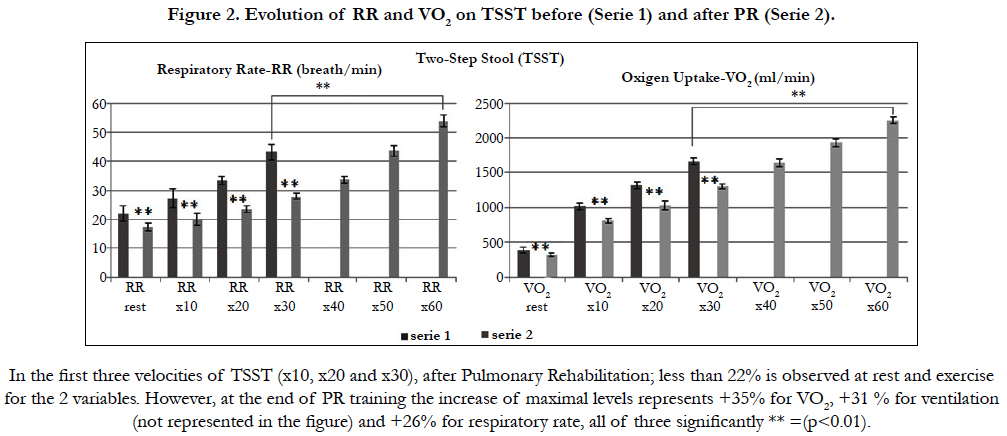
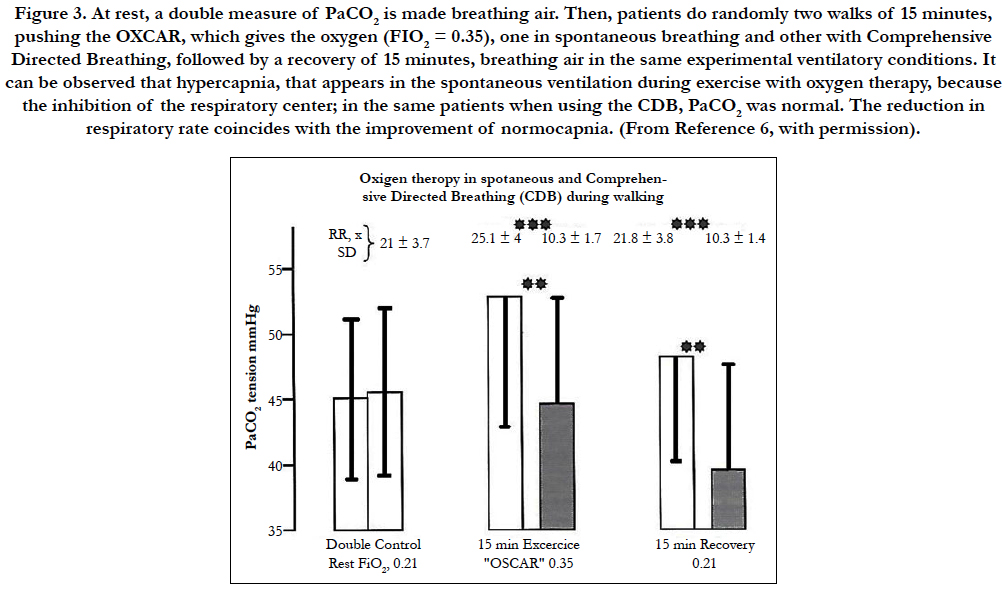
Figure 2 shows the evolution of RR and VO2 on TSST before PR (Serie 1) and after PR (Serie 2). In the first three velocities of TSST (x10, x20 and x30), after Pulmonary Rehabilitation; less than 22% is observed at rest and exercise for the 2 variables. However, at the end of PR training, the increase of maximal levels represents +35% for VO2, +31 % for ventilation (not represented in the figure) and +26% for respiratory rate, all of three significantly ** =(p<0.01).
Figure 3. RR = Respiratory rate (breathes/min). At rest, a double measure of PaCO2 is made breathing air. Then, patients do randomly two walks of 15 minutes, pushing the OXCAR (Oxygen Cart) [20, 23], which gives the oxygen (FIO2 = 0.35), one in spontaneous breathing and other with Comprehensive Directed Breathing when learned, followed by a recovery of 15 minutes, breathing air in the same experimental ventilatory conditions. It can be observed that hypercapnia, appears in the spontaneous ventilation during exercise with oxygen therapy, because the inhibition of the respiratory center; in the same patients when using the CDB, PaCO2 was normal. The reduction in respiratory rate coincides with the improvement of normocapnia [6, 13, 20] (with permission) [6].
Figure 3. At rest, a double measure of PaCO2 is made breathing air. Then, patients do randomly two walks of 15 minutes, pushing the OXCAR, which gives the oxygen (FIO2 = 0.35), one in spontaneous breathing and other with Comprehensive Directed Breathing, followed by a recovery of 15 minutes, breathing air in the same experimental ventilatory conditions. It can be observed that hypercapnia, that appears in the spontaneous ventilation during exercise with oxygen therapy, because the inhibition of the respiratory center; in the same patients when using the CDB, PaCO2 was normal. The reduction in respiratory rate coincides with the improvement of normocapnia. (From Reference 6, with permission).
Discussion
The present study shows that: 3-months training were significant beneficial using Comprehensive Directed Breathing during the special bi-levels BiSC [11] and TSST-Training [10]. With this technique, it is observed that: First, the 15 subjects presented a full adherence to the training program, i.e. 100%; Second, most of the stated exercise impairment initially found, including overbreathing, exertional dyspnea, arterial blood hypertension and lower endurance exercise could be reversed by adequate training; Third, the force and endurance of skeletal and respiratory muscles were improved; Fourth, the ventilatory pattern, especially at the peak level of the exercises was changed with lower RR and higher VT while VO2 did not change (Figure 1 and 2); Fifth, Table 2 shows that diaphragmatic mobility was reduced prior to Pulmonary Rehabilitation and, that under the effects of Comprehensive Directed Breathing, overweight subjects learn to master their diaphragm correctly without asynchrony or the effects of paradoxical ventilation [12, 16, 17]; Sixth, with lower respiratory rate the patients could perform significantly higher work; the comparison of the maximal RR before training, with the maximal 8th floor after PR, the respiratory rate is similar. These reductions are economical (Figure 2), because the oxygen consumption is simultaneously reduced at rest, and during exercises. This is also the consequence of an important diaphragmatic mobility, without paradoxical ventilation neither asynchronisms (Table 2), nor hypercapnia (Figure 3). Moreover, exertional dyspnea and pain in the legs are significantly lower allowing performing higher levels. Dyspnea during the 12s-peak of the BiSC-test was only 35% of the dyspnea at O2 peak of the incremental exercise, i.e. for the same maximal power-work. Therefore, BiSC is especially well tolerated since it is subjectively less dyspneic, respects the homeostasis, because there is no time to stimuli the anaerobic limits, neither the metabolic acidosis during the full test [16, 17, 20].
All subjects were able to tolerate 30 minutes with the TSST and 30 minutes with the BiSC, which subsequently made it possible to determine, with both tests, a single training session of 30 to 40 minutes of Endurance at home, which was well tolerated. The initial oxygen therapy in the hospital, corrected, at the beginning, the discrete hypoxemia observed during the maximum exercises (PWR, TSST and BiSC). After that, the CDB single provided effective alveolar ventilation without hypoxemia. After the first fifteen training sessions at the hospital, subjects performing both tests and, the CDB learned fairly well, the Staff go together with the subject to adapt the training in his own stairs of the building, where he lives, with the opportunity to train under the supervision of a member of the PR team [12, 13, 16, 20]. However, two subjects who did not have stairs at home, the adaptation was made with the purchase of an economic Two-step stool (wooden stool), reproduced, with the same dimensions [6, 12, 13, 20]. In this way, at the end of the Pulmonary Rehabilitation program, the subject can continue his training at home, to retain the clinical improvements noted in the hospital.
Thus, both bi-level training models ( Two-step stool and Bi-level climbing stairs) get similar significant training responses than in healthy subjects [17, 19], increasing VO2max (+30%) and endurance capacity (+40%), while inducing less symptoms like dyspnea or leg discomfort, during exercise sessions (p≤0. 01) [6, 13, 16, 17, 20].
There were no formal trials criteria for training dyspneic overweight patients [1-3, 19]. It is therefore likely that concordance with the program will relate to motivation and access [1-3, 16, 17]. In the BiSC program published until now [20, 21], the good motivation was assured by the limited exertional dyspnea, the magnetism of the test itself and by the initial intervention of the whole Rehabilitation Team [12, 16, 20, 23].
In addition, the continuous dialogue and explanations given by the specialized physiatrist and a physiotherapist, during all the training sessions, justify the good adherence (100%) of the subjects [16, 17]. In the same way, Vallet et al., [22] our team [23], Casaburi et al., [24] Bodenheimer et al., [25] and Cahalin et al., [27] published studies illustrating the importance of individualized training. In general, these exigencies are not esteemed.
The significant benefits in the BiSC users, contrast with the negative results of the literature [32-36]; these differences could be: (a) the constant versus bi-level training regimen, and (b) the work applied by a group of specialists in Pulmonary Rehabilitation. Our team includes: Pneumologists, Physiatrist, Physiotherapist, Psychologist, and specialist for muscular training, all interested and working in Pulmonary Rehabilitation [16, 17]. In the literature, frequently the constant "training load" represented a vast submaximal exercise between 30-95 % of the maximum performed [1-6]. Using a maximal level could be more efficient, and more particularly during a sufficiently short period, to avoid exertional dyspnea, including patients before and after pulmonary transplant. These two reasons represent the main benefit of the two bi-level strategies used in this study [12, 16, 17, 20].
The first interest of the BiSC and TSST programs is to use some phases of maximal load. Eight weeks of endurance training, performing heavy constant cycle ergometry exercise daily for 45 min, was studied by Casaburi et al., [24] in healthy subjects and in patients with COPD [24]. It supports the view that training at a level below anaerobic threshold (AT) work was less efficient to reduce ventilation and production of lactate that power above AT [24].
It is unlikely that this 12s-maximal power causes contractile fatigue of the diaphragm since Mador et al., [31] demonstrated that, even in COPD patients, and even after high-intensity constant workload cycle exercise at the limit of tolerance they do not found any fatigue [31].
There is modest information, however, about the recognized perception of dyspnea when the patient undergoes high intensity constant or bi-level work rate exercise [23]. We have recently published 32 a paper comparing and discussing the differences of dyspnea in six maximal exercises, used in Pulmonary rehabilitation, comparing either constant [24], Bi-level (Square wave exercise endurance test =SWEET) [23, 32, 33], interval [34, 35], or the 6-MWT [37]. The 6-MWT’s ED [44] is 95% of Sweet-peak’s ED [23, 33] and both represent respectively 65% and 69% of the PWR ED. Moreover, the 6-MWT usually considered as moderate, is energetically higher than AT and represents roughly 80% or either 100% of the O2 peak, in COPD patients [12, 33]. In addition, in the subjects of the present study; with average PWR of 150 W, the 6-MWT ED represents 65% of the PWR ED but 95% of the Sweet-peak ED [33]. Thus the 6-MWT is a hard test. Moreover, the speed of the 6-MWT has never been studied; thus it is difficult to study the energetic cost of the test or its application for training. Also, this test usually presents hypoxemia, at times very important.
The shuttle test (ISWT) [37], is also proposed for training. However, in addition to the predicting distances, it is more difficult to determine the intensity of the treadmill endurance. As described by the authors [5, 37], in order to relate the intensity of the treadmill endurance tests to a percentage of the patient’s maximum exercise capacity on a treadmill, an incremental, symptom limited test was performed to establish individual values of VO2 peak [37].
On a separate occasion a submaximal treadmill test was also performed in order to identify the relationship between oxygen uptake and treadmill walking speed for each patient [37]. This submaximal test consisted of three different walking speeds, of four minutes duration, with a short rest period between each. The VO2 was measured during each stage and a graph of VO2 and the corresponding speed was plotted for each patient [31]. The walking speeds which related to 75%, 85%, and 95% of the measured VO2 peak, for each patient, was interpolated from their own individual graph [37]. The three customized walking speeds were used for the treadmill endurance tests. The treadmill endurance tests were conducted in a manner similar to the field tests, instructed to walk for as long as possible [37]. This protocol is very hard and need many controls the walk on the field, and at the Laboratory of muscular exercise; the speed of the three levels is not clear; also the treadmill is not a test of fields; second, for authors who do not have a treadmill and use a cycle ergometry, extrapolation to a march or run, presents serious difficulties [37]; However, in the TSST [10] VO2 has been directly measured [10], with subjective feelings, dyspnea, legs pain and heart rate in the three (before) or six shear rates possible (after [10], Table 3);
These are personal data measured during the training session, to the maximum level [10]. Furthermore, in the same conditions, were measured, at the same speeds, and can be known indirectly the consumed VO2 [10]. Therefore, our data are more objective, and less complicated to determine for researchers and patients [10].
Because of the learning effect, while no verbal encouragement is used, and given that it is externally paced, a follow test of the ISWT [5, 37] is recommended. Although there are no guidelines, contraindications, for the test and reasons for immediate interruption which are valid for the 6-MWT is also applied to the ISWT [37]. The use of interval training as opposed to continuous training is the second strategy that can be used to increase load of Peak work rate (PWR) and endurance, as the intermittent exercise proposed by Coppoolse et al., [34], and Vogiatzis et al., [35]. The first study [34], is really a bi-level test, with 21 patients compared an intermittent 30 min-exercise with one minute of peak to 90% of the PWR and two minutes to 45 %, with a constant exercise at 60% of the PWR [34]. Training did not result in a significant improvement in lung function neither the ventilatory pattern, but only maximal inspiratory mouth pressure increased in both groups by 10% in Constant, and 23% in intermittent (bi-level?) test; O2 peak, increased by 10% [34]. Vogiatzis et al., [35] studied [36] patients with COPD that were assigned to 40 min-cycling, twice weekly for 12 weeks, either at 30s-intensive interval (20 times with 30s-rest interval) or continuously at 50% of baseline PWR 35. Both groups declared similar improvements in exercise tolerance and quality of life. However, the interval-training group perceived less dyspnea during exercise [35].
Critical point, the homeostasis requires to be considered when training healthy subjects and, chiefly in patients [36]. For instance, during five consecutive sessions of one minute maximal bout, followed by four minutes rest, the pH decreased progressively and drastically, in a group of healthy subjects, with a recovery after exercise as long as 30 minutes [43]. Sabapathy et al., [38] studied the physiological responses of 10 patients with moderate COPD (FEV1=50%) who performed both an intermittent (1 min exercise and rest intervals) and a continuous cycle ergometry exercise on separate days, both tests performed at 70% of the peak Workrate (i.e.≈ 40 W) determined during an incremental exercise test (4W/30s), VO2 peak, (14.8 mL/kg/min) and Work-rate peak (57W) were very low [38]. Subjects were able to complete a significantly greater total amount of work during intermittent exercise (71kJ) than during continuous (31kJ). The degree of dynamic lung hyperinflation was significantly lower during intermittent exercise than in continuous exercise [38]. These results suggest that the intermittent exercise seems to be more efficient and tolerated than continuous exercise and constitutes a better mode of training for patients with COPD [38]. In our study [11] with the BiSC, dyspneic subject’s climbed10 flights, as with the continuous they couldn’t climb more than eight flights with significantly more dyspnea [11].
The 12 seconds of the bi-level peak phase of the BiSC, represents less than the first 30s of a maximal constant exercise. On the physiological point of view, and because the 12 second-exponential increase in the VO2 at the start of a constant power exercise, in the first minute VO2 reaches about 65 % of the VO2 peak [13], thus much lower than that. Then, without really reaching the corresponding high metabolic rate, the BiSC peak explores and achieves the maximum power and thus trains well peripheral and respiratory muscles [16, 17].
In addition, the BiSC-peak trains the alactic anaerobiosis, within about the first 12 seconds. Thus, in this last period, it provokes a hyperventilation at the origin of the observed ventilatory alkalosis [10, 13, 33], that corrects, at least partially, the metabolic acidosis, due to the excess of lactate [24]. Moreover, during (descending 8s) the base aerobic phase, the working muscles transform the excess of lactate in glucose by glyconeogenesis [24]. These two mechanisms explained, probably, the normal tolerance maintained during the session training of the BiSC in healthy subjects, and in the overweight subjects of this study. This is in agreement with the study of Hermansen et al., [36] showing that during the active recovery after a maximal exercise test, the excess of lactate was faster metabolized during active than passive recovery [36].
In patients, the reduction in VT was almost entirely caused by an increase in end expiratory lung volume (EELV) [37] with little changes in end inspiratory lung volume (EILV) [37]. The increase in EELV, or hyperinflation, is the corollary of the difficulty to expire through highly resistive airways. The increased EELV impedes the inspiratory muscles and, for a given central inspiratory drive, causes a decrease in VT and increases RR.
Thus, strategies to lessen dynamic hyperinflation at a given amount of exercise are the aim in pulmonary rehabilitation [35], breathing exercise and exercise training. We undertook a study to test the effect of different exercises (isometric and during varying levels of dynamic incremental exercise on cycle ergometry) on EELV in active well trained cyclists (T), with low Respiratory Rate (RR), compared to healthy untrained volunteers (NT, non trained), with higher RR, using coupled respiratory inductive plethysmography (RIP). The T group demonstrated a significant decrease in thoracic EELV under all exercise conditions and a complete post-exercise recovery, while NT participants recruited their respiratory reserve volume only for the higher levels of the incremental test and did not totally recover: These findings suggest that the better increase in ventilation by deepening expiration observed in the present study, after BiSC training in the overweight ED subjects during exercise, is similar to what is observed in sportsmen experienced in endurance training compared to sedentary people. That underlines the advantages of high intensity rehabilitative exercise training. For all overweight in the BiSC, it was apparent that, after TSST and BiSC-training, their physiological capacity for various exercises (6-MWT, 40w constant work, incremental exercise) had improved.
Furthermore, the applied voluntary Diaphragmatic Breathing [6, 37, 38], principally oriented on the diaphragm activity, (Tables 2 and 3) can also reduces the additional solicitation of accessory and intercostals muscles and thus eliminates dyssynchronism and the smallest participation of the rib cage [37, 38]. The reduced VO2, ED , and RR for a given work rate are consistent with this notion [32] (Table 4, Figures 2 and 3).
The main beneficial effect for respiratory function at rest seems to be the decrease in EELV produced by the voluntary deep diaphragmatic effort, principally expiratory. Moreover, they could also be the increased efficiency of ventilation by the recovery of a maximal diaphragmatic mobility (Table 2); During the BiSC-30min training dyspnea and the leg discomfort are moderated during the 30 minutes, as well as the systolic arterial blood pressure, that are significantly lower (p<0.01), and equivalent to that of the values observed at PWR of the incremental exercise.
The effect of oxygen therapy on exercise [41, 42], in moderately desaturated patients, at the peak of VO2, has been studied [41, 42]. It should be noted that desaturation rarely declined below 90% [42]. They analyzed the acute effects of O2 that had no predictive effects on the effects of training [50]. This suggests that oxygen and training can improve exercise by different ones. Oxygen therapy reduces lactate values, and since lactate levels are an important training stimulus, VO2 exercise supplementation may reduce the effects of training [41].
Given the moderate hypoxemia observed in intensive efforts, we decided to add oxygen therapy for the first 10 training sessions so that SpO2 was always above 94%. After this initial "protective" phase, subjects could perform the sessions without additional oxygen, with an always satisfactory SpO2 (Table 4) [42]. This suggests that the application of the CDB [14-27, 39] had already begun to improve the ventilatory regimen of these subjects dyspneic and overweight, but also the distribution of ventilation [48] and the mechanical behavior of the respiratory system [40].
The beneficial use of BiSC-training and Comprehensive Directed Breathing that we observed in the present study, in active overweight subjects, with a significant decline in dyspnea during exercises, confirm the positive results that we had previously found in patients with moderate or severe COPD, and lung transplant recipients [16, 17, 39-41, 44]. Thus, patients, with any significant desaturation in exercise, can also be training, with oxygen therapy, at levels of exercises comparable to healthy subjects of the same age and physical activity [6, 17, 43, 44].
The significant benefits in the BiSC and TSST users, contrast to the negative results of the literature [26-30]; these differences could be: (a) the constant versus interval or bi-level training regimen, and (b) the work applied to a group of specialists on Pulmonary Rehabilitation [14-17, 39, 40]. Our team includes: Pneumologists, Physiatrist, Physiotherapist, Psychologist, and specialist for muscular training, all of them interested and working in Pulmonary Rehabilitation.
No formal trials criteria existed for training dyspneic overweight patients [1-3, 19]. It is therefore likely that concordance with the program will relate to motivation and access [1-3, 17, 19, 42]. In the BiSC program published until now [17], the good motivation was assured by the limited dyspnea, the magnetism of the test itself and by the initial intervention of the whole Rehabilitation Team. In addition, the continuous dialogue and explanations given by the specialized physiatrist and physiotherapist, during all the training sessions, justify the good adherence (100%) of the subjects [17, 43]. In the same way, Vallet et al, [22], Casaburi et al, [24] our team [23], Bodenheimer et al., [25] and Cahalin et al., [26] published studies illustrating the importance of individualized training. In general, these exigencies are not esteemed [6, 20].
In an interesting article [45] entitled: “Are we forgetting the evidence?” Also, Jonson MK, and Stevenson RK [46] (2002) describe a multi-center study in England with 1,400 COPD patients from 38 hospitals in acute admission, to compare clinical practice with the recommendations of the British Thoracic Society. It appears that: “The educational staff of teaching represents 28%; this shows that the consensus recommendations for the primary care of the asthmatic patient are not, for the most part, respected, those responsible for this education are neither defined nor available and, consequently, a lack of responsibility for doctors and paramedical personnel is lacking” [43], Greater coordination of acts and, in conclusion, there is the absence of a respiratory rehabilitation team as defined or proposed [45, 46]. In addition, Cahalin et al., [20] found that more than 75% of the studies in their revue did not report a method to examine competency in diaphragmatic breathing [26] and there were no diaphragmatic instruction in 71%. Usually the Physiotherapist works alone because no Physiatrist is present in the physical room neither team of PR. These complicated situations explained most of the negatives results of Pulmonary Rehabilitation.
Furthermore, Sava et al., [47] in training COPD patients with three category of BMI observed that BMI had no effect on outcomes on univariate or multivariate regression analyses, taking account differences in baseline pulmonary function [47]. Obese and overweight patients had higher FEV1 and FEV1/FVC ratio than their lean counterparts [47], results that is also observed in this study. One possible explanation, they say, is that patients with weight excess tend to be more dyspneic for a given FEV1, as illustrated by the higher Borg dyspnea and leg fatigue scores found in the obese patients during 6MWT [47]. A second possible explanation is the fact that they could have alveolar hypoventilation during exercises, because they have overbreathing, high RR and lower tidal volume with asynchronisms [6, 23, 47]. Their prospective study [47], therefore, adds to this information in showing that dyspnea, quality of life and exercise tolerance improve as much in the obese and overweight COPD patients as their normal BMI counterparts [47].
Our results contribute to a better understanding of the physiology of bi-level with median and high intensity exercise in overweight ED subjects, and help determine the best target work rate intensity for training, as well as provide ventilatory support for counseling these patients, on how to better breath, without asynchronisms, and tolerate activities of daily living: a) that required sudden onset, like in the peak, or b) sustained moderate work like the negative work base of the BiSC-and Two-step stool Training, and enhance well adapted ventilation. In this way, simultaneously to the reduction of RR, the metabolism (VO2) is as well reduced, as previously demonstrated [6, 42]. Once more and, contrary to the affirmation of several studies [26-30] the CDB does not increase metabolism (VO2) neither the work of breathing [6, 42, 43, 49-51]. CDB is realized without hypercapnia, ventilatory asynchronisms neither paradoxical ventilation. Moreover, CDB increases alveolar ventilation (Figure 3, Table 4) [6, 49]. With this important improvement, SpO2 increases significantly while ED, Legs pain and HR are reduced (Table 4).
This discussion identifies several confident points:
1. Exercise training for overweight respiratory sufferers is difficult. It is dangerous to control efforts just from a clinical perspective. Repeated arterial blood gases studies are sometimes necessary. Usually, the control with peripheral oxygen saturation SpO2 is faster, obligatory and correct.
2. Initially if resting hypoxemia increases during exercise, it must be compulsory under controlled oxygen therapy and requires close individual supervision.
3. The ventilatory automatism to the exercises is generally acquired rather quickly when the CDB is well applied [6, 16, 17, 48, 51]. The contribution of respiratory acidosis to diaphragmatic fatigue to exercise 45 is rectify by the CDB 6,46 (see Figure 3). In fact CDB trained simultaneously inspiratory and expiratory muscular force and endurance of diaphragm [48-51] and, at the same time correct hypercapnia and respiratory acidosis at rest and exercises [39, 40, 48-51].
4. This training improves ventilatory and metabolic conditions. As a result, energy opportunities are increased. [6, 16, 17, 20, 23, 32, 39, 40, 42, 48-51]. All the patients easily realize the elementary and everyday acts of life controlling and adapting his ventilation. [6, 16, 17, 23, 32, 39, 40, 48-51].
Conclusion
Our study demonstrates that the Two-step stool and Bi-level Stairs Climbing (BiSC) training could be an efficient home training of cardiopulmonary function, in overweight subjects with dyspnea. Both tests are low-tech exercise, safe, inexpensive, and available to most patients and physicians; both tests increase greatly endurance capacity and, in the same time, reduce overbreathing, dyspnea and weight. Other studies reported that almost everybody, either healthy or suffering from any pulmonary disability, can benefit from these two training exercises, especially because they can be performed in a home environment.
Acknowledgments
We thank Lahoucine Benhamgar, PhD, epidemiologist researcher, for scientific and statistical advising, assistance and constructive criticism throughout the study; Maria Angeles Montoliu, MD, PhD, for clinical help and advice; Encarnación Abril, Daniel Lopez PT, PhD, Mari Carmen Lareo, PhD for their participation in the clinical trial and implementation of physical protocol techniques; Maeva Sossi for help with graphics and drawings; and the 15 dyspneic overweight subjects who faithfully followed the complete protocol.
References
- Sword, David O. Exercise as a Management Strategy for the Overweight and Obese: where does exercise fit in? Strength and Conditioning J. 2012 Oct;34(5):47-55.
- Vogiatzis I, Terzis G, Nanas S, Stratakos G, Simoes DC, Georgiadou O, et al. Skeletal muscle adaptations to interval training in patients with advanced COPD. Chest. 2005 Dec ;128(6):3838–3845. PubMed PMID: PM16354852.
- World Health Organisation. Global Recommendations on Physical Activity for Health. Geneva; 2010.
- Lavie CJ, O’Keefe JH, Sallis RE. Exercise and the Heart: the Harm of Too Little and Too Much. Curr Sports Med Rep; 2015 Apr;14(2):104–109. Pub- Med PMID: 25757005.
- O’Keefe JH, Franklin B, Lavie CJ. Exercising for health and longevity vs peak performance: different regimens for different goals. Mayo Clin Proc. 2014 Sep;89(9):1171–5. PubMed PMID: 25128073.
- Gimenez M. Managed Ventilation During Chronic Respiratory Failure. Technique, physiopathology and results at rest and during pulmonary exercise. Med Nancy Thesis. 1968;1:260.
- Nikolić I, Majerić-Kogler V, Plavec D, Maloca I, Slobodnjak Z. Stairs Climbing Test with Pulse Oximetry as Predictor of Early Postoperative Complications in Functionally Impaired Patients with Lung Cancer and Elective Lung Surgery: Prospective Trial of Consecutive series of patients. Croat Med J. 49: 50-57. PubMed Central PMID: PMC2269232.
- Sharp JT, Henry JP, Sweany SE, Meadows WR, Pietras RJ. The total work of breathing in normal and obese men. J Clin Invest. 1964 Apr;43(4):728-739. PubMed Central PMCID: PMC289549.
- Stendardi L, Grazzini M, Gigliotti F, Lotti P, Scano G. Dyspnea and legs effort during exercise. Respir Med. 2005 Aug ;99(8):933-942. PubMed PMID: 15950133.
- Gimenez M, Saavedra P, Martin N, Lantarón EM, Polu E, Bach JR. Two Step Stool Aerobic Training for Smokers. Am J Phys Med Rehab. 2014 Jul;93(7):586-594. PubMed PMID: 24508939.
- Gimenez M, Saavedra P, Lantarón EM, Robert JB. Comparison of Two Stairs Climbing Protocols for Smokers. Int J Resp Dis Care Med. 2017 Jan 10;2(1) :8-13.
- Gimenez M, Saavedra P, Lantarón EM, Servera E. Application of the Bi-level Stairs climbing as alternative of Respiratory rehabilitation training in dyspneic smokers; Int J Resp Dis Care Med. 2017 Jun;2(3):22-27.
- Gimenez M, Salinas W, Servera E, Kuntz C. Vo2ax during progressive and constant exercise in sedentary men and women. Eur J Appl Physiol Occup Physiol. 1981;46(3):237-48. PubMed PMID: 7195806.
- Minette A. Questionnaire of the European Community for Coal and Steel (ECSC) on respiratory symptoms: 1987 updating of the 1962 and 1967 questionnaires, for studying chronic bronchitis and emphysema. Eur Respir J. 1989 Feb;2(2):165-77. PubMed PMID :2703044.
- Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin E, et al. Lung volumes and Forced ventilatory flows. Report Working Party Standardization of Lung Function Tests. European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur J Respir Dis. 1993;16:5-40.
- Gimenez M, Servera E, Abril E, Saavedra P, Darias M, Gomez A , et al. Comprehensive Directed Breathing Retraining Improves Exertional Dyspnea for Men with Spirometry within Normal Limits. Am J Phys Med Rehab. 2010 Feb;89(2):90-98. PubMed PMID: 19789433.
- Gimenez M, López D, Abril E, Martin N, Darias M, Gomez A. Comprehensive directed breathing and aerobic-anaerobic muscle training strongly improve a patient with severe COPD by pulmonary emphysema. Fisioterapia. 2010 Oct;32(5):236-42.
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5): 377-81. PubMed PMID: 7154893.
- Aliverti A, Quaranta M, Chakrabarti B, Albuquerque AL, Calverley PM. Paradoxical movement of the lower ribcage at rest and during exercise, in COPD patients. Eur Respir J. 2009 Jan;33(1):49–60. PubMed PMID: 18799505.
- Gimenez M, Mancha AM, Fillion R, Zeguin A. Training with the effort of the Bronchiteux Chronic hypercapniques. Interest of the Association Oxygenothérapie and Comprehensive Ventilation Dirigée. Kinesitherapy Annals. 1976 ;3(n°7):320-333.
- Laird NM, Ware JH. Random-Effects Models for Longitudinal Data. Biometrics. 1982 Dec;38(4):963-974. PubMed PMID: 7168798.
- Vallet G, Ahmaidi S, Serres I, Fabre C, Bourgouin D, Desplan J, et al. Comparison of two training programmer in chronic airway limitation patients: standardized versus individualized protocols. Eur Respir J. 1997 Jan;10(1):114–122. PubMed PMID: 9032502.
- Gimenez M, Servera E, Vergara P, Bach JR, Polu JM. Endurance training in patients with chronic obstructive pulmonary disease: A comparison of high versus moderate intensity. Arch Phys Med Rehab. 2000 Jan;81(1):102-09. PubMed PMID: PM10638884.
- Casaburi R, Patessio A, Ioli F, Zanaboni S, Donner CF, Wasserman K. Reduction in exercise lactic acidosis and ventilation as a result of exercise training in patients with obstructive lung disease. Am Rev Respir Dis. 1991 Jan;143(1):9-18. PubMed PMID: 1986689.
- Bodenheimer T, Lorig K, Holman, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002 Nov;288(19):2469-75. PubMed PMID: 12435261.
- Cahalin LP, Braga M, Matsuo Y, Hernandez ED. Efficacy of diaphragmatic breathing in persons with chronic obstructive pulmonary disease: A review of the literature. J Cardiopulm Rehab. 2002 Feb;22(1):7-21. PubMed PMID: 11839992.
- Dechman G, Wilson CR. Evidence underlying cardiopulmonary physical therapy in stable COPD. Cardiopulm Phys Ther. 2002 Jun;13(2):20-2.
- Gosselink RA, Wagenaar RC, Rijswijk H, Sargeant AJ, Decramer ML. Diaphragmatic breathing reduces efficiency of breathing in patients with COPD. Am J Respir Crit Care Med. 1995 Apr;151(4):1136-42. PubMed PMID: 7697243.
- Perez Bogerd S, Selleron B, Hotton R, Ferrali O, Sergysels R. Chest physiotherapy techniques- can they reduce hyperinflation? Rev Mal Respir. 2009 Dec;26(10):1107-17. PubMed PMID: 20032846.
- Willeput R, Vachaudez JP, Lenders D, Nys A, Knoops T, Sergysels R.. Thoraco-abdominal motion during chest physiotherapy in patients affected by chronic obstructive lung disease. Respiration. 1983 Jun;44(3):204-14. PubMed PMID: 6222449.
- Mador MJ, Kufel TJ, Pineda LA, Sharma GK. Diaphragmatic fatigue and high-intensity exercise in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000 Jan;161(1):118-23. PubMed PMID: 10619807.
- Gimenez M, Saavedra P, Lantarón EM, Alonso B, Polu E, Bernard A. Exertional Dyspnea Comparison in Four Maximal Training Exercises used in Pulmonary Rehabilitation: Continuous versus Bi-Level Responses in Time. Inter J Resp Dis Care & Med. 2017 Jul 1;2(4):28-34.
- Gimenez M, Servera E, Saunier C, Lacoste J. Square-Wave Endurance Exercise Test (SWEET) for training and assessment in trained and untrained subjects. II - Blood gases and acid-base balance. Eur J Apply Physiol Occup Physiol. 1982;49(3):369-377. PubMed PMID: 369-77.
- Coppoolse R, Scholz AMWJ, Baarends EM, Mostert R, Akkermans MA, Janssen PP. Interval versus continuous training in patients with severe COPD: a randomize Clinicae trial. Eur Respir J. 1999 Aug;14(2):258-63. PubMed PMID: 1051398.
- Vogiatzis I, Nanas S, Kastanakis E, Georgiadou O, Papazahou O, Roussos Ch. Dynamic hyperinflation and tolerance to interval exercise in patients with advanced COPD. Eur Respir J. 2004 Sep;24(3):385–390. PubMed PMID: 15358696.
- Hermansen L, Osnes JB. Blood and muscle pH after maximal exercise in man. J Appl Physiol. 1972 Mar ;32(3):304-8. PubMed PMID: 5010039.
- Selvadurai HI, Cooper PJ, Meyers N, Blimkie CJ, Smith L, Mellis CM. Validation of shuttle tests in children with cystic fibrosis. Pediatric Pulmonol. 2003 Feb;35(2):133-38. PubMed PMID: 12526075.
- Sabapathy S, Kingsley RA, Schneider DA, Adams L, Morris NR. Continuous and intermittent exercise responses in individuals with chronic obstructive pulmonary disease. Thorax. 2004 Dec;59(12):1026-1031. PubMed PMID: 15563700.
- Sackner MA, Silva G, Banks JM, Watson DD, Smoak WM. Distribution of ventilation during diaphragmatic breathing in obstructive lung disease. Am Rev Respir Dis. 1974 Aug 7;109(3):331-7.
- Cutillo AC, Renzetti AD. Mechanical behavior of the respiratory system, as a function of frequency in health and disease. Bull Eur Physiopath resp. 1983 Jun;19(3):293-326. PubMed PMID: 6349723.
- Gilbert R, Ashutosh K, Auchincloss JH, Rana S, Peppi D. Prospective study of controlled oxygen therapy. Poor prognosis of patients with asynchronous breathing. Chest. 1977 Apr;71(4):456-62. PubMed PMID: 856543.
- Gimenez M, Uffholtz H, Ferrara G, Plouffe P, Lacoste J. Exercise training with oxygen supply and Comprehensive Directed breathing in patients with chronic airways obstruction. Respiration. 1979;37:157-166. PubMed PMID: 194021.
- Gimenez M, Ûffholtz H, Pham QT, Sobradillo V. Ten years follow up with chronic obstructive lung disease submitted to a program of pulmonary rehabilitation. J R Soc Med. 1978 Jan ;71(1):61-5. PubMed PMID: 633248.
- Jones AYM, Dean E, Chow CCS. Comparison of the oxygen cost of breathing exercises and spontaneous breathing in patients with stable chronic obstructive pulmonary disease. Phys Ther. 2003 May;83(5):424-31. PubMed PMID: 12718708.
- Montori VM, Guyatt GH. What is Evidence-Based Medicine and why should it be practiced? Respir Care. 2001 Nov;46(11):1201-14. PubMed PMID: 11679142.
- Jonson MK, Stevenson RK. Management of an acute exacerbation of copd: are you ignoring the evidence? Thorax. 2002 Oct;57 Suppl 2:II15-II23.
- Sava F, Laviolette L, Bernard S, Breton MJ, Bourbeau J, Maltais F. The impact of obesity on walking and cycling performance and response to pulmonary rehabilitation in COPD. BMC Pulm Med. 2010;10:55. PubMeed Central PMCID: PMC2987952.
- Gimenez M, Polu E, Pinto AM. Ejercicios respiratorios. Técnica y conducta de la Ventilación Dirigida (VD) en reposo y en ejercicio. Las cinco etapas de la VD. In: Gimenez M, Servera E, Vergara P, editors. Prevención y Rehabilitación en patología respiratoria crónica: Fisioterapia, entrenamiento y cuidados respiratorios. 2nd edn. Madrid: Spain, Panamericana; 2004. 131-43.
- Gimenez M, Polu JM, Peñafiel M, Muñoz F. Fisiopatología de los ejercicios respiratorios, Validación fisiopatológica de la Ventilación Dirigida en reposo, y durante ejercicios y Sweetraining. In: Gimenez M, Servera E, Vergara P, editors. Prevención y Rehabilitación en patología respiratoria crónica: Fisioterapia, entrenamiento y cuidados respiratorios. 2nd edn. Madrid: Spain, Panamericana; 2004. 145-56.
- Gimenez M, Uffholtz H, Pham QT, Bernabeu M. Papel de la Ventilación Dirigida en la Rehabilitación Respiratoria: Resultados observados en diferentes grupos de pacientes pulmonares crónicos; Tres casos clínicos larga evolución. In: Gimenez M, Servera E, Vergara P, editors. Prevención y Rehabilitación en patología respiratoria crónica: Fisioterapia, entrenamiento y cuidados respiratorios. 2nd edn. Madrid: Spain, Panamericana; 2004. 157-71.
- Gimenez M, Ros R, Mougel D, Vergara P. Implicaciones de las técnicas de fisioterapia y entrenamiento físico en la patología respiratoria cronica. Fisiopatología con cargas de resistencias inspiratorias. Tres casos clínicos. In: Gimenez M, Servera E, Vergara P, editors. Prevención y Rehabilitación en patología respiratoria crónica: Fisioterapia, entrenamiento y cuidados respiratorios. 2nd edn. Madrid: Spain, Panamericana; 2004. 197-207.