Isolated Genital Psoriasis
El Jouari O1*, Zaougui AA2, Gallouj S1, Senhaji G1, Farih MH2, Mernissi FZ1
1 Department of Dermatology University Hospital Hassan II, Fez, Morocco.
2 Department of Urology University Hospital Hassan II, Fez, Morocco.
*Corresponding Author
Ouiame EL Jouari,
Department of Dermatologym,
University Hospital Hassan II, Fez, Morocco.
Tel: 212645768798
Fax: 212535617687
E-mail: eljouariouiame@gmail.com
Received: June 13, 2018; Accepted: September 24, 2018; Published: September 26, 2018
Citation: El Jouari O, Zaougui AA, Gallouj S, Senhaji G, Farih MH, Mernissi FZ. Isolated Genital Psoriasis. Int J Pediat Health Care Adv. 2018;5(4):84-85. doi: dx.doi.org/10.19070/2572-7354-1800023
Copyright: El Jouari O© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Psoriasis is a chronic, inflammatory skin disorder with a considerable impact on social functioning and personnel relationship. Isolated genital psoriasis is considered a rare manifestation of psoriasis. The manifestations of genital psoriasis may differ from typical genital dermatoses and may mimic other diseases at an early stage. The psychosocial impact of psoriasis often causes more distress than its physical symptoms, and the perception of stigmatization has a detrimental impact on social functioning and self-image. We report a new case in order to recognize this rare variety of psoriasis.
2.Introduction
3.Case Presentation
4.Discussion
5.Conclusion
6.References
Keywords
Psoriasis; Genital; Child.
Introduction
Isolated genital psoriasis is a variety of autoimmune dermatological disease, which can have an onset in all age groups. It is considered a rare manifestation of psoriasis. It is most often diagnosed at an advanced stage [1]. The manifestations of genital psoriasis may differ from typical genital dermatoses and may mimic other diseases at an early stage. Relapsing-remitting course of psoriasis is another factor limiting adequate diagnosis [2]. The objective of this article is to report a case of an isolated genital psoriasis and to review the literature, emphasizing the underdiagnosis of this condition.
Case Presentation
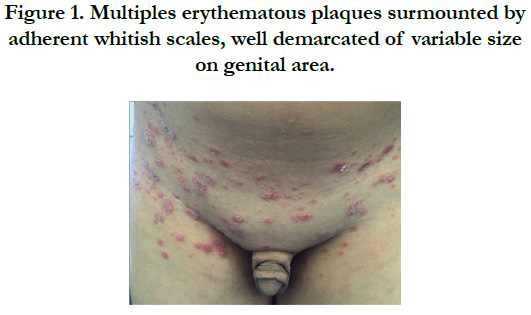
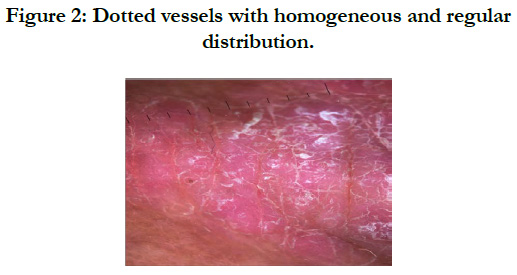
9-year-old child without significant pathological antecedent, including no similar case in the family. He was referred by a urologist for management of erythematous squamous itching genital lesions, evolving since one year by relapses and remissions. Dermatological examination had objected the presence of multiple erythematous plaques surmounted by adherent whitish scales, well demarcated of variable size measuring 2 cm for the largest on genital area [Figure1]. The sign of the methodical scratching of Brocq was positive. Dermoscopy revealed dotted vessels with homogeneous and regular distribution [Figure 2]. The examination of the phaneres and the mucous membranes was normal. The patient was outed on a potent dermocorticoids until the bleaching of the lesions followed by gradual progression. The evolution was favorable with a complete regression of the lesion after 2 months.
Discussion
Psoriasis is a chronic, inflammatory skin disorder with a considerable impact on social functioning and personnel relationship [3]. The isolated presentation of psoriasis solely on genital skin seems to be rare and occurs in only 2-5% of the psoriatic patients [4]. Its pathogenesis explained by the microenvironment of the genital region. Genital skin folds are susceptible to maceration and fissuring due to the combination of moisture, warmth and friction. In addition, the genital area is often exposed to mechanical and chemical irritation [2]. Most patients with genital psoriasis experience localised mild to moderate sensory skin symptoms such as itch, pain and/or burning [5]. Diagnosis of genital psoriasis can usually be made on the basis of its typical clinical appearance that includes symmetrical, welldemarcated, brightly erythematous thin plaques that usually lack the typical dry scaling [2]. Sometimes, lesions may be accompanied by painful rhagades or fissures [5]. The treatment of genital psoriasis is often empirical and generally topical associated to is necessary to avoid irritation in this area [1]. Based on the available literature, the treatments advised for genital psoriasis are on first-line treatment topical corticosteroid. On second- line treatment vitamin D preparation or tar based treatment and the immunomodulators should be regarded as third-line treatment options [2, 6]. Moreover, a suitable choice of remedies is necessary to avoid irritation in this area [1]. Psoriasis affecting genital skin may be associated with considerable morbidity, discomfort and embarrassment and may considerably impair quality of life and psychosexual wellbeing [2]. The psychosocial impact of psoriasis often causes more distress than its physical symptoms, and the perception of stigmatization has a detrimental impact on social functioning and self-image [3].
Conclusion
Isolated genital psoriasis is considered an embarrassing condition and is often misjudged as a sexually transmitted disease or allergic reaction due to low social awareness of the disease. The diagnosis and treatment of genital psoriasis may be difficult and often requires a multidisciplinary approach.
References
- Czuczwar P, Stępniak A, Goren A, Wrona W, Paszkowski T, Pawlaczyk M, et al. Genital psoriasis: a hidden multidisciplinary problem—a review of literature. Ginekol Pol. 2016;87(10):717-721. doi: 10.5603/GP.2016.0074. PubMed PMID: 27958625.
- Meeuwis KA, De Hullu JA, Massuger LF, Van De Kerkhof P, Van Rossum MM. Genital psoriasis: a systematic literature review on this hidden skin disease. Acta Derm Venereol. 2011 Jan;91(1):5-11. doi: 10.2340/00015555-0988. PubMed PMID: 20927490.
- Ryan C, Sadlier M, De Vol E, Patel M, Lloyd AA, Day A, et al. Genital psoriasis is associated with significant impairment in quality of life and sexual functioning. J Am Acad Dermatol. 2015 Jun;72(6):978-83. doi: 10.1016/j. jaad.2015.02.1127. PubMed PMID: 25824273.
- Van de Kerkhof PCM. Clinical Features. Textbook of Psoriasis. Oxford : Blackwell Publishing Ltd ; 2003. p. 3-29.
- Meeuwis KA, de Hullu JA, IntHout J, Hendriks IM, Sparreboom EE, Massuger LF, et al. Genital psoriasis awareness program: physical and psychological care for patients with genital psoriasis. Acta Derm Venereol. 2015 Feb;95(2):211-6. doi: 10.2340/00015555-1885. PubMed PMID: 24806592.
- Dauendorffer JN, Renaud-Vilmer C, Cavelier-Balloy B. Genital psoriasis in humans. Ann Derm Venereol. 2014 Jan 1;141(6):466-472.