A Yellow and Benign Tumor in a Newborn
A Nassiri*, K Moustaide, H Baybay, Fz Mernissi
Dermatology Department, Hassan II Hospital University, Fez. Morocco.
*Corresponding Author
Aicha Nassiri,
Dermatology Department,
Hassan II Hospital University, Fez. Morocco.
Tel: +212650599689
Fax: +2120535511616
E-mail: aichanassiri6@gmail.com
Received: February 28, 2018; Accepted: March 26, 2018; Published: March 28, 2018
Citation: A Nassiri, K Moustaide, H Baybay, Fz Mernissi. A Yellow and Benign Tumor in a Newborn. Int J Pediat Health Care Adv. 2018;5(2):79-80. doi: dx.doi.org/10.19070/2572-7354-1800021
Copyright: A Nassiri© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
2.Case Report
3.Discussion
4.Conclusion
5.References
Introduction
The sebaceous hamartoma of Jadassohn (HSJ) is a congenital malformation most often discovered during infancy. Early surgical excision is motivated by the rare risk of malignant tumor development, especially basal cell carcinoma during puberty [1]. We report the case of a Jadassohn Hamartoma.
Case Report
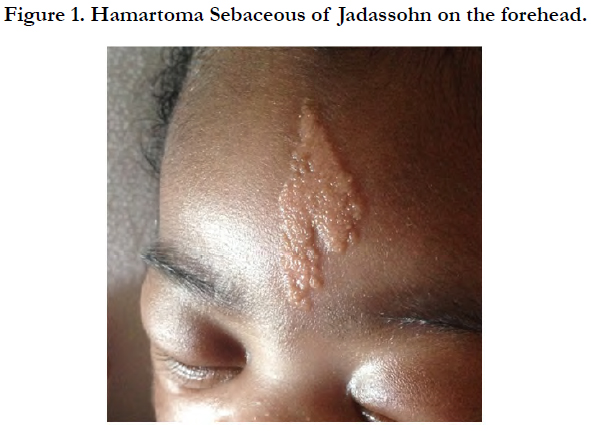
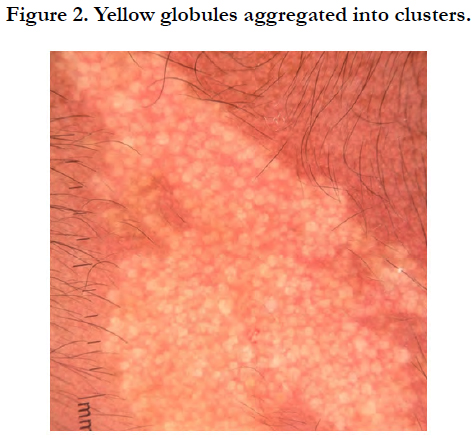
In a Newborn at J4 hospitalized in neonatal reanimation for respiratory distress following premature birth, Our opinion was solicited for congenital medio-frontal lesion. On dermatological examination, it was a yellowish medial-length plaque, about 4 cm long, well-defined, with a regular border, and smooth surface. In dermoscopy, there were yellow globules aggregated into clusters without special vascularization.
The neurological examination was completely normal and no further explorations were made. After consultation with pediatricians, surgeons and the parents the decision taken was to monitor the sebaceous hamartoma instead of excision.
Discussion
Sebaceus Hamartoma of Jadassohn is a congenital anomaly first described by a dermatologist Josef Jadassohnin 1895.
Sebaceous Hamartoma of Jadassohn is a rare congenital anomaly that can lead to cosmetic deformity, alopecia or malignant transformation in rare circumstances. The lesion is usually present at birth, widens slowly with age, and usually develops more rapidly during puberty hormonal surge [2] (Figure 1).
During infancy, sebaceous hamartoma of Jadassohn typically appears as a smooth or velvety yellow-orange well-circumscribed plaque (Figure 2). Classically, it is located on the vertex of the scalp but has been described on other areas such as the face or neck [3]. At puberty, hormonal changes cause proliferation and hyperplasia of the lesion and lead to a larger and more verrucous appearance that can be come quite large [4]. Later in life, the lesions can develop benign or malignant appendageal tumors that cause further disfigurement.
Malignant transformations have been reported with an average incidence of 8% and ranging from 0% to 22%, most commonly basal cell carcinoma, although there is some controversy of falsely high estimations, given the misdiagnosis of trichoblastoma that appear histologically similar to basal cell carcinoma in earlier reports [5, 6].
Few publications have described the dermoscopic aspect of this hamartoma, which could be important to differentiate it mainly from sebaceous hyperplasia and sebaceous adenoma, especially since the evolution of HSJ can become complicated with degeneration [3].
The timing of surgical intervention is controversial. While smaller lesions may be technically easier to excise, younger patients may not be amenable to local anesthesia or able to safely tolerate a general anesthetic. Secondary tumor transformation seems to be seen almost exclusively in adults, as one retrospective analysis found that 96% of all nevus sebaceous (NS) - derived malignant tumors occurred in patients older than 18 years and the remaining 4% in patients aged 11 to 17 years [6-8]. This has led to the popularized reasoning to excise prior to pubertal enlargement and when local and general anesthesia are well tolerated versus clinically observing until malignant features develop [3]. Therapeutic management of NS includes full-thickness excision with clear margins. CO2 lasers have been shown to enhance cosmesis but can only reach the papillary dermis and are therefore not recommended because of the possibility of malignant degeneration of remaining cells in the lower dermis [5].
Conclusion
Sebaceous hamartoma of Jadassohn is a rare congenital abnormality that can lead to cosmetic deformity, alopecia, or malignant transformation in rare circumstances. The lesion is usually present at birth, slowly enlarges with age, and typically grows most rapidly during the pubertal hormonal surge. The pre disposition to epithelial neoplasms in sebaceous hamartoma of Jadassohn is well established; most tumors occur in adults and are benign.
No definitive consensus on surgical intervention versus close observation exists. In the absence of worrisome signs for malignant transformation, management of sebaceous hamartoma of Jadassohn is a decision best made by the child, his or her family, and the surgeon, based on their expectations of oncologic safety, and the understanding of more extensive excision required should increased growth occur.
References
- Kelati A, Baybay H, Gallouj S, Mernissi FZ. Dermoscopic Analysis of Nevus Sebaceus of Jadassohn: A Study of 13 Cases. Skin Appendage Disord. 2017 May;3(2):83-91. PubMed PMID: 28560218.
- Kamyab‐Hesari K, Seirafi H, Jahan S, et al. Nevus sebaceus: a clinicopathological study of 168 cases and review of the literature. Int J Dermatol. 2016 Feb;55(2):193-200. PubMed PMID: 26381137.
- Al Hammadi, Lebwohl MG. Nevus sebaceus. 2017 [cited 2017 May 20]. Available from: http://emedicine.medscape.com/article/1058733-overview.
- Chepla KJ, Gosain AK. Giant nevus sebaceus: definition, surgical techniques, and rationale for treatment. Plast Reconstr Surg. 2012 Aug;130(2):296e- 304e. PubMed PMID: 22842426.
- Moody MN, Landau JM, Goldberg LH. Nevus sebaceous revisited. Pediatr Dermatol. 2012 Jan-Feb;29(1):15-23. PubMed PMID:21995782.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014 Feb;70(2):332-7. PubMed PMID: 24268309.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000 Feb;42(2 Pt 1):263-8. Pub- Med PMID: 10642683.
- Labbé D, Badie BM, Petit F. Sebaceus nevus of Jadassohn. Apropos of 62 surgically treated cases and review of the literature. Rev Stomatol Chir Maxillofac. 1999 Oct;100(4):175-9. PubMed PMID: 10599124.