Do Ophthalmologists in India Over Prescribing Topical Antibiotics in Acute Infectious Conjunctivitis?
Kauser H1*, Garg R2
1 Associate Professor, Department of Ophthalmology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
2 Internship, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
*Corresponding Author
Dr. Hina Kauser,
Associate Professor, Department of Ophthalmology,
Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
Tel: 9811760127
E-mail: hina3kauser@yahoo.co.in
Received: June 13, 2019; Accepted: July 08, 2019; Published: August 02, 2019
Citation: Kauser H, Garg R. Do Ophthalmologists in India Over Prescribing Topical Antibiotics in Acute Infectious Conjunctivitis?. Int J Ophthalmol Eye Res. 2019;7(2):400-403. doi: dx.doi.org/10.19070/2332-290X-1900081
Copyright: Kauser H© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: To assess the prescribing trends of topical antibiotics for acute infectious conjunctivitis among Ophthalmologists in India and to analyze whether they are using them appropriately or not.
Design: Ophthalmologists from various states in India were surveyed by mail using a questionnaire on antibiotic use in acute infective conjunctivitis.
Methods: Two hundred fifty ophthalmologists from different parts of India were given printed questionnaire via email. Only 75 responded to the mail. Results of categorical variables were recorded as counts and percentages.
Result: The commonest indication for prescribing topical antibiotics was infective conjunctivitis. The most commonly prescribed topical antibiotic was moxifloxacin (65%). The frequency of instillation was 4 times a day by 66.6%. All 75 participants agreed that majority of the cases were viral. 93.4% had the knowledge that majority of infective conjunctivitis are viral in origin and self limiting and that there is no need of antibiotic still then 84% would prescribe antibiotic in viral conjunctivitis. 60% had the opinion that acute bacterial conjunctivitis are mild and resolve on their own without complications. But in spite of this knowledge 94.7% advised an antibiotic in cases of bacterial conjunctivitis. Wait and see policy was adopted by only 8% and 40% took time for patient education.
Conclusion: Acute conjunctivitis is mainly viral in origin and self limiting and even among those with a bacterial cause, antibiotics are seldom required. Most of the ophthalmologist surveyed had this knowledge but there was knowledge action mismatch which may promote antibiotic resistance and increase medical costs.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Conclusions
7.References
Keywords
Acute Conjunctivitis; Antibiotic Resistance; Viral Conjunctivitis; Antibiotic Overuse; Bacterial Conjunctivitis.
Introduction
Inflammation or infection of the conjunctiva is known as conjunctivitis. It is characterized by dilatation of conjunctival vessels, hyperemia and edema of the conjunctiva and typically associated with discharge [1]. Conjunctivitis affects many people and imposes economic burden. Approximately 6 million people were affected annually with acute conjunctivitis in the United States [2]. The cost of treating bacterial conjunctivitis alone was estimated to be $377 million to $857 million per year [3]. Irrespective of the cause of conjunctivitis, in many US state health departments, students are required to be treated with topical antibiotic eye drops before returning to school [4].
The conjunctivitis prevalence varies on the basis of underlying cause, which may be influenced by the patient’s age and the season of the year. Viral conjunctivitis is the most common cause of infectious conjunctivitis contributing up to 80% cases. Conjunctivitis is usually a self-limiting infectious disease. Antibiotics are seldom necessary to treat conjunctivitis and only a minority of patients benefit from antibiotic therapy [5]. Acute bacterial conjunctivitis is mild and resolve on their own without complications. The complications if occur are mild and very rare and there is no evidence that antibiotics reduce rates of complications [6].
A wide spectrum of topical antibiotics is now available to our ophthalmologists. And the current trend of prescribing broad spectrum topical antibiotics by Ophthalmologists in India is alarming. Antibiotic use is mostly prophylactic, as ophthalmologist often do not have data from culture analysis [7]. This antibiotic overuse can lead to resistance among ocular surface flora leading to infections that can become difficult to treat, increase the chances of severe ocular damage and vision loss.
The ultimate goal of drug utilization research is to facilitate the rational use of drugs in populations and to provide insight into the efficiency of drug use and the results of these researches can be used to help to set priorities for the rational allocation of health care funds [8].
Concerns regarding benefits and risks associated with drug use and increase burden of Health care costs have shown a tremendous increase, making periodical identification of drug usage pattern extremely important.
Therefore, this study was undertaken with the aim to evaluate antibiotic utilization by ophthalmologists in acute conjunctivitis, a disease where antibiotics are seldom required for its treatment. We assessed how frequently acute conjunctivitis patients were prescribed topical antibiotics. These potentially harmful practices may promote antibiotic resistance and increase medical costs.
Materials and Methods
Two hundred fifty ophthalmologists who were known to me and settled in different parts of India were given questionnaire on antibiotic use in acute infective conjunctivitis via email. Out of 250 ophthalmologists only 75 responded to the mail. Data was entered into Microsoft Excel spread sheet and analysis was done. Results of categorical variables were recorded as counts and percentages. The results were compared with current recommendations.
Results
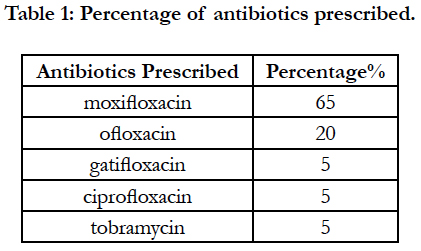
Out of 250 ophthalmologists from different states of India who were given a questionnaire, only 75 responded to the email. A total of 75 ophthalmologists were surveyed. Among them 55 ophthalmologists (73.4%) were consultants and 20(26.6%) were residents. 40 %( 30) among them were practicing in Government hospitals and the rest 60% (45) were practicing in private setup. The commonest indication for prescribing topical antibiotics by all 75 participants (100%) was infective conjunctivitis. The most commonly topical antibiotic prescribed was moxifloxacin (65%) followed by ofloxacin (20%), gatifloxacin (5%), ciprofloxacin (5%), tobramycin (5%). Those in Government hospitals prescribed more of ciprofloxacin and tobramycin whereas ofloxacin and moxifloxacin were more used in private institutions (Table 1).
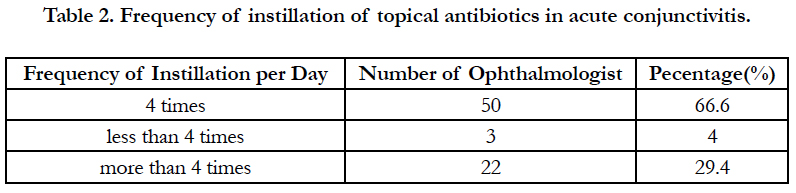
The frequency of instillation was 4 times a day by 66.6% (50) of the participants. 29.3% (22) prescribed more than 4 times and 4% (3) prescribed less than 4 times a day (Table 2). No statistical correlation was found with the type and frequency of instillation of antibiotic prescribed in different states of India and by the experience of the ophthalmologist, whether consultant or resident.
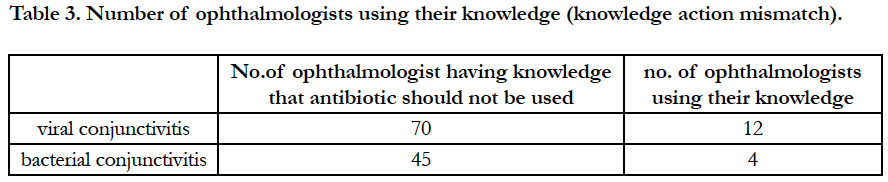
All 75 participants (100%) agreed that majority of the cases of acute infective conjunctivitis were of viral origin followed by bacterial conjunctivitis. 93.4% of the ophthalmologist (70) have the knowledge that majority of infective conjunctivitis were viral in origin and are self-limiting and that there is no need of antibiotic prescription. 60% of the participants (45) had the opinion that acute bacterial conjunctivitis are mild and resolve on their own without complications. 84% (63) prescribed an antibiotic drops in viral conjunctivitis cases and 16% (12) would never prescribe an antibiotic when suspecting conjunctivitis of viral origin. 94.7% (71) of the participants in the survey advised an antibiotic therapy in cases of bacterial conjunctivitis and 5.3% (4) did not prescribe any antibiotic.
93.4% of the total ophthalmologist (70) have the knowledge that majority of infective conjunctivitis were viral in origin and are self-limiting and that there is no need of antibiotic prescription but only 16% (12) of the participants were not prescribing antibiotic drops in viral conjunctivitis. 60% of the participants (45) had the opinion that acute bacterial conjunctivitis are mild and resolve on their own without complications but 5.3% (4) were not prescribing antibiotics in acute bacterial conjunctivitis (Table 3).
Wait and see policy was adopted by only 8% (6) of the ophthalmologists while others 92% (69) started antibiotic therapy in the first visit of the patient presenting with acute infective conjunctivitis. Thirty (40%) of the Ophthalmologists took time for patient education, whereas 45 (60%) did not.
Discussion
It is not possible to comment on rational drug use or suggest actions to improve prescribing trends without understanding the way how drugs are being prescribed. Therefore collecting information on prescribing trends is the role model of any auditing system [9].
Among the antibiotics, fluoroquinolone was the most commonly prescribed antibiotic in our study , which coincides with the findings of earlier studies [10-12]. Polymyxin-bacitracin (eg, Polysporin) was advised for the treatment of conjunctivitis and not fluoroquinolones in one study [13]. To address the rising antibiotic resistance, ophthalmologists readily accept and indiscriminately use newer expensive and broad spectrum antibiotics which further contribute to increase rates of antimicrobial resistance and health care costs [14]. In our study also fourth generation fluoroquinolones, moxifloxacin was commonly prescribed by 65% ophthalmologists while other studies favor that the antibiotic choice should be usually empiric. There is no clinical evidence suggesting the superiority of any particular antibiotics, the least expensive and most convenient option should be selected. Even Povidone-iodine 1.25% ophthalmic solution could be considered as it is as effective as topical antibiotic therapy for treating bacterial conjunctivitis when antibiotics access is limited like in developing countries [15].
According to the recommendations of the American Academy of Ophthalmology (2013), immediate antibiotic therapy was not advised when the cause of conjunctivitis was unknown [16] but in our observations 92 % ophthalmologists (69) started antibiotic therapy in the first visit of the patient presenting with acute infective conjunctivitis. The recommended management strategy is to delay antibiotic use and promote supportive care such as frequent eye washing with sterile water, warm water compresses, proper hand and eyelid hygiene, and temporary use of artificial tears for comfort. If the symptoms of conjunctivitis do not begin to improve within 2 days of proper supportive management, the recommendation is to then begin a topical antibiotic [17]. Infective conjunctivitis should be managed conservatively and antibiotics should be prescribed either after a delayed period if symptoms do not improve within 3 days of onset or not at all [18].
The frequency of instillation in our study was 4 times a day by 66.6% (50) of the participants. 29.3% (22) prescribed more than 4 times and 4% (3) prescribed less than 4 times a day. 33.3% of consultants were prescribing topical antibiotic for conjunctivitis at frequencies more than or less than the recommendation of four times a day which should be avoided to prevent generation of drug resistance. Compliance with the duration (7-10 days) the antibiotics are prescribed is also particularly important to prevent drug resistance.
93.4% of the total ophthalmologist (70) have the knowledge that majority of infective conjunctivitis were viral in origin and are self-limiting and that there is no need of antibiotic prescription but only 16% (12 )of the participants were not prescribing antibiotic drops in viral conjunctivitis. 60% of the participants (45) had the opinion that acute bacterial conjunctivitis are mild and resolve on their own without complications but 5.3% (4) were not prescribing antibiotics in acute bacterial conjunctivitis (Table 3). There was so much knowledge action mismatch in our study group of ophthalmologist i.e. only 16% ophthalmologist were utilizing their knowledge (that there is no need of antibiotics) in viral conjunctivitis cases and 5.3% participants were utilizing their knowledge in bacterial conjunctivitis cases. 84% (63) of the participants prescribed an antibiotic drops in viral conjunctivitis cases. 94.7% (71) of the participants in the survey advised an antibiotic therapy in cases of bacterial conjunctivitis. Most of them were prescribing antibiotics in acute conjunctivitis unnecessarily which is not only costly but it also leads to disruption of the microbial flora in the eye and leading to antibiotic resistance. Topical antibiotics can induce bacterial resistance not only ocular but also at extra ocular sites like topical tetracycline use in eye causes increase nasopharyngeal pneumococcal resistance [19].
Acute conjunctivitis is a common ocular infection and current treatment practice followed by ophthalmologists in India appears to be inappropriate and not evidence based.
This study opens our eye in the field of overprescribing antibiotics that we think few are aware of. Why these ophthalmologists were overprescribing topical antibiotics in acute conjunctivitis? We think it is clinically difficult to differentiate viral from bacterial conjunctivitis and this inability to quickly find out the etiology of acute conjunctivitis leads with just in case antibiotic prescription. A rapid, in-office immunodiagnostic test using antigen detection is available for adenovirus, the most common cause of viral conjunctivitis [20]. It is not sensitive (39%) in clinical settings and is not used widely [21]. There are also no tests available routinely for diagnosing bacterial conjunctivitis. This lack of diagnostic certainty might be the reason for over prescribing antibiotics in acute conjunctivitis.
Patient expectations and preferences also play a role in overprescribing antibiotics. There is a misconception in patients that antibiotics are not so harmful [22], and it is better to be under cover for possible bacterial cause [23]. Ophthalmologists also believe that prescribing antibiotics improves patient satisfaction [24].
Conclusion
Acute conjunctivitis is mainly viral in origin and self limiting and even among those with a bacterial cause, antibiotics are seldom required. Most of the ophthalmologist surveyed had this knowledge but there was knowledge action mismatch which may promote antibiotic resistance and increase medical costs.
The results of this study could be used to change prescribing pattern for acute conjunctivitis. BUT HOW? The patient should be educated about measures that will help reduce the spread of the infection and promote supportive care, such as frequent eye washing with sterile water, warm water compresses, proper hand and eyelid hygiene. Ophthalmologists and primary health care takers should be encouraged to adopt evidence-based practices for acute conjunctivitis. There should be better and proper diagnostic aids, awareness should be created among ophthalmologists and primary health care takers of the need for rational use of antibiotics. National regulatory agencies should impose restrictions on over-the-counter sale of antibiotics. We need a new approach for the diagnosis and management of acute conjunctivitis to reduce the cost per prescription and the worldwide threat of antimicrobial resistance.
References
- Leibowitz HM. The red eye. N Engl J Med. 2000; 343(5):345–351.
- Udeh BL, Schneider JE, Ohsfeldt RL. Cost effectiveness of a point-of-care test for adenoviral conjunctivitis. Am J Med Sci. 2008; 336(3):254–264.
- Smith AF, Waycaster C. Estimate of the direct and indirect annual cost of bacterial conjunctivitis in the United States. BMC Ophthalmol. 2009; 9:13.
- Ohnsman CM. Exclusion of students with conjunctivitis from school: policies of state departments of health. J Pediatr Ophthalmol Strabismus. 2007; 44(2):101–105.
- Sheikh A, Hurwitz B, van Schayck CP,McLean S, Nurmatov U.Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2012;(9)
- Jefferis J, Perera R, Everitt H,van Weert H, Rietveld R, Glasziou P, et al. Acute infective conjunctivitis in primary care: who needs antibiotics? An individual patient data meta-analysis. Br J Gen Pract. 2011; 61(590):542-548.
- Oydanich M, Dingle TC, Hamula CL, Ghisa C, Asbell P. Retrospective report of antimicrobial susceptibility observed in bacterial pathogens isolated from ocular samples at Mount Sinai Hospital, 2010 to 2015. Antimicrob Resist Infect Control 2017; 6:29
- Introduction to drug utilization research—World Health Organization. Available from: apps.who.int/medicinedocs/pdf/ s4876e/s4876e.pdf. [Last accessed on 2017 July 24].
- Desalegn AA. Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, south Ethiopia: A cross-sectional study. BMC Health Serv Res 2013; 13:170|
- Jadhav PR, Moghe VV, Deshmukh YA. Drug utilization study in ophthalmology outpatients at a tertiary care teaching hospital. ISRN Pharmacol 2013; 2013:768792.
- Dutta SB, Beg MA, Mittal S, Gupta M. Prescribing pattern in ophthalmological outpatient department of a tertiary care teaching hospital in Dehradun, Uttarakhand: A pharmaco-epidemiological study. Int J Basic Clin Pharmacol 2014; 3:547-2.
- Nehru M, Kohli K, Kapoor B, Sadhotra P, Chopra V, Sharma R. Drug utilization study in outpatient ophthalmology department of Government Medical College Jammu. JK Science 2005; 7:149-51.
- Maxwell D.M.Treatment of conjunctivitis. Can Fam Physician. 2010 Jan; 56(1): 18.
- Hogerzeil HV. Promoting rational prescribing: an international perspective. British Journal of Clinical Pharmacology. 1995; 39(1):1–6.
- Isenberg SJ, Apt L, Valenton M, et al. A controlled trial of povidone-iodine to treat infectious conjunctivitis in children. Am J Ophthalmol. 2002; 134(5):681-688.
- American Academy of Ophthalmology. Choosing wisely: Five things physicians and patients should question. Available from: http:// www.choosingwisely. org/societies/american-academy-ofophthalmology. 2013. [Last accessed on 2018 Jan 24]
- Epling J. Bacterial conjunctivitis .Clin Evid (Online) 2007. pii: 0704.
- Visscher KL1, Hutnik CM, Thomas M Evidence-based treatment of acute infective conjunctivitis: Breaking the cycle of antibiotic prescribing.Can Fam Physician. 2009 Nov; 55(11):1071-5.
- Gaynor BD, Chidambaram JD, Cevallos V, Miao Y, Miller K, Jha HC,et al. Br J Ophthalmol. 2005 Sep; 89(9):1097-9.
- Sambursky R, Tauber S, Schirra F, Kozich K, Davidson R, Cohen EJ. The RPS adeno detector for diagnosing adenoviral conjunctivitis. Ophthalmology. 2006; 113(10):1758-1764.
- Kam KY, Ong HS, Bunce C, et al. Sensitivity and specificity of the Adeno-Plus point-of-care system in detecting adenovirus in conjunctivitis patients at an ophthalmic emergency department: a diagnostic accuracy study. Br J Ophthalmol. 2015; 99(9):1186-1189.
- Roberts RM, Albert AP, Johnson DD, Hicks LA. Can improving knowledge of antibiotic-associated adverse drug events reduce parent and patient demand for antibiotics? Health Serv Res Manag Epidemiol. 2015; 2:2333392814568345.
- Sanchez GV, Roberts RM, Albert AP, et al. Effects of knowledge, attitudes, and practices of primary care providers on antibiotic selection, United States. Emerg Infect Dis. 2014; 20(12):2041-2047.
- Lee GC, Reveles KR, Attridge RT, Lawson KA, Mansi IA, Lewis JS 2nd,et al. Outpatient antibiotic prescribing in the United States: 2000 to 2010. BMC Med. 2014; 12:96.