Manual Small Incisional Cataract Surgery Learning Curve: Observational Comparison of Three Trainee Training
Anita T Girish1, Soumya HV2, Anuj K Singal3*, Pooja A Angadi3, Raghavendra Reddy A3, Chandramouli A4
1 Consultant Vitreoretinal Surgeon, Vivekananda Institute of Medical Sciences, Sarat Bose Road Kolkata, India.
2 Senior Resident,Vivekananda Institute of Medical Sciences, Sarat Bose Road Kolkata, India.
*Corresponding Author
Dr. Anuj Kumar Singal,
Junior Resident, Department of Ophthalmology,
JSS Medical College and Hospital, MG Road,
Mysore, Karnataka, Pin - 570004, India.
Tel: +91-9212762478/7219877735
E-mail: dranujsinghal@hotmail.com
Received: October 03, 2018; Accepted: October 29, 2018; Published: October 31, 2018
Citation: Anita T Girish, Soumya HV, Anuj K Singal, Pooja A Angadi, Raghavendra Reddy A, Chandramouli A. Manual Small Incisional Cataract Surgery Learning Curve: Observational Comparison of Three Trainee Training. Int J Ophthalmol Eye Res. 2018;6(6):393-396. doi: dx.doi.org/10.19070/2332-290X-1800079
Copyright: Anuj K Singal© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: To assess and compare the learning curve of three ophthalmology trainee in their post graduate training for Manual Small Incisional Cataract Surgery (MSICS) over 50 cases each.
Methods: The study was done over a period of 12 months and a total of 150 patients were operated with each of the three trainee surgeon operating 50 cases. All the surgeries were performed under the guidance of expert cataract surgeons. The Preoperative, Intraoperative, Postoperative day 1, day 7 and day 42 status of the patients were noted and evaluated.
Results: Mean age of patients was 59.83 years +/- 7.56 years. Right eye was operated upon in 81 eyes. Males comprised 71 patients. Posterior capsule rent occurred in 13 cases. Intraocular lens was placed in all cases. Overall, 56 cases were mature cataract. The residents started performing independent surgery after the 25th case and completed at least ten of the last 15 cases provided to them. All patients achieved a BCVA of 20/40 or better at the end of six weeks.
Conclusion: The study demonstrates that 50 cases operated under proper guidance over a few months is sufficient for a trainee to learn MSICS.
2.Abbreviations
3.Introduction
4.Materials and Methods
4.1 Pre-Operative
4.2 Intraoperative
4.3 Post-Operative
5.Result
6.Discussion
7.Conclusion
8.Acknowledgements
9.References
Keywords
Cataract Extraction; Learning Curve; Small Incisional Cataract Surgery; Ophthalmology Trainee.
Abbreviations
MSICS: Manual Small Incisional Cataract Surgery; EHR: Electronic Health Record; CCC: Continuous Curvilinear Capsulorhexis; A/C: Anterior Chamber; PC: Posterior Capsule; ANOVA: Analysis of Variance; DM: Descemet Membrane; IOL: Intraocular Lens.
Introduction
The most common elective surgery performed worldwide is Manual Small Incision Cataract Surgery or MSICS. It has universal applicability, as it is economical and can be performed for all grades of cataract [1]. It has perhaps the most use in large volume cataract surgery centers [2]. Being cheap and fast with less complications, it has become the surgery of choice for all types of cataracts in developing countries [3].
Cataract surgery like any other surgery has a chance of having complications. The chance of the same decreases by 1% with each successive case [4] and thus understanding the different milestones in its learning curve is very important to impart a good training to trainee MSICS surgeons.
Materials and Methods
The study was an observational study from the data extracted over one year from the surgical logbook of the trainee of a tertiary care hospital in south India. These trainees were postgraduate students in their second year of residency at a tertiary hospital of south India. The trainee under the supervision of experienced cataract surgeons operated these cases. If needed, the Electronic Health Record (EHR) was looked into.
The Declaration of Helsinki was adhered to and was approved by the ethical committee. Informed written consent was collected from all patients prior to their enrolment in this study.
The trainees operated a total of 150 eyes of 150 cases, 50 eyes per trainee under the guidance of senior experienced surgeons using side view observoscope and Television for guidance. All the pre-operative patient data, Intraoperative complications and difficulties faced and Post-operative outcome was recorded and compiled.
The trainees were experienced in basic extraocular surgeries such as lid suturing and chalazion procedures. A trainee was considered to have been trained sufficiently when he/she was able to complete at least ten MSICS cases. All cases operated were charitable cases that were harvested from camps conducted outside the hospital. All surgeries and medicines were given free to the patient.
The patients were evaluated one day beforehand for detailed preoperative assessment. This examination included Visual Acuity, IOL power calculation using SRK/T formula, fundoscopy, slit lamp examination and physician’s review ifindicated. Lens Opacities Classification System III or LOCS III was used to grade the cataract. If patients had systemic diseases then they were certified fit by the physician before proceeding for the surgery. Complicated cases such as poorly dilating pupils, patients with pseudoexfoliation, complicated cataracts were not taken up by the trainees.
Pupils were dilated on the day of the surgery. Medications used to achieve the same was Tropicacyl plus (0.8% Tropicamide and 5% Phenylephrine by Sunways Pvt, Mumbai, India). Omeflox-KT Eye drops (Omefloxacin 3 mg/ml and Ketorolac 5 mg/ml, Entod Pharmaceuticals Ltd) was instilled for antibiotic prophylaxis and to maintain intraoperative mydriasis. The regional anesthesia was given by injecting 4 - 6ml of Lox 2% which is a combination of Lignocaine 2% and 1:200,000 adrenaline along with 0.5% Sensorcaine (bupivacaine 0.5%, Neon Lab Ltd, Mumbai, India). To increase the tissue perfusion, Hyalase (15 units/ml Hyaluronidase, Wockhardt, USA) was also added. The resident himself gave this. Gentle massage was given to the globe if necessary to make the eyeball soft. All cases were operated using Zeiss OPMI LUMERA 300 microscope.
All cases underwent MSICS by modified Blumenthal technique [5]. A fornix based conjunctival peritomy was done with Vestcott’s scissors. Bleeding vessels were cauterized using a wet cautery. A linear scleral incision about 2mm behind the surgical limbus taken. The length of the incision was about 6.5mm long (as measured using Castroviejo's callipers) was made with a crescent knife or a 11 no. Blade.
A crescent knife (Sharpedge instruments Pvt, India) was used to make a tunnel of about a millimetre into clear cornea and was extended sideways. This helped in creating side pockets on both the sides of the tunnel. Side port was made at 9 o’clock position. Trypan blue was injected to stain the anterior capsule. Continuous curvilinear capsulorhexis (CCC) was done with a bent 26G needle.
In occasional cases where CCC was not completed properly then completion was done with a can-opener technique. An entry blade which was an angled 45 degrees microkeratome was used to enter the anterior chamber (A/C). Using the same blade the wound was extended. This gave an inverted trapezoid opening.A dispersive viscoelastic of 2% methylcellulose was used to maintain the anterior chamber.
This was followed by Hydro dissection using a 27 gauge cannula and Ringer’s lactate solution. After prolapsing the nucleus, a sandwich technique involving a Vectis and Sinskey hook were used to deliver the nucleus. The corrugated vectis was placed below the dislocated lens and the Sinskey hook placed above and a constant gentle pressure was given on the outer lip of the wound so as to pull the nucleus out of the wound. Remaining epi-nucleus plate was removed by Visco-expression. Left over cortical matter was aspirated using simcoe cannula. The anterior chamber was then reformed using a Viscoelastic. A rigid intraocular lens (Appasamy Associates Pvt, Puducherry, India) of 6 mm diameter was then implanted.
In cases where sufficient mydriasis was not achieved, intracameral epitrate (0.1ml of adrenaline 1:1000) was used. Most wounds were self sealing but the few which had premature entries or if an incompetent valvular system was observed then the trainee would close the wounds using interrupted 10/0 nylon sutures. The side port was kept sealed by stromal hydration.
Sub conjunctival 0.3ml Gentamycin and 0.3ml dexamethasone 4mg/ml was given at the end of the surgery. The operated eye was then patched and bandaged. VA and slit lamp examination was done on the first day post-operative day. Patients with satisfactory results were then discharged on topical Oflacin- Dx (Ofloxacin 0.3%, dexamethasone 0.1% combination, Micro Labs Pvt, Bangalore, India). Patients with postoperative complications were given appropriate treatment. Patients having corneal edema were given 5% Hypersol (Sodium Chloride, Jawa Pharm, Pvt, Jaipur, India).
Usually operation theatre was twice a week and chances were given as per availability of patients. A supervisor was always there to assist and intervene whenever it became necessary. This supervisor was an expert cataract surgeon and may occasionally provide verbal suggestion. If any of the following situations occurred: an extension of capsulorhexis margin, repeated piris prolapse, three continuous unsuccessful trials in same step or residents’ active request for help, the supervisor would take over the surgery. If possible then the resident was allowed to resume as a primary surgeon. However, if in case of any major complication such as posterior capsule (PC) rupture, the remaining surgery would be taken over by the supervisor.
The patients were observed in the hospital for 2 days post-operative and then called on post-operative Day 7 and seen in camps on post-operative day 42. All follow up visits included a thorough check-up including visual acuity assessment, anterior chamber examination using a slit lamp.
Complete collection of data would be done after the surgery. A record of whether the surgery was completed by the resident or there was a requirement of assistance of supervisor and if required then at which step of the procedure. A record of all intraoperative complications was also noted.
Both descriptive and inferential statistics were employed for data analysis using IBM SPSSTM version 22.0. The Descriptive statistics was used to calculate Frequencies, percentages, mean and standard deviation. The Independent-Samples t test and fisher test was used to compare means for two groups, Analysis of variance (ANOVA) was used to compare intergroup and intragroup variation. Tukey's honest significance test was done to compare multiple pair of groups. P value less than 0.05 was considered significant.
Results
The trainees operated a total of 150 eyes of 150 cases, 50 eyes of 50 cases per trainee over one year such that on an average a trainee would get one case per week. Mean age of patients was 59.83 years +/- 7.56 years. Right eye was operated upon in 81 eyes while left eye was operated upon in 69 eyes. Males comprised 71 patients while females 79 patients.
Overall 56 cases were mature while 94 cases were immature (Grade I - 10, Grade II - 30, Grade III - 29, Grade IV - 13, Cortical - 10, Posterior subcapsular - 2). Posterior capsule rent occurred in 13 cases that was managed by anterior vitrectomy and intraocular lens (IOL) placement in the sulcus in ten eyes while scleral fixated in two cases. One case had an associated nucleus drop that underwent vitreoretinal surgery and nucleus removal on the same sitting. IOL was implanted at the sulcus in this patient.
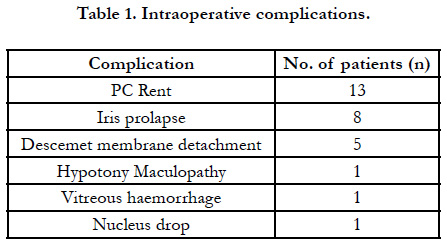
Descment membrane (DM) detachment was managed by injecting air bubble at the end of surgery and advising the patient to lie down in supine position. One case was found to have hypotony maculopathy secondary to wound leak on seventh postoperative day and underwent resuturing of the wound. One case was found to have vitreous haemorrhage on first post-operative day that resolved within two weeks by conservative management (Table 1).
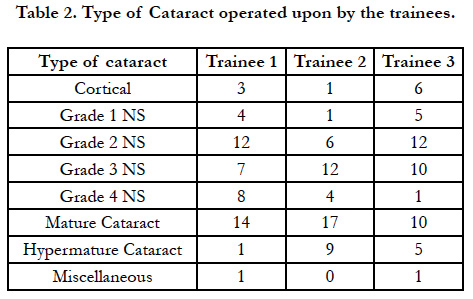
All attempts were made that all the three surgeons were given similar cases, though there were some minor discrepancies. Trainee 1 (A.K.S.) and trainee 3 (P.A.A.) operated upon more of immature cataracts while trainee 2 (R.R.A) operated more on mature cataracts (TABLE 2).
Overall visual acuity on the first postoperative day was found to be 20/100 overall that improved to 20/35 by the end of six weeks. A highly significant improvement in visual acuity was noted at the end of six weeks (p<0.001). All patients had IOL placed in their eye. A visual acuity of 20/200 or better was attained in 83% (n=125) patients and 46% patients (n=69) had a visual acuity of 20/60 or better on first postoperative day. Three patients had a visual acuity of hand movements while two patients had a visual acuity of only perception of light on the first post-operative day but all five improved to 20/140 or better at the end of six weeks. Most common post op cause for low vision was striate keratopathy that was treated by hypersol - 6 ointment (Sodium Chloride, Jawa Pharm, Pvt, Jaipur, India) given three times a day for two weeks or till corneal edema decreased.
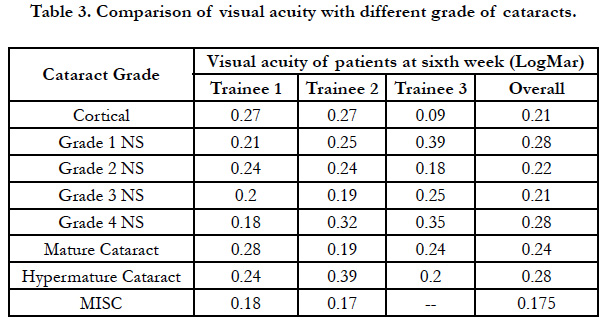
Even though all the trainees operated on different type of cataracts over one year (Table 3), it was found that the final visual acuity at the end of six weeks did not depend upon the type of cataract (p=0.988). Further the final post op visual acuity did not depend on the type of cataract (p=0.276).
All the three trainees were able to operate independently from the 25th case and all of them were able to operate at least ten of the last 15 cases given to them. No patient had severe complication like retinal detachment or endophthalmitis.
Discussion
In a previous retrospective study done by Aravind et al., [6] on a total of 79,777 patients, demographic factors pertaining to the patient was not found to be associated with intraoperative complications. Similar to them, our study also had more females. It might be due to the fact that the surgeries were being offered free and thus issue of costs and money wouldn’t arise [7].
MSICS needs to be mastered which requires sufficient experience. It is important to construct leak-proof valvular tunnel, have a competent capsulorhexis, nucleus prolapse and delivery. Phacoemulsification is a much costlier surgery. It has a prolonged and sometimes-traumatic learning curve [7]. Phacoemulsification has always found to have higher complication rates as compared to MSICS among trainees [6] and thus is a more practical approach for young surgeon training. The need for any supervisor to intervene decreased significantly, as time progressed and the trainees started to operate independently around the 25th case. They were able to complete the surgery in at least ten of the last 15 cases without any complications. On satisfactorily completing these ten cases, they were certified competent of handling cataract surgery. Lenticular opacity has been found to be statistically significant as per complications in other studies and maybe assumed due to bigger nuclei in denser cataracts that often pose challenges especially during prolapse but in our study the final visual acuity did not vary with the density of nucleus.
Though there is no minimum number of surgeries that may be taken as a sufficient learning curve, in our study it was found that 50 cases if done with a proper trainer were sufficient for a trainee. On the contrary, 80 cases were found to be sufficient for trainee phacoemulsification surgeons [8].
In a study [9] done in Nepal, it was found that about 20-30 assisted MSICS surgeries were required to master the surgery but a recent study done at Aravind eye hospital by Gupta et al., [11] recommended 300 surgeries for a resident to be competent to perform MSICS independently. We felt that 50 surgeries was a better quantity for the trainee to be conversant enough. A similar extensive study by Emmanuel et al., demonstrated that after 64 surgeries, the need of strict supervision diminished [7].
It is well known that transition to phacoemulsification is easier if one has mastered MSICS, as severeal steps such as scleral tunnel incision, capsulorhexis, hydro procedures, etcetera are common to both [10].
Being an observational study, several parameters could lead to a bias: The quality and extent of vision depends on the health of macula. Surgical training progress being assessed on Snellen’s visual outcome is also known to be fraudulent [7].
Conclusion
A good patient selection is another key factor in mastering MSICS. The ideal case is an immature cortical or grade II-III nuclear sclerosis. There should be no loss of zonular support, patients should have adequate intraoperative mydriasis. The cornea should be clear and have sufficient number of endothelial cells.
The trainee should be initially encouraged to concentrate on tunnel construction and geometry at initial stages.
Acknowledgements
Mr. Ankush Singhal, BBA, MBA for statistical analysis.
References
- Muralikrishnan R, Venkatesh R, Prajna NV, Frick KD. Economic cost of cataract surgery procedures in an established eye care centre in Southern India. Ophthalmic Epidemiol. 2004 Dec;11(5):369-80. PubMed PMID: 15590584.
- Albrecht H. Sutureless Non-phaco Cataract Surgery: A Solution to Reduce Worldwide Cataract Blindness?. Community Eye Health. 2003;16(48):49- 51. PubMed PMID: 17491831.
- Guzek JP, Ching A. Small-incision manual extracapsular cataract surgery in Ghana, West Africa. J Cataract Refract Surg. 2003 Jan;29(1):57-64. Pub- Med PMID: 12551668.
- Robin AL, Smith SD, Natchiar G, Ramakrishnan R, Srinivasan M, Raheem R et al. The initial complication rate of phacoemulsification in India. Invest Ophthalmol Vis Sci. 1997 Oct;38(11):2331-7. PubMed PMID: 9344356.
- Blumenthal M, Assia E. Extracapsular cataract extraction. In: Nordan LT, Maxwell WA, Davison JA, eds. The surgical rehabilitation of vision. New York: Gower Medical Publishing. 1992:10.1-10.
- Aravind H, David F, Mascarenhas R, Madhu S. Complication rates of phacoemulsification and manual small-incision cataract surgery at Aravind Eye Hospital. J Cataract Refract Surg. 2012 Aug;38(8):1360-9. doi: 10.1016/j. jcrs.2012.04.025. PubMed PMID: 22814042.
- Megbelayin EO, Rangarajan A, Pindikura S. Learning curve of a trainee ophthalmologist in manual small incision cataract surgery: A self-appraisal. J Surg. 2013;1:63-9.
- Randleman JB, Wolfe JD, Woodward M, Lynn MJ, Cherwek DH, Srivastava SK. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007 Sep;125(9):1215-9. PubMed PMID: 17846361.
- Hennig A. Nucleus management with Fishhook. Indian J Ophthalmol. 2009 Jan-Feb;57(1):35-7. PubMed PMID: 19075407.
- Ashok G. Clinical Significance and Relevance of Small Incision Cataract Surgery in the 21st Century Era. Master’ s Guide to Manual Small Incision cataract surgery (MSICS). India: Jaypee; 2009. p. 3-9.
- Gupta S, Haripriya A, Vardhan SA, Ravilla T, Ravindran RD. Residents’ Learning Curve for Manual Small-Incision Cataract Surgery at Aravind Eye Hospital, India. Ophthalmology. 2018 Nov;125(11):1692-1699. doi: 10.1016/j.ophtha.2018.04.033. PubMed PMID: 29861118.