Study of Ocular Manifestations in Patients Hospitalized with Dengue Fever
Shrivastava V1*, Sarkar S2
1 Consultant Vitreoretinal Surgeon, Vivekananda Institute of Medical Sciences, Sarat Bose Road Kolkata, India.
2 Senior Resident,Vivekananda Institute of Medical Sciences, Sarat Bose Road Kolkata, India.
*Corresponding Author
Vaibhav Shrivastava,
Consultant Vitreoretinal Surgeon,
Vivekananda Institute of Medical Sciences 99,
Sarat Bose Road Kolkata-700026, India.
E-mail: vaibhav.shrivastava.28@gmail.com
Received: August 26, 2018; Accepted: October 29, 2018; Published: October 31, 2018
Citation: Shrivastava V, Sarkar S. Study of Ocular Manifestations in Patients Hospitalized with Dengue Fever. Int J Ophthalmol Eye Res. 2018;6(6):387-392. doi: dx.doi.org/10.19070/2332-290X-1800078
Copyright: Shrivastava V© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To study the clinical spectrum of ocular manifestations in patients hospitalized with dengue fever during a dengue outbreak.
Design: It is a cross-sectional observational study, designed to determine the prevalence of ocular signs and symptoms, in hospitalized dengue patients. It was conducted from the month of September to November 2017 (3 months) in a tertiary care hospital of Kolkata, India during a recent dengue outbreak.
Methods: A detailed history was taken followed by a comprehensive eye examination which included BCVA assessment, Slit lamp based anterior segment examination was done followed by dilated fundoscopy with 90D slit lamp examination, the findings of which were confirmed by Indirect Ophthalmoscopy. Platelet counts and results of Dengue serological tests were also recorded.
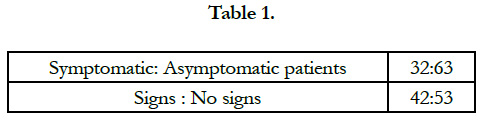
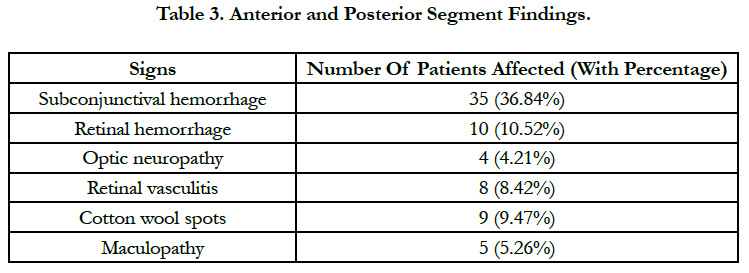
Result: 95 patients with dengue fever who were admitted in this hospital in the specified period were included in our study [1]. Dengue patients with ocular manifestations comprised 51.57%. Ocular pain was the most common symptom followed by redness and blurring of vision. The most common eye manifestation according to our study is Subconjunctival Haemorrhage (35.84%) followed by Retinal Hemorrhage (10.52%), Vascular Sheathing (10.52%), Cotton wool spots (9.47%),disc hyperamia (8.42%), and maculopathy (5.26%). Disc changes were noticed mainly in patients with previous history of dengue fever. Correlation of decrease in platelet count was significant with increase in subconjunctival hemorrhage, retinal hemorrhage, cotton wool spots and maculopathy (Pearsons’ correlation coefficient).
Conclusion: Patients hospitalized with dengue fever presented with a multitude of ocular symptoms and signs. The most common symptom being ocular pain whereas the most common sign being Subconjunctival hemorrhage. Intra retinal hemorrhages, maculopathy and cotton wool spots were the other most common signs all of which correlated with low platelet counts. Fundus examination can thus be used to prognosticate patients hospitalized with dengue fever.
2.Introduction
3.Materials and Method
3.1 Study Design And Study Population
3.2 Exclusion Criteria
3.3 Data Collection and Examination
4.Result
5.Discussion and Review of Literature
6.Conclusion
7.References
Keywords
Maculopathy, Dengue; Intra-Retinal Haemorrhage; Sheathing of Vessels; Cotton Wool Spots; Subconjunctival Hemorrhage; Ocular Coherence Tomography.
Introduction
Dengue fever, the most common mosquito borne viral disease in humans, is a multi-systemic disease with various complications [1-7]. It is transmitted through the bite of an infected female Aedes aegypti/albopictus mosquito [9]. The dengue virus belongs to the genus Flavivirus of the family Flaviviridae [1-4].
Dengue fever has increased gradually in the last two decades in India hence has become a major public health problem [25]. The incidence of dengue over the period 1998-2009 was 6.34 per million population which increased to 34.81 per million population in 2010-2014. (Data source: NVBDCP, Govt. of India).
Classic dengue fever is more commonly seen in adolescents and young adults [9]. It`s clinical features are classified into 5 presentations: non-specific febrile illness, classical dengue fever, dengue hemorrhagic fever, dengue hemorrhagic fever with shock syndrome and other unusual symptoms such as encephalopathy and hepatitis [10-13]. It is characterized by symptoms that appear 3-14 days after the bite of a vector [14] like sudden onset of fever associated with malaise, headache, joint pain, retro-orbital pain, maculopapular rash, associated thrombocytopenia, with or without bleeding manifestations etc. Ocular manifestations are otherwise uncommon. It has 4 serotypes (DEN-1, DEN-2 ,DEN-3, DEN-4) [8, 14]. The pathogenesis of systemic dengue infection is believed to be multifactorial, complex, and as yet not fully understood [15].
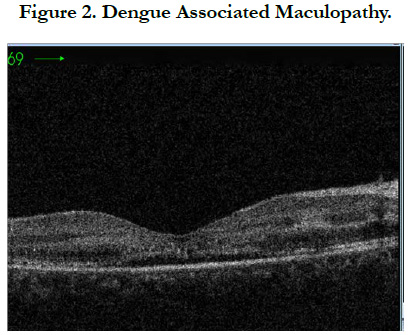
Ocular manifestations are rather uncommon but those reported in literature include subconjunctival, vitreous and retinal haemorrhage. Occasionally it may present with posterior uveitis, optic neuritis and maculopathies such as foveolitis and macular edema. Main symptoms include blurring of vision, scotoma, metamorphopsia and floaters [14]. Diagnostic and monitoring investigations include Optical coherence tomography, fundus fluorescein angiography and visual field analysis [14].
A cross-sectional observational study was conducted on all consecutive patients admitted with dengue fever, in a tertiary multispeciality hospital of Kolkata, India (Vivekananda Institute of Medical Sciences) over a period of three months during a dengue outbreak in 2017. The patients who were serologically positive, and also those diagnosed only on clinical grounds by the internists were considered as dengue fever and selected for our study. Eye screening examination was performed on these patients, irrespective of any ocular complaints. Informed consent was obtained from all patients who were included in the study. The study was approved by the Institutional Ethics Committee before commencement.
Patients with the following conditions were excluded:
1. Concurrent Febrile illness from malaria, or any other cause apart from dengue.
2. Patients with comorbidities like hypertension, diabetes or any other condition predisposing to retinopathy.
3. Patients in which informed consent could not be obtained.
A detailed history including some specific questions were asked. History of any similar previous episodes as well as any visual complaints persisting from previous similar episodes was taken. History of onset and duration of fever, associated complaints, past history of dengue fever, any ocular complaints during the onset of fever, of present or past illness, about presence of comorbidities, any history of trauma and coagulopathies were recorded. Laboratory reports of complete blood count including platelet count and serological assay of NS1, IgM, IgG were noted. Malaria was ruled out with MPDA (malarial parasite dual antigen) test.
All subjects then underwent the following tests - 1. Distance visual acuity (BCVA) using Snellen chart; 2. Near visual acuity (VA); 3. Pupillary light responses 4. Anterior segment examination using slit-lamp; 5. Dilated fundoscopy by 90D slit lamp examination and findings were corroborated with Indirect Ophthalmoscopy.
Patients with ocular symptoms and signs were followed-up subsequently. Patients with severe thrombocytopenia were examined at bedside only with an Indirect Ophthalmoscope.
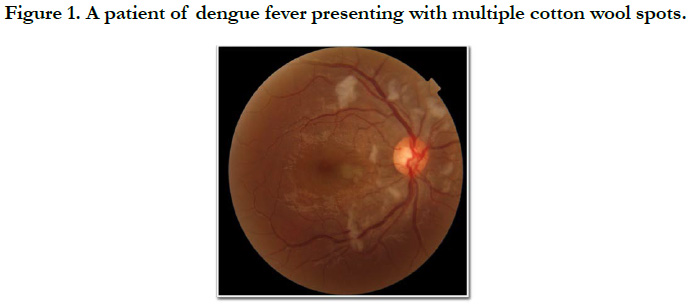
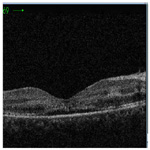
Fundus photos were documented in patients with retinal findings wherever possible. Subjects with macular changes consistent with dengue maculopathy underwent further examination, followed by investigations to confirm the diagnosis (Fundus photography, OCT). Diagnostic and monitoring investigations included direct and indirect ophthalmoscopy, optical coherence tomography, fundus photography and visual field analysis (Humphrey`s automated perimetry 24-2). A follow-up telephone call was made 2 weeks after the onset of fever to rule out any onset of new visual symptoms, and a repeat ophthalmic examination to rule out presence of dengue maculopathy.
A correlation study between platelet count and each of the individual ocular manifestations was done using Point biserial correlation method [17] which is mathematically equivalent to Pearson correlation coefficient [17]. p value of each coefficient was determined to prove whether the hypothesis was significant or not, and the level of significance's determined if it was significant. So, it was used to identify statistically significant relationships between the presence of ocular manifestations and platelet counts [18]. Statistical significance was assumed at P<0.05 level. All statistical analysis were done using STATA 14 software.
Result
This study was conducted over a 3 month period from September 2017 to November 2017, during a dengue outbreak. 110 consecutive patients were examined among which 95 patients were considered for inclusion in our study having a response rate of 86.36%. Others were not included as they matched one or more of the exclusion criteria. 110 patients suspected of dengue fever, were checked on the day of admission. 91 of them eventually had a positive dengue IgM, with the remaining 19 been negative. 4 IgM negative patients were presumed to have dengue fever by the treating physicians on clinical grounds with only NS1 positive, since an outbreak was prevailing and hence were included in our study. The mean interval between the onset of fever and the day of eye examination was 4 days. Table 2 summarizes the demographic profile of the patients. 55(57.89%) of them were male and 40(42.10%) were female.
Mean BCVA of the affected eyes were 6/7.5. Mean period of hospital stay was 5.9 (+-) 5.3 days. Minimum interval between the onset of fever and eye examination was 4 days. Mean interval between the onset of fever and the lowest platelet count was 5.7 days.
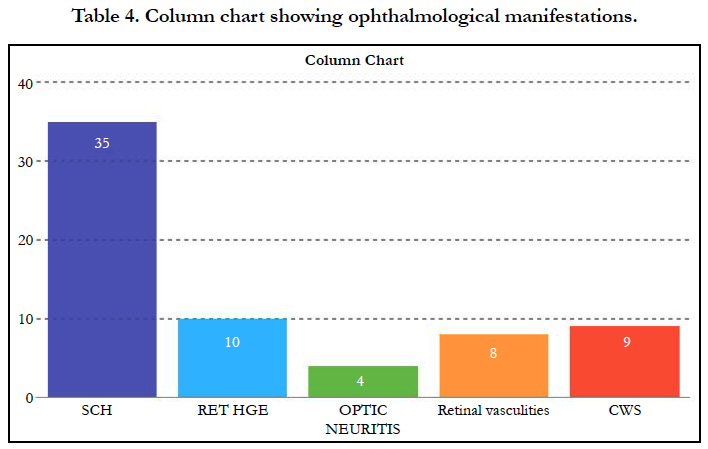
The most common eye manifestation according to our study is Subconjunctival Haemorrhage followed by Retinal Haemorrhage, Cotton wool spots, disc hyperemia and maculopathy. Disc changes were noticed mainly in patients with previous history of dengue fever.
49 (51.57%) patients were symptomatic while the rest were asymptomatic. The most common symptoms of the patients we studied included ocular pain, redness of eyes, and occasionally blurring of vision [14].
Eye examination was mainly performed on day 4 and day 6 of onset of fever. Diagnostic and monitoring investigations included optical coherence tomography, fundus photography and visual field analysis (Humphrey`s automated perimetry 24-2).
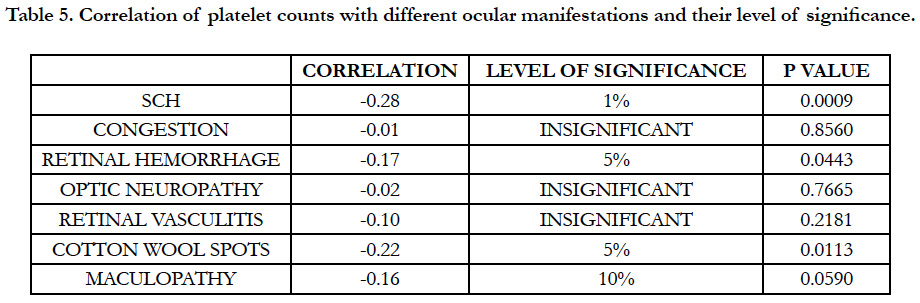
A correlation study between platelet count and each of the individual ocular manifestations were done using Point bi-serial correlation method. The results were as follows and are also depicted in Table 5:
Table 5. Correlation of platelet counts with different ocular manifestations and their level of significance.
• As the platelet count decreases, subconjunctival haemorrhage increases by 28.53% and the result is significant at 1% level of significance with p value 0.0009.
• As the platelet count decreases, congestion increases by 1.59% , but the result is insignificant with the p value 0.8560.
• As the platelet count decreases, retinal haemorrhage increases by 17.53% and the result is significant at 5% level of significance with p value 0.0443.
• As the platelet count decreases, Optic neuropathy increases by 2.61%, but the result is not significant with p value 0.7665.
• As the platelet count decreases, Retinal vasculitis increases by 10.79%, but the result is insignificant with p value 0.218.
• As the platelet count decreases, cotton wool spots increases by 22%, and the result is significant at 5% level of significance with p value 0.0113.
• As the platelet count decreases, maculopathy increases by 16% and the result is significant at 10% level of significance with p value 0.0590.
Correlation of decrease in platelet count was significant with increase in subconjunctival hemorrhage, retinal hemorrhage, cotton wool spots and maculopathy, with 28.53%, 17.53% , 22% and 16% respectively, at different levels of significance.
Discussion and Review of Literature
Dengue is an acute viral infection with potential fatal complications. Pathophysiologic mechanism of dengue fever is still not completely understood. Several theories have been suggested [16, 20-23]. While some studies support an immune mediated mechanism, others indicate towards an infective etiology [9, 28]. Predominant serotypes in India include DENV-1, DENV-2, DENV- 3 and DENV-4, though are antigenically related but are distinct , having several subtypes or genotypes [18]. The WHO 2009 classification divides dengue fever into two groups- uncomplicated and severe whereas the 1997 WHO classification divides dengue fever into 3 types - undifferentiated fever, dengue fever, and dengue haemorrhagic fever. WHO 1997 classification is still widely used.
Though dengue in India was first reported in Madras (now Chennai) in 1780, the first virologically proved epidemic dengue fever occurred in Calcutta (now Kolkata) in 1963 [18]. So, we can conclude dengue fever in Kolkata started way back. The predominant serotype affecting residents of Kolkata was DENV-3, dating back to 1983. It is also the oldest and most extinct lineage in India [18]. DENV 2 is the most common genotype in India almost over a span of 50 years [18]. Along with the usual manifestations, dengue presents atypically as well in many cases. It includes neurological, hepatic, musculoskeletal, cardiac, autoimmune, renal and cutaneous manifestations.
Dengue fever is known to affect a number of organ systems, but ocular manifestations are uncommon [19] and this may explain the paucity of published literature on the same. Moreover incidence and severity of dengue epidemics have increased only in the past two decades and so are the ocular manifestations which has led to renewed attention of the ophthalmologists on dengue patients. Whether increasing ocular involvement is also due to change in virus strain patterns is something which needs to be investigated. Chee et al., reported the possibility of dengue maculopathy to be serotype-specific [16]. No maculopathy was reported during a DEN-2 epidemic whereas there was a 10% incidence during a DEN-1 epidemic. The silver lining seems to be the fact that most of the ocular manifestations are self limiting and have a good prognosis though it is still unclear whether visual recovery is a part of the treatment or a part of the natural course of the disease.
Ocular manifestations reported in literature include subconjunctival hemorrhage, anterior uveitis, retinal hemorrhages, vascular sheathing, macular edema, periphlebitis, optic neuropathy, foveolitis, vitreous hemorrhage etc. Kanungo et al documented a case of Branch retinal artery occlusion secondary to dengue fever in 2008 [27].
Out of the 95 patients included in our study, 55 (57.9%) were males and 40( 42.1% ) were females. Subconjunctival hemorrhage was the most common ocular finding and the only anterior segment finding which correlated with low platelet count. Unlike previous studies we could not find any patient with signs of anterior uveitis [9, 27]. The second most common finding was retinal hemorrhages. It was also the most common posterior segment finding. Hemorrhage in patients with dengue fever can be due to multiple factors including thrombocytopenia, coagulation defects, capillary fragility and platelet dysfunction [29]. Cotton wool spots were another common posterior segment finding. The findings of our study were similar to that of Sujatha R et al., [27] albeit with minor differences. While a number of studies in India and globally have noticed Foveolitis as one of the characteristic finding, it was not seen in any of our patients [9, 30].
To our knowledge this is the first such study in eastern India which is a dengue endemic zone. This study should propel further prospective studies as there are many unanswered questions on ocular involvement in dengue patients.
The study has a number of limitations. First, the sample size was small. Second, we studied only hospitalized patients. Third, follow up after hospital discharge was not proper and we had to face a lot of dropouts. Serotype evaluation would have helped in getting some idea about the correlation of serotype with ocular involvement and this could not be done because of lack of infrastructure.
Conclusion
With increase in dengue cases and severity of the disease it is but natural for the number of patients with ocular involvement to increase further. It is imperative for the treating physician to know about this hitherto unknown fact of ocular involvement in dengue patients. All patients with visual/ocular symptoms should be referred to an ophhalmologist. Whether asymptotic patients will also benefit by eye examination is something which need to be studied further. Dengue eye manifestations are usually self-resolving, resulting mainly from an immune mediated reaction [1], with a few having long term effects. A detailed eye examination of both anterior and posterior segment has to be done in all dengue patients for early detection of ocular manifestations.
Association of ocular manifestation with decreasing platelet count has been noted. There is a need to organize educational programmes and health awareness trainings, for control of vector borne diseases. Early detections, through serology on the second day of the fever itself, during an epidemic is of utmost importance, in this way so that long term effects of any ophthalmological complications can be prevented. The diagnosis of dengue fever remains largely passive in India, more active community based epidemiological studies with intensive vector control and initiatives for dengue vaccine development should be geared up to control the spread of dengue in India [24].
A few limitations of this study includes small sample size, single hospital based study and only hospitalized patients were considered for inclusion. Many of the ocular manifestations are seen 7-10 days after the onset of dengue fever presumably because of immune mediated effects. These immune mediated manifestations could not be assessed as patients were discharged by that time.
Additional studies and randomized controlled trials needs to be conducted about the ocular manifestations of dengue fever and its long term consequences , which is yet an unexplored arena that lacks attention.
References
- Bacsal KE, Chee SP, Cheng CL, Flores JV. Dengue-associated maculopathy. Arch Ophthalmol. 2007 Apr;125(4):501-10. PubMed PMID: 17420370.
- Itha S, Kashyap R, Krishnani N, Saraswat VA, Choudhuri G, Aggarwal R. Profile of liver involvement in dengue virus infection. Natl Med J India. 2005 May-Jun;18(3):127-30. PubMed PMID: 16130612.
- Subramanian V, Shenoy S, Joseph AJ. Dengue hemorrhagic fever and fulminant hepatic failure. Dig Dis Sci. 2005 Jun;50(6):1146-7. PubMed PMID: 15986872.
- Kularatne SA, Gawarammana IB, Kumarasiri PR. Epidemiology, clinical features, laboratory investigations and early diagnosis of dengue fever in adults: a descriptive study in Sri Lanka. Southeast Asian J Trop Med Public Health. 2005 May;36(3):686-92. PubMed PMID: 16124439.
- Wiwanitkit V. Dengue myocarditis, rare but not fatal manifestation. Int J Cardiol. 2006 Sep 10;112(1):122. PubMed PMID: 16307808.
- Kalita J, Misra UK, Mahadevan A, Shankar SK. Acute pure motor quadriplegia: is it dengue myositis?. Electromyogr Clin Neurophysiol. 2005 Sep- Oct;45(6):357-61. PubMed PMID: 16315973.
- Rao IS, Loya AC, Ratnakar KS, Srinivasan VR. Lymph node infarction--a rare complication associated with disseminated intra vascular coagulation in a case of dengue fever. BMC Clin Pathol. 2005 Dec 12;5:11. PubMed PMID: 16336698.
- Bronnert J, Malhotra C, Suavansri K, Hanvesakul R, Kulwichit W, Wilde H. Complete ptosis caused by dengue fever. Lancet. 2005 Dec 3;366(9501):1982. PubMed PMID: 16325703.
- Lim WK, Mathur R, Koh A, Yeoh R, Chee SP. Ocular manifestations of dengue fever. Ophthalmology. 2004 Nov;111(11):2057-64. PubMed PMID: 15522372.
- Nimmannitya S. Clinical spectrum and management of dengue haemorrhagic fever. Southeast Asian J Trop Med Public Health. 1987 Sep;18(3):392-7. PubMed PMID: 3433169.
- Nimmannitya S, Thisyakorn U, Hemsrichart V. Dengue haemorrhagic fever with unusual manifestations. Southeast Asian J Trop Med Public Health. 1987 Sep;18(3):398-406. PubMed PMID: 3433170.
- Kalayanarooj S, Vaughn DW, Nimmannitya S, Green S, Suntayakorn S, Kunentrasai N, et al. Early clinical and laboratory indicators of acute dengue illness. J Infect Dis. 1997 Aug;176(2):313-21. PubMed PMID: 9237695.
- World Health Organization. Dengue Haemorrhagic Fever: Diagnosis, treatment, prevention and control. 2nd ed. Publication no. 1152249. Geneva: World Health Organization; 1997.
- Ng AW, Teoh SC. Dengue eye disease. Surv Ophthalmol. 2015 Mar-Apr;60(2):106-14. doi: 10.1016/j.survophthal.2014.07.003. PubMed PMID: 25223497.
- Yacoub S, Mongkolsapaya J, Screaton G. The pathogenesis of dengue. Curr Opin Infect Dis. 2013 Jun;26(3):284-9. doi: 10.1097/QCO.0b013e32835fb938. PubMed PMID: 23449140.
- Su DH, Bacsal K, Chee SP, Flores JV, Lim WK, Cheng BC, et al. Prevalence of dengue maculopathy in patients hospitalized for dengue fever. Ophthalmology. 2007 Sep;114(9):1743-7. PubMed PMID: 17561258.
- Demirtas H, Hedeker D. Computing the point-biserial correlation under any underlying continuous distribution. Communications in Statistics-Simulation and Computation. 2016 Sep 13;45(8):2744-51.
- Gupta N, Srivastava S, Jain A, Chaturvedi U. Dengue in India. Indian J Med Res. 2012 Sep;136(3):373-90. PubMed PMID: 23041731.
- Rigau-Pérez JG, Clark GG, Gubler DJ, Reiter P, Sanders EJ, Vorndam AV. Dengue and dengue haemorrhagic fever. Lancet. 1998 Sep 19;352(9132):971-7. PubMed PMID: 9752834.
- Markoff LJ, Innis BL, Houghten R, Henchal LS. Development of crossreactive antibodies to plasminogen during the immune response to dengue virus infection. J Infect Dis. 1991 Aug;164(2):294-301. PubMed PMID: 1856477.
- Rico-Hesse R, Harrison LM, Salas RA, Tovar D, Nisalak A, Ramos C, et al. Origins of dengue type 2 viruses associated with increased pathogenicity in the Americas. Virology. 1997 Apr 14;230(2):244-51. PubMed PMID: 9143280.
- Rothman AL, Ennis FA. Immunopathogenesis of dengue hemorrhagic fever. Virology. 1999 Apr 25;257(1):1-6. PubMed PMID: 10208914.
- Lei HY, Yeh TM, Liu HS, Lin YS, Chen SH, Liu CC. Immunopathogenesis of dengue virus infection. J Biomed Sci. 2001 Sep;8(5):377-88. PubMed PMID: 11549879.
- Halstead SB. Pathogenesis of dengue: challenges to molecular biology. Science. 1988 Jan 29;239(4839):476-81. PubMed PMID: 3277268.
- World Health Organization. Dengue: Guidelines for Diagnosis. Treatment, Prevention and Control: New Edition. World Health Organization: Geneva. 2009. PubMed PMID: 23762963.
- Kanungo S, Shukla D, Kim R. Branch retinal artery occlusion secondary to dengue fever. Indian J Ophthalmol. 2008 Jan-Feb;56(1):73-4. PubMed PMID: 18158412.
- Sujatha R, Nousheen S, Nazlin A, Prakash S. Ocular manifestations of dengue fever. Int J Med Sci Pub Health. 2015;4:690-693.
- Chan DP, Teoh SC, Tan CS, Nah GK, Rajagopalan R, Prabhakaragupta MK, et al. Ophthalmic complications of dengue. Emerg Infect Dis. 2006 Feb;12(2):285-9. PubMed PMID: 16494756.
- Chhina DK, Goyal O, Goyal P, Kumar R, Puri S, Chhina RS. Haemorrhagic manifestations of dengue fever & their management in a tertiary care hospital in north India. Indian J Med Res. 2009 Jun;129(6):718-20. PubMed PMID: 19692757.
- Kamath SJ, Nayak MK, Gour R, Singh N. Dengue Stings the Eye!. J Clin Diagn Res. 2017 Sep;11(9):ND03-ND05. doi: 10.7860/JCDR/2017/25563.10610. PubMed PMID: 29207746.
- Mutheneni SR, Morse AP, Caminade C, Upadhyayula SM. Dengue burden in India: recent trends and importance of climatic parameters. Emerg Microbes Infect. 2017 Aug 9;6(8):e70. doi: 10.1038/emi.2017.57. PubMed PMID: 28790459.