Posterior Cerebral Artery Infarct with Haemorrhagic Transformation
Cham KM1*, Wang J2
1 Department of Optometry and Vision Sciences, The University of Melbourne, Victoria 3010, Australia.
2 OPSM West Lakes, South Australia 5021, Australia.
*Corresponding Author
Kwang Meng Cham,
Department of Optometry and Vision Sciences,
The University of Melbourne, Victoria 3010, Australia.
E-mail: ckwang@unimelb.edu.au
Received:November 17, 2017; Accepted: November 27, 2017; Published: November 29, 2017
Citation: Cham KM, Wang J. Posterior Cerebral Artery Infarct with Haemorrhagic Transformation. Int J Ophthalmol Eye Res. 2017;5(9):348-350. doi: dx.doi.org/10.19070/2332-290X-1700070
Copyright: Kwang Meng Cham© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
A 65-year-old female presented with visual disturbances a week following surgical breast biopsy and stopping eliquis. A diagnosis of a perioperative posterior cerebral ischemic stroke with haemorrhagic transformation, in the setting of eliquis cessation, was made. Despite several features in this case suggesting a posterior cerebral artery cardio embolic ischemic stroke, differentials such as infarctions of the anterior circulation and middle cerebral artery, other possible causes of posterior circulation stroke, acute peripheral vestibular dysfunction, intracranial or subarachnoid haemorrhage, neoplasms, basilar migraine, toxic or metabolic disturbances, neuro-inflammatory or chronic infectious conditions, and ocular vascular disorders should be considered.
Prompt detection and diagnosis of cardio embolic cerebral infarction is crucial to initiate long-term anti-coagulant therapy for secondary prevention. Clinicians should maintain a high index of suspicion for the signs and symptoms of stroke. Apart from a detailed history, a complete neurological examination with appropriate imaging will aid clinicians in detection, diagnosis and prevention of stroke with appropriate referral and management.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Ischemic Stroke; Cerebrovascular Disease; Atrial Fibrillation; Posterior Cerebral Artery
Introduction
Stroke is the primary cause of disability, and the second most common cause of global mortality [1, 3]. Cardio embolic cerebral infarction accounts roughly 25% of all infarcts, and is regarded as the most severe ischaemic stroke subtype with high hospitalisation fatality rate (6%-27%) [2, 4]. The frequency varies between 14% to 30.6%, with incidence reaching as high as 36% when 85 years or older [5].
Case Report
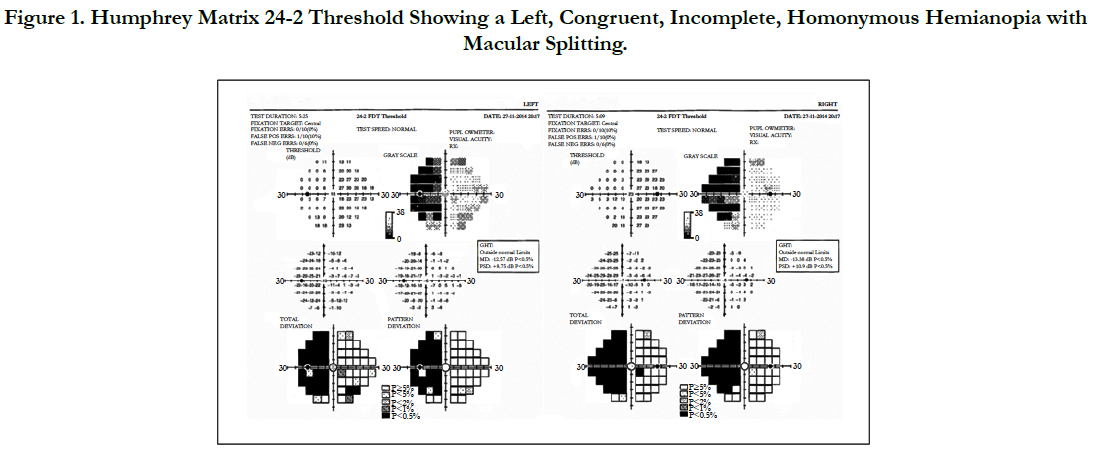
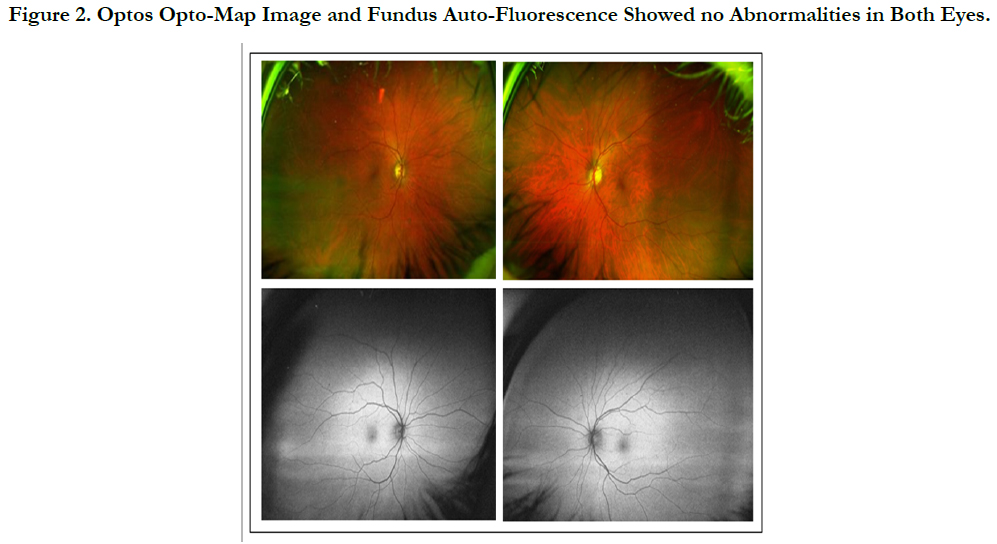
A 65-year-old female presented with ‘violent’ headaches and visual disturbance in her left side, a week following surgical breast biopsy and stopping eliquis 48 hours prior, which she was prescribed for atrial fibrillation. Best-corrected visual acuities were 6/6 binocularly. Excursions were smooth with no diplopia or nystagmus. Pupillary reactions were normal. Confrontation revealed possible left hemianopia, and visual field testing with Humphrey Matrix 24-2 threshold showed a left, congruent, incomplete, homonymoushemianopia with macular splitting (Figure 1). She denied any previous cerebral vascular events and her family history was unremarkable. Further questioning showed no history of amaurosis fugax, transient ischemic attacks or syncope. There were no other focal neurological symptoms, motor weakness or sensory deficits. Anterior segment biomicroscopy and a dilated fundus examination were normal (Figure 2). No signs of arterial/arteriolar plaques, cotton wool spots, vascular occlusions, and venous stasis retinopathy were detected.
Figure 1. Humphrey Matrix 24-2 Threshold Showing a Left, Congruent, Incomplete, Homonymous Hemianopia with Macular Splitting.
The patient was referred to a neuro-ophthalmologist the same day, and the clinical findings were confirmed. A neurological examination returned normal cranial nerves, gait and speech. Her upper and lower limbs showed no weaknesses or paralysis, and there were no ataxia or sensory deficits. Her blood pressure was 114/66 mmHg, with a pulse of 60 beats per minute. A computed tomography (CT) brain and an angiogram scan revealed a hypo-dense region in the right posterior cerebral artery (PCA) territory with some haemorrhage and surrounding oedema. No signs of arterial stenosis or occlusion were observed. The presence of her cardiac pacemaker precluded use of magnetic resonance imaging. Results for the patient’s breast biopsy were normal, and there was no evidence of intracranial tumours.
Based on the above findings, a diagnosis of a perioperative right PCA territory cardio embolic ischemic stroke with haemorrhagic transformation, in the setting of eliquis cessation, was made. The patient was advised to discontinue driving, and a repeat CT brain scan was scheduled in a month’s time.
Discussion
Cardio embolism may arise from: (i) blood stasis and thrombus formation in an enlarged or structural change in the heart chamber; (ii) material discharged from an anomalous valvular surface, and (iii) abnormal venous-to-arterial circulatory system [2]. Several features in this case strongly suggest a PCA cardio embolic ischemic stroke. These include: (i) atrial fibrillation, the most common and important cause of cardiac disease with risk for embolism [4]. Atrial fibrillation causes stroke by blood stasis in the atrial appendage, elevating fibrinogen levels, D-dimer, and von Willebrand factor. This pro-thrombotic state is then liable to thrombus formation with subsequent increased rate of cerebral embolization [3]; (ii) eliquis cessation, an anti-coagulant that prevents stroke and embolism in atrial fibrillation; (iii) haemorrhagic transformation, which occur up to 71% of cardioembolic strokes, and as many as 95% of haemorrhagic infarcts are caused by cardio embolism [4]; (iv) severe headaches, likely due to irritation of trigeminal vascular afferents located in brainstem arteries [6], and are vascular in origin [7], and (v) acute homonymous hemianopia, which suggests PCA due to ischemia [8]. Despite these strong associations, differentials such as infarctions of the anterior circulation and middle cerebral artery, other possible causes of posterior circulation stroke (e.g. vertebro-basilar dolichoectasia, cervical arterial dissection, subclavian steal syndrome), acute peripheral vestibular dysfunction, intracranial or subarachnoid haemorrhage, neoplasms, basilar migraine, toxic or metabolic disturbances, neuro-inflammatory or chronic infectious conditions (e.g. sarcoidosis, Behcet’s disease), and ocular vascular disorders (ischemic optic neuropathy and central retinal vein occlusion) should be considered [9].
Prompt detection and diagnosis of cardio embolic cerebral in-farction is crucial to initiate long-term anti-coagulant therapy for secondary prevention [10]. Currently there is no consensus in establishing the diagnosis and optimal treatment modality. Alcohol abuse, hypertension with valvular heart disease and atrial fibrillation, nausea and vomiting, and previous cerebral infarct may predict stroke recurrence [4]. The National Institutes of Health Stroke Scale (NIHSS) is of limited value in posterior circulation stroke, with patients having a poor prognosis despite low NIHSS scores [11].
Conclusion
Clinicians should maintain a high index of suspicion for the signs and symptoms of stroke. Apart from a detailed history, a complete neurological examination with appropriate imaging will aid clinicians in detection, diagnosis and prevention of stroke with appropriate referral and management. Based on the CHADS2 index (acronym for Congestive heart failure, Hypertension, Age, Diabetes and Stroke), the patient scored 3/6 and will have a high annual risk of stroke [12]. The patient will require life-long ongoing monitoring and review to detect stroke recurrence and rehabilitation.
References
- Arboix A, Alió J. Cardio embolic stroke: clinical features, specific cardiac disorders and prognosis. Current Cardiol Rev. 2010 Aug;6(3):150-161. DOI:10.2174/157340310791658730. PubMed PMID: 21804774.
- Ferro JM. Brain embolism. Answers to practical questions. J Neurol. 2003 Feb;250(2):139-147. DOI:10.1007/s00415-003-1017-0. PubMed PMID: 12574943.
- Weir NU. An update on cardio embolic stroke. Postgrad Med J. 2008 Mar;84(989):133-142. DOI:10.1136/pgmj.2007.066563. PubMed PMID: 18372484.
- Arboix A, Alió J. Acute Cardio embolic Cerebral Infarction: Answers to Clinical Questions. Current Cardiol Rev. 2012 Feb;8(1):54-67. DOI:10.2174/157340312801215791. PubMed PMID: 22845816.
- Arboix A, Vericat MC, Pujades R, Massons J, Garcia-Eroles L, Oliveres M. Cardioembolic infarction in the Sagrat Cor-Alianza Hospital of Barcelona Stroke Registry. Acta Neurol Scand. 1997 Dec;96(6):407-412. DOI:10.1111/j.1600-0404.1997.tb00307.x. PubMed PMID: 9449481.
- Vestergaard K, Andersen G, Nielsen MI, Jensen TS. Headache in stroke. Stroke. 1993 Nov 1;124:1621-1624. DOI:https://doi.org/10.1161/01. STR.24.11.1621.
- Fisher CM. The posterior cerebral artery syndrome. Can J Neurol Sci. 1986 Aug;13(3):232-239. DOI: https://doi.org/10.1017/S0317167100036337 PubMed PMID: 3742339.
- Margolis MT, Newton TH, Hoyt WF. Cortical branches of the posterior cerebral artery: Anatomic-radiologic correlation. Neuroradiology. 1971 Aug;2(3):127-135.DOI:https://doi-org/10.1007/BF00335041. PubMed PMID: 5164214.
- Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. 2014;5:30. DOI:10.3389/fneur.2014.00030. PubMed Central PMCID: 3985033.
- Bogousslavsky J, Regli F, Maeder P, Meuli R, Nader J. The etiology of posterior circulation infarcts: a prospective study using magnetic resonance imaging and magnetic resonance angiography. Neurology. 1993 Aug;43(8):1528-1533. DOI:http://dx.doi.org/10.1212/WNL.43.8.1528. PubMed PMID: 8351006.
- Sato S, Toyoda K, Uehara T, Toratani N, Yokota C, Moriwaki H, et al. Baseline NIH Stroke Scale Score predicting outcome in anterior and posterior circulation strokes. Neurology. 2008 Jun 10;70(24 Pt 2): 2371-2377. DOI:10.1212/01.wnl.0000304346.14354.0b. PubMed PMID: 18434640.
- Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke. Results from the national registry of atrial fibrillation. JAMA. 2001;285(22):2864-2870. DOI: 10.1001/jama.285.22.2864.