The Occurrence and Pattern of Uterine Cervix Lesions in the Tropics: The Igbo Women of Eastern Nigeria Experience
Ndubuka GIN1*, Ngwogu KO2, Ejeta KO1, Okafor CW1, Ajugo E1, Nwosu IO3, Nwosu IL3
1 Departments of Biomedical Technology and Anatomy, Federal University of Technology, Owerri, Nigeria.
2 Department of Histo Pathology, College of Medicine and Health Sciences, Abia State University Teaching Hospital Aba, Nigeria.
3 Ivory Specialist Hospital LTD, Aba, Nigeria.
*Corresponding Author
Ndubuka GIN,
Department of Biomedical Technology,
Federal University of Technology, Owerri, Nigeria.
Tel: +2348056604122
Email: chiomaimmenmachi@gmail.com/chinmagideon@yahoo.com
Received: January 14, 2019; Accepted: April 08, 2019; Published: April 09, 2019
Citation: Ndubuka GIN, Ngwogu KO, Ejeta KO, Okafor CW, Ajugo E, Nwosu IO, et al.,. The Occurrence and Pattern of Uterine Cervix Lesions in the Tropics: The Igbo Women of Eastern Nigeria Experience. Int J Forensic Sci Pathol. 2019;6(1):400-406. doi: dx.doi.org/10.19070/2332-287X-1900084
Copyright: Ndubuka GIN© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The process of disease development in the cervix follows stimulus from oncogenic factor acting principally on the anterior and posterior cervical lips site during cervical eversion resulting to metaplasia in one hand, or on the histophysiology and immunity to give disease. The lesions of the cervix vary in number, type, and rare with few children forms in existence. From 18 years retrospective study were and 1501 specimens of uterine cervix from Igbo female patients of South-Eastern Nigeria whose ages ranged from 20 to 79 years, consulted at 5 major Hospitals and Pathology Laboratories. Common clinical symptoms were irregular vaginal bleeding, lower abdominal pain, post coital bleeding, and weakness in the morning. Nine diseases found were inflammation, benign, and three sub-types of carcinoma. Benign lesions were 28% in 5 age groups and 75% is inflammatory, and 40 - 49 was most burdened with 52% cases while 19% are in 20 - 29. Sixty six percent cancers occurred in 5 age groups to which 34% is in 50 - 59 and is followed by 30% in 60 - 69. All cervical diseases distribution showed 35% were in 40 - 49 and 27% with 50 - 59 while 7% occurred in 20 - 29. Squamous cell carcinoma is 38% of all cervical diseases and was found most 57% of 989 cancer cases. Cancers nuclear features were specific and undifferentiated showed 78% of oval nuclear over all shapes, and 60% were seen of poorly differentiated. All diseases were histomorphologically distinguishable in pattern of cells arrangement and haematologic parameters less significance.
2.Abbreviations
3.Introduction
4.Materials and Methods
5.Results
6.Discussion
7.Conclusion
8.References
Keywords
Cervical Diseases; Distribution Burden; Age Group; Clinical Features; Region.
Keywords
CIN: Cervical Intraepithelial Neoplasia; SIL: Squamous Intraepithelial Lesion; HPV: Human Papillomavirus.
Introduction
The diseases of the uterine cervix varied in presentations and two major types have been confirmed to be benign - i.e. soft tissue neoplasias, which long have been said to contain sufficient cellular pointer to stromal sarcoma advancement. The other is papillomavirus-related cervical intraepithelial neoplasias which is precancerous lesions [1] and may not always advance to cancer as they spontaneously can regress when stimulus is removed. The duo development is associated in part to lots of factors which when incident on squamocolumnar junction can engender histologic changes [2]. The periodic changes of transformation of the cells of the anterior or posterior cervical lips particularly at menopause [3] or before cellular metaplasia of the region predisposes the susceptible site to evolution of several cancer lesions [4] which may occur more often than when there is short period benign lesion giving rise to same cancer.
The development of benign neoplasias of the uterine cervix is dependent upon factors or as natural differentiation occurs in association. When such potentiating factors are incidental, the frequency is not generally for the two basic types. Most common type is leiomyoma of the cervix which is said to account for 8% of all uterine leiomyoma [5]. These lesions may protrude as polyp into the endocervical canal at which position it is commonly considered as endocervical polyp. Being submucosal, leiomyoma of the uterine corpus origin appear with histologic resemblance with the other lesions but may have the potential of malignant simulation or transformation. However endocervical polyps are always viewed by Investigators as common lesion among 4th to 6th decade of multigravidas [6, 7]. Associated symptoms are profuse mucous discharge or abnormal bleeding said to be often with small size of 1cm in diameter as well as large polyps [8]. Also much friction or irritations by large protruding polyps of 5cm and above seem to produce increased and variable infrequent clinical symptoms. Though these same clinical symptoms are observable of vaginal polyps but do vary slightly in histomorphologic entities with the presence of atypical stromal cells [9]. Clinical symptoms of uterine leiomyomas are associated abnormal bleeding, sudden pain, post-coital bleeding, frequent or uncurbed microorganism infections and anaemia.
The others rare but possible benign neoplasia of the cervix include lipoma, blue nevus, glioma, and lymphangioma [10-14], and these are accidental finding in hysterectomy. Possible among the younger females are two rare neoplasia types of mesonephric papilloma and papilloma adenofibroma [15, 16].
Several factors have been confirmed to promote or cause cervical lesions which are associated with the development of sustained or frequent stimulus over time. These may be direct or indirect factors as contended by similar studies. Multiple sex partners and the age of first sexual intercourse have been said to predispose an individual female to increasing risk of an oncogenic factor to cervical intraepithelial neoplasia (CIN) or other intraepithelial abnormal changes (dysplasia) over the period. The potential effects of poor hygiene resulting to viral and bacterial infections [17-20] have been identified as etiologic factors to cervical cancer (particularly the presence of Haemophilus vaginalis, Chlamydia, Neisseria gonorrhoeae and Trichomonas protozoa that can on colonizing the region initiate cervicitis of varying degree or lesion). The presence of viral content in Papanicolaou smears from young women with cervical warts have been established to progress to neoplasia (CIN) and squamous intraepithelial lesion (SIL) and hence cancer. Viral particles identified include those of Herpesvirus, Human papilloma virus (HPV), and Cytomegalovirus which are all known as potentiators of cervical cancer through CIN or SIL. Other factors regarded as indirect are age of patients (which is obvious at sudden withdrawal of hormonal volume or eventual absence), pregnancy (when there is up surge of certain hormones) and trauma (continued irritation or friction, which may be post operative or accidental).
The identification, characterization or staging of cervical lesions are based on good and reliable histological methods that can showcase histomorphologic entities of the lesion and the possible isolates and/or confirmation of the presence of causative agents. These methods have earlier been standardized through Papanicolaou smear screening method, and of late the identification of DNA of HPV, [21, 22] Herpes virus, Chlamydia trachomatis and others in smears and tissues. Also the screenings of patient hormonal status, age and socioeconomic status have been helpful though not specific.
The analysis and recognition of the presence of precancerous conditions is key to prevention and staging of cancers, while the evidence of benign lesions are only subjective and hence is to tackle early stage or factors potential enough for cancer development as the large leiomyomatous polyps, and Condyloma [23]. These lesions are also capable of regression.
The 18 year study of lesions affecting the uterine cervix of Igbo women of Nigeria was to ascertain if there are new changes apart from previous existing pattern through which cervical lesions can occur in the early 21st century. In addition, identifiable and possible evidence of new factors capable of transforming epithelial cells to cancer through new characteristic pattern of benign lesions or histomorphologic changes specific for any new factor will be searched. The search would reveal uterine cervical lesions, and epidemiological data about the Igbo women of Eastern Nigeria.
Materials and Methods
The retrospective study spanned through a period of 18 years (1996-2013), involving scrutiny of 2581 patients whose clinical folders, laboratory request forms and results were traced to Igbo female residence in South-East Nigeria. Their samples to Royal Ihedu Medical Diagnostic Laboratory were further traced to Hospitals (Government, Private and Mission) which though may or not have required facilities and efficient Staff for Histopathology diagnosis but have the capability for Surgical procedures. Such Hospitals were located at South-east of Igbo land which population is majorly characterized by peasant farmers, artisans, professionals, numerous traders and civil servants (Figure 1). Names of such patients and dates of surgery were confirmed by comprehensive scrutiny of staffers and possibly trace patient to home address only on uterine cervix cases. Cases which confirmation and ethnic origin were not determined or found to hale by birth of cross-ethnic marriage mother or father were disqualified for the study. Also cases which folders bear understandable clinical history and which were further found difficult to comprehend were further subjected to scrutiny, and on failure were rejected for the study.
All clinical records and histopathology report books consulted and approved were reviewed alongside processed tissue blocks and slides and must have convincing identity to one of the five Pathology Laboratories of the Hospitals chosen for the study. The remaining gross or fragments samples from which tissue blocks and slides were made ab initio, were searched to ascertain and authenticate the origin of tissue blocks and slides. Tissue blocks and their slides were sought and reviewed microscopically alongside all corresponding histopathology reports. Also clinical history of patients assessed were used to considered accuracy of request for laboratory testing of samples and results, while medical imaging involvement in sampling and diagnosis was considered for appropriateness of sample and authentication of site. Ultrasound imaging, Colposcopy and ablation and/or excisions were considered and involved procedures.
All clinical records irrespective of sufficient patient history were further probed for satisfactory evidence and must meet the criteria for inclusion if tissue blocks and slides were traced to them. New slides were also made from these blocks, stained by popular Harris's heamatoxylin and eosin staining technique. The same were reported upon and diagnosis authenticated in comparison with previously histopathology reports. Nuclear shapes were evaluated on random scale of 100 cell nuclei per light-field microscopy for up to 1000 cell nuclei. Therefore number of light-field microscopy viewed is directly proportional to cell nuclei counted. Also the heamatological parameters of patients were sought through the folders and same reports were traced to Departments of Heamatology for authentication accuracy, and confirmation.
Results
In 18 years consultation were 1501 uterine cervix samples searched out of 2581 gynecological specimens from five hospitals located in five states in the South-East Nigeria in 5 States in the region. In all only 1381 (92%) cases sampling were by excision or ablation after Colposcopy as means of treatment as well. These follow abdominoperineal ultrasound imaging which help for appropriateness and investigation of site, and in 120 cases there were no ultrasound but only colposcopy carried out after which was ablation or excision. Such technical procedures were carried out in all of the five hospitals in Aba, Abakaliki, Enugu, Owerri, and Umuahia towns in the States of the region (Figure 1) for sample collection. It was observed that not all the Hospitals have the capability for histopatholgy investigations and refer samples to Royal Ihendu Medical Diagnostic Laboratory and these were inclusive in this study.
Figure 1. Geo-Political zone in Nigeria expressed in the Nation’s Map, and Igbo land is (SE) coloured purple. Courtesy of aboutnigerians.com 2018.
From the clinical folders discovered that common clinical symptoms of uterine cervix lesions were infrequent with lesion type and may remain variable as lesion progresses or even constant. Must common are associated often and on weakness to do house chores, fainting in morning that progresses to loss of balance while walking in the day, pelvic pain, abnormal bleeding and sudden pain even at coitus, post-coital bleeding, frequent or uncurbed micro organism infections and paleness of eyelids and sub-mucosa observed pronounced at late lesion.
All the new slides made from selected tissue blocks reviewed had same diagnosis as the previous, hence there was no variation of results observed. Also provisional diagnosis was accurate in 96.4% of all uterinal cervix samples though clinical signs and syptoms were the same for all.
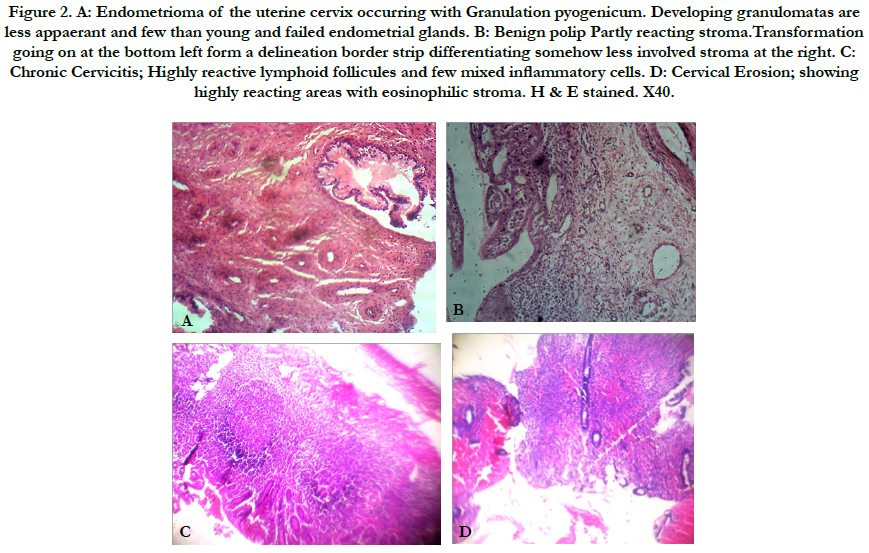
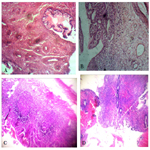
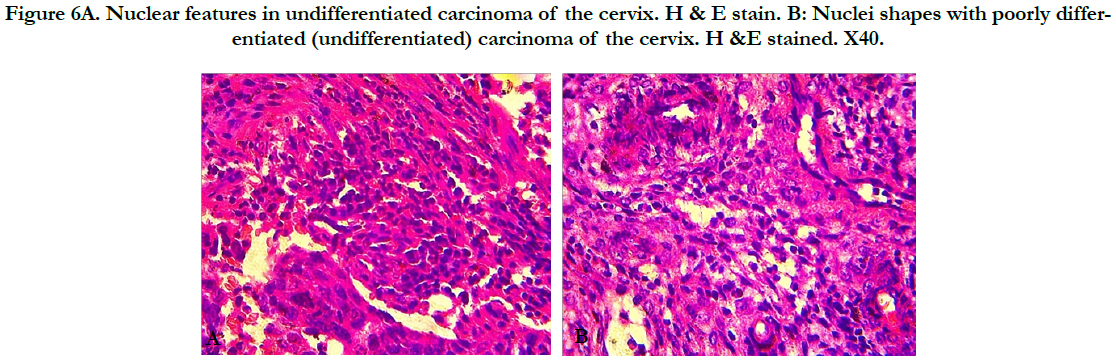
Three basic diseases were found in the cervix were inflammation, benign neoplasia, and cancer occurring in their subtypes and at varying degrees. Histomorphologic entities present denote specific type and pattern of arrangement with all appeared characteristically revealling transformation components that did not expose causative factors (Figures 2-6). Nuclear features were specific for individual cancer type in shapes and sizes while pattern of arrangement confirms design (which also was not specific for same type) that warranted rondom differentiation from slides of the three cancer types. Two nuclear shapes was observed frequent and occurred more than others in all the slides classed as differentiated and undifferentiated (Figures 4-6). Apparent was that 221 of 283 undifferentiated show oval shaped nuclear dominancy over spindle while with differentiated, 60% of poorly differentiated show oval shaped nuclear dominancy.
Figure 2. A: Endometrioma of the uterine cervix occurring with Granulation pyogenicum. Developing granulomatas are less appaerant and few than young and failed endometrial glands. B: Benign polip Partly reacting stroma.Transformation going on at the bottom left form a delineation border strip differentiating somehow less involved stroma at the right. C: Chronic Cervicitis; Highly reactive lymphoid follicules and few mixed inflammatory cells. D: Cervical Erosion; showing highly reacting areas with eosinophilic stroma. H & E stained. X40.
Figure 3A. Leiomyomatous polyp. Aggressive reacting and suspicious disarrayed papillary component and varied glandular elements patterned in loosed scanty stroma. B: Cervical Dysplasia (CIN III); the dysplastic changes varied based on the degree of infection (Cervicitis). H & E stained. X40.
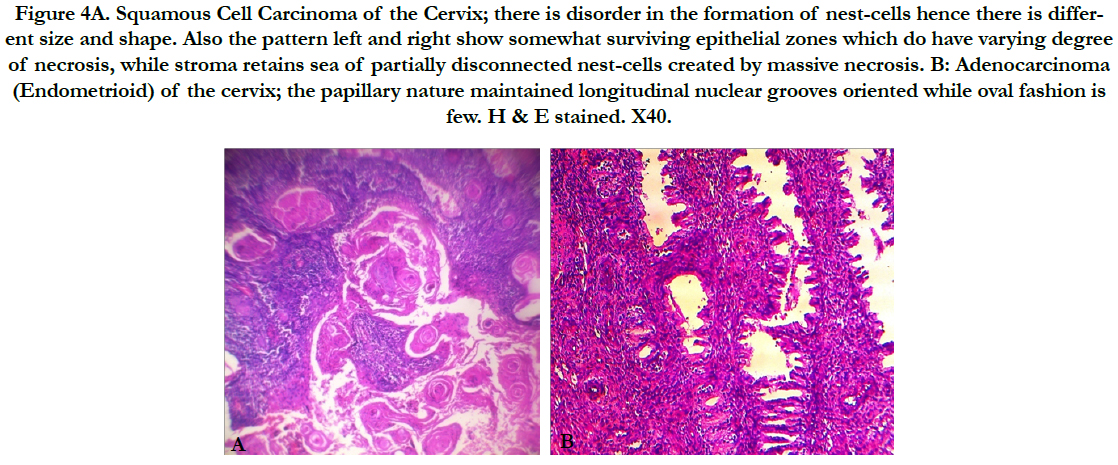
Figure 4A. Squamous Cell Carcinoma of the Cervix; there is disorder in the formation of nest-cells hence there is different size and shape. Also the pattern left and right show somewhat surviving epithelial zones which do have varying degree of necrosis, while stroma retains sea of partially disconnected nest-cells created by massive necrosis. B: Adenocarcinoma (Endometrioid) of the cervix; the papillary nature maintained longitudinal nuclear grooves oriented while oval fashion is few. H & E stained. X40.
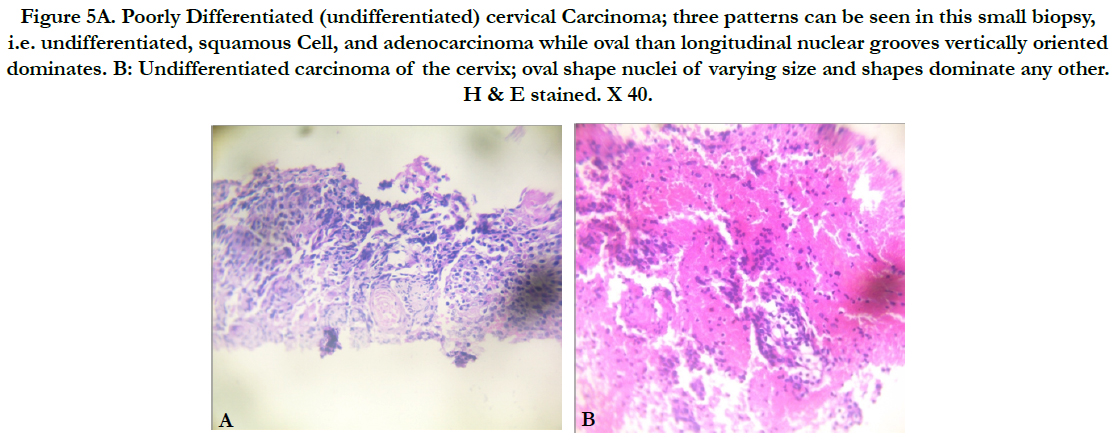
Figure 5A. Poorly Differentiated (undifferentiated) cervical Carcinoma; three patterns can be seen in this small biopsy, i.e. undifferentiated, squamous Cell, and adenocarcinoma while oval than longitudinal nuclear grooves vertically oriented dominates. B: Undifferentiated carcinoma of the cervix; oval shape nuclei of varying size and shapes dominate any other. H & E stained. X 40.
Figure 6A. Nuclear features in undifferentiated carcinoma of the cervix. H & E stain. B: Nuclei shapes with poorly differentiated (undifferentiated) carcinoma of the cervix. H &E stained. X40.
Discussion
The occurrence of uterine cervix diseases change and types appear to be more geographical than ethnic and when consideration alongside primary risk factors of infection or incidence of trauma, may also lack arguable merit in favour for genetic character constituents. From the study what appear to have changed were degree and rate of occurrence [24] as in tables I & II, and suggests that more women are responding with trust to Allopathic Medicare than traditional or they are gaining access to it now more than before or that there is improved method of medicare practice due to injection of new technology and staff in the system within this geographical zone (Figure 1). Hence more of cervical lesions were discovered as health care services are nearer to the general population now than before in the region. Therefore, in 18 years 2581 gynecological specimens from five hospitals domiciled in five States of the region were 58% cases of Igbo women found to have uterine cervical problems. Also the methods applied for sampling involved imaging save for 120 cases denied of ultrasound imaging for unstated reason. These methods were evident in another report where less significant changes in uterine cervical lesion types and degree of occurrence were recorded but had significance changes in rate of incidence [25]. Again, from our finding 96% of provisional diagnosis were accurate. This could be as a result of improved but appropriate technology application by good and efficient staff.
Cautious effort and diligence were taken to search out from 2581 specimens and records 1501 of uterine cervical diseases from Igbo women extraction. This was done to eliminate ethnic crossbred women population who are not needed in the study, thereby encouraging ethnic pathology study of uterine cervix diseases as is reported elsewhere for cancer of the cervix [26]. Finding is that six lesions of the cervix were benign types which have potentials to transform into cancer state, and three cancer types while figure 3A remained suspicious of sarcoma and is a case diagnosed of leiomyomatous polyp.
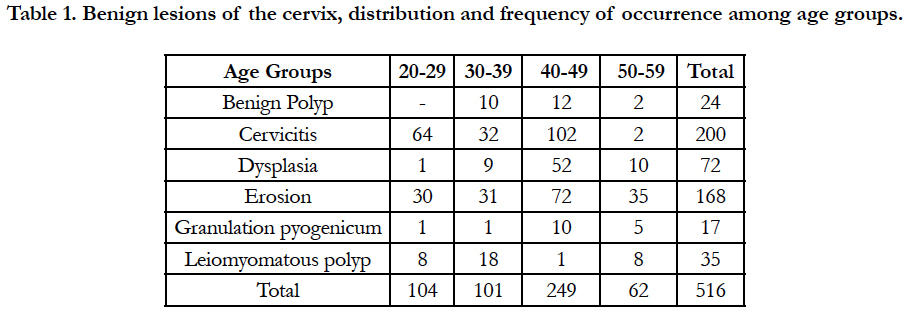
The occurrence and frequency rate of benign lesions of the uterine cervix in this study is worrisome considering that six lesions were present and is divided into growth and inflammatory. There was no evidence from clinical history that the development of any of the two types were associated with infection save for histomorphologic entities. However it has been reported that benign growths (leiomyomatous and benign polyps) are not caused by infectious microorganism but when same contaminates the growth and may cause transformation to cancer after continued cytolysis [27, 28]. In this study, known lesions caused by bacterial infection were found and all showed varied histomorphologic characters reviewed in the three types (Figures 1C, D & Table 1).
Of 516 patients with benign lesions in the study was found 131 with growths to which 46 of them occurred in age group 20- 29 and 30-39, and the rest in 40-49 and 50-59. These patterns of occurrence among age groups are pointer and incriminate age as factor to increasing benign lesions as reported by other investigators of precancerous lesions because of early diagnosis or screening [29]. These findings do suggest possibility of benign lesions being a precursor to age for transformation to cancer as patients growth are infected with microorganism (Figures 1A - D). Also considering that 159 with benign inflammatory lesions were caused by bacterial infection among age group 20-29 and 30-39 is significant when compared with age groups 40-49 and 50-59 which gave 85 cases. It therefore follows from this study that age and infection alone may not be main factor for benign lesion transformation into cancer scenario. After all, the potential for cellular transformation to occur can be traced to the process of interaction and possible physiology of the individuals. These can be possible even with benign cells as stated elsewhere [30-32]. Also other studies have shown evidence of these benign lesions give duo novo to cancer when there is active sustained factor [33]. Could it be that the two basic types of benign lesions (caused by micro-organism infection and occasioned by hormonal effects) have the same capability of transformation to cancer in this environment? Such capability is open to further investigation as it is necessary for prevention, important for treatment, and management of cancer out come.
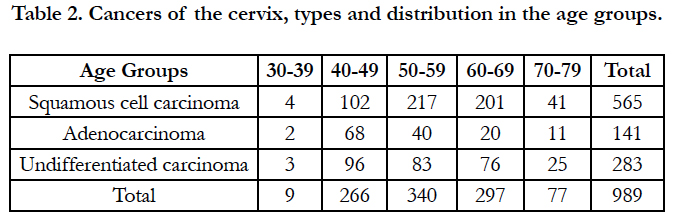
Three cancer types were observed in the study, with squamous cell carcinoma occurring most and are followed by undifferentiated carcinoma table 2. The trend has not change as given in this study as in other reports when patient at varying age group respond to cervical screening from region to region where such program is available [34, 35]. In deed what has changed is the rate within period as in this study and solution to abate it has not yielded either. From this study it can be said that the frequency of occurrence within 18 years is alarming and requires urgent attention to curb the menace.
In this study cancer types occurred from age group 30-39 to 70-79 showcasing an undulating frequency of distribution. Most affected age groups are 40-49, 50-59 and 60-69. The reason for such occurrence in this study is not unrelated to poverty and the insensitivity to growing health care campaign in the region even as health care bills scar relations to unpaid and uncared pensioners. The all important cervical cancer screening guideline in Nigeria lack effective adoption for implementation in this region and the neglect observed is vivid in procedural ablation, colposcopy and imaging unlike elsewhere [35]. Hence early detection of cervical cancer is not noted through screening as reports particularly in the western world.
Cautious effort was made to observe that certain nuclear features and arrangements modified pattern of cancer design of uterine cervix particularly with two types. The study of the entire slide helped to obviously identify four types of nuclear features of cancer of the cervix therefore avoiding subtype classification based on nuclear features. Most prominent and of frequent occurrence of them all is that displayed in poorly differentiated and undifferentiated figures 5 and 6. Such finding is classic and may be a pointer to the fact that one type could give room for the other to occur may be under a definite stimulus, or suggest the reason for rare occurrence of sarcomas within the cervix. In poorly differentiated patterns, nuclear features are important among other characteristic elements present to determine the degree of differentiation rather than only considering quantity of components as in figure 4A in this study.
Conclusion
It is obvious from this study that uterine cervix diseases occurrence and frequencies are not dependent on regional environment factors alone but may include histophysiologic stimulus and possibly sciophysiologic entities as precursors. The pattern of uterine cervix lesions may vary from one region to another which depends on all age groups and the health care standard. What seem to be racial factor is the environmental contribution in relation to sedentary lifestyle and individual hygiene which can precipitate factors discovered in this study. Uterine cervix lesions vary in occurrence and distribution among age groups have not changed. Hence the transformation of benign lesions of the cervix to cancer types is possible based on precursor acting on agents capable of producing inflammation and inducing physiologic change in time.
Pattern of histomorphologic features for individual lesion that occurred revealed subtypes at varying advances of change as are evident with nuclear features. Uterine cervix lesions distribution among age groups and incidence tend remain slightly unchanged in South-Eastern Nigeria when compared with elsewhere, but has changed in relation with previous reports in the region.
References
- Crum CP, Nuovo G, Friedman D, Silverstein SJ. Accumulation of RNA homologous to human papillomavirus type 16 open reading frames in genital precancers. J Virol. 1988 Jan;62(1):84-90. PubMed PMID: 2824859.
- Ferenczy A. Anatomy and histology of the cervix. InPathology of the female genital tract. Springer: New York, NY; 1977. p. 102-123.
- Nelson Jr JH, Averette HE, Richart RM. Cervical intraepithelial neoplasia (dysplasia and carcinoma in situ) and early invasive cervical carcinoma. CA: a cancer journal for clinicians. 1989 May;39(3):157-78.
- Kessler II. Perspectives on the epidemiology of cervical cancer with special reference to the herpesvirus hypothesis. Cancer Res. 1974 May;34(5):1091-110. PubMed PMID: 4366984.
- Fluhmann CF. The cervix uteri and its diseases. Saunders; 1961.
- Aaro LA, Jacobsen LG, Soule E. Endocervical polyps. Obstet Gynecol. 1963 Jun 1;21(6):659-65.
- Dougherty CM, Moore WR, Cotten N. Histologic diagnosis and clinical significance of benign lesions of the nonpregnant cervix. Ann NY Acad Sci. 1962 Sep 1;97(3):683-702.
- Lippert LJ, Richart RM, Ferenczy A. Giant benign endocervical polyp: report of a case. Am J Obstet Gynecol. 1974 Apr 15;118(8):1140-1. PubMed PMID: 4817652.
- Chirayil SJ, Tobon H. Polyps of the vagina: a clinicopathologic study of 18 cases. Cancer. 1981 Jun 15;47(12):2904-7. PubMed PMID: 7260876.
- Rilke F, Cantaboni A. Lipoma of the uterus. Presentation of 2 cases and a review of the recent literatures Am J Obset Gynecol. 1964 Aug;86:645.
- Patel DS, Bhagavan BS. Blue nevus of the uterine cervix. Hum Pathol. 1985 Jan;16(1):79-86. PubMed PMID: 3882546.
- Dundore W, Lamas C. Benign nevus (ephelis) of the uterine cervix. Am J Obstet Gynecol. 1985 Aug 1;152(7 Pt 1):881-2. PubMed PMID: 4025438.
- Luevano-Flores E, Sotelo J, Tena-Suck M. Glial polyp (glioma) of the uterine cervix, report of a case with demonstration of glial fibrillary acidic protein. Gynecol Oncol. 1985 Jul 1;21(3):385-90.
- Stout AP. Hemangio-endothelioma: a tumor of blood vessels featuring vascular endothelial cells. Ann Surg. 1943 Sep;118(3):445-64. PubMed PMID: 17858281.
- Selzer I, Nelson HM. Benign papilloma (polypoid tumor) of the cervix uteri in children: report of 2 cases. Am J Obstet Gynecol. 1962 Jul 15;84:165-9. PubMed PMID: 13910540.
- Abell MR. Papillary adenofibroma of the uterine cervix. Am J Obstet Gynecol. 1971 Aug 1;110(7):990-3. PubMed PMID: 5558981.
- Ng AB, Reagan JW, Yen SS. Herpes genitalis: Clinical and cytopathologic experience with 256 patients. Obstet Gynecol. 1970 Oct 1;36(4):645-51.
- Schaefer G. Tuberculosis of the female genital tract. Clin Obstet Gynecol. 1970 Dec 1;13(4):965-98.
- Reagan JW, Fu YS. The uterine cervix. In: Silverberg S. ed, Principles and practice of surgical pathology. New York: John Wiley & Sons; 1983. p. 1219-1263.
- Wenckebach GF, Curry B. Cytomegalovirus infection of the female genital tract. Histologic findings in three cases and review of the literature. Arch Pathol Lab Med. 1976 Nov;100(11):609-12. PubMed PMID: 185987.
- Crum CP, Nagai NO, Levine RU, Silverstein S. In situ hybridization analysis of HPV 16 DNA sequences in early cervical neoplasia. Am J Pathol. 1986 Apr;123(1):174-82. PubMed PMID: 2421580.
- Zur Hausen H. Papillomavirus infections - a major cause of human cancers. Biochim Biophys Acta. 1996 Oct 9;1288(2):F55-78. PubMed PMID: 8876633.
- Sykes NL Jr. Condyloma acuminatum. Int J Dermatol. 1995 May;34(5):297-302. PubMed PMID: 7541783.
- Hogewoning CJ, Bleeker MC, van den Brule AJ, Voorhorst FJ, Snijders PJ, Berkhof J, et al. Condom use promotes regression of cervical intraepithelial neoplasia and clearance of human papillomavirus: a randomized clinical trial. Int J Cancer. 2003 Dec 10;107(5):811-6. PubMed PMID: 14566832.
- Sasieni PD, Shelton J, Ormiston-Smith N, Thomson CS, Silcocks PB. What is the lifetime risk of developing cancer?: the effect of adjusting for multiple primaries. Br J Cancer. 2011 Jul 26;105(3):460-5. doi: 10.1038/bjc.2011.250. PubMed PMID: 21772332.
- Moyer VA. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2012 Jun 19;156(12):880-91, W312. doi: 10.7326/0003-4819-156-12-201206190-00424. PubMed PMID: 22711081.
- Winkler B, Crum CP. Chlamydia trachomatis infection of the female genital tract. Pathogenetic and clinicopathologic correlations. Pathology annual. 1987;22:193-223.
- Ezeama CO, Ikechebelu JI, Obiechina NJ, Ezeama NN. Clinical Presentation of Uterine Fibroids in Nnewi, Nigeria: A 5. year Review. Ann Med Health Sci Res. 2012 Jul;2(2):114-8. doi: 10.4103/2141-9248.105656. PubMed PMID: 23440007.
- Vizcaino AP, Moreno V, Bosch FX, MUNoz N, Barros‐Dios XM, Borras J, et al. International trends in incidence of cervical cancer: II. Squamouscell carcinoma. Int J Cancer. 2000 May 1;86(3):429-35. PubMed PMID: 10760834.
- Evans CS, Goldman RL, Klein HZ, Kohout ND. Necrobiotic granulomas of the uterine cervix. A probable postoperative reaction. Am J Surg Pathol. 1984 Nov;8(11):841-4.
- Davis JR, Steinbronn KK, Graham AR, Dawson BV. Effects of Monsel’s solution in uterine cervix. Am J Clin Pathol. 1984 Sep;82(3):332-5. PubMed PMID: 6380272.
- Campion MJ, McCance DJ, Cuzick J, Singer A. Progressive potential of mild cervical atypia: prospective cytological, colposcopic, and virological study. Lancet. 1986 Aug 2;2(8501):237-40. PubMed PMID: 2874275.
- Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999 Sep;189(1):12-9. PubMed PMID: 10451482.
- Patel A, Galaal K, Burnley C, Faulkner K, Martin-Hirsch P, Bland MJ, et al. Cervical cancer incidence in young women: a historical and geographic controlled UK regional population study. Br J Cancer. 2012 May 22;106(11):1753-9. doi: 10.1038/bjc.2012.148. PubMed PMID: 22531636.
- Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain J, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012 May-Jun;62(3):147-72. doi: 10.3322/caac.21139. PubMed PMID: 22422631.