Acute Toxicity by Hair Dye in Upper Egypt
Abdel-Moneim A*
Department of Forensic Chemistry, College of Forensic Sciences, Naif Arab University for Security Sciences, Riyadh, Saudi Arabia.
*Corresponding Author
Hatem Abdel Moniem Ahmed,
Department of Forensic Chemistry,
College of Forensic Sciences,
Naif Arab University for Security Sciences, Riyadh, Saudi Arabia.
Email: Hatemahmed29@yahoo.com
Hatemahmed29@nauss.edu.sa
Received: December 13, 2016; Accepted: January 09, 2017; Published: January 10, 2017
Citation: Abdel-Moneim A (2017) Acute Toxicity by Hair Dye in Upper Egypt. Int J Forensic Sci Pathol. 5(1), 305-311. doi: http://dx.doi.org/10.19070/2332-287X-1700069
Copyright: Abdel-Moneim A© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Hair-dye containing Para-phenylenediamine is widely used in Middle Eastern and some Asian countries. Many cases of toxicity and mortality either due to accidental or deliberate ingestion of hair dyes were reported. The aim of the present work is to study the clinical manifestation and common histopathological changes to various aspects of acute poisoning through a retrospective study of fatalities reported in seven governors in Upper in Egypt as a result of its ingestion and if there is a dose-effect relationship. The records of acute poisoning cases of seven governors in Upper Egypt investigated by Assiut forensic chemical laboratory in the period from January 2008 to December 2012 were examined as regards type of poison, pattern, incidence, age, sex, geographical distribution and mode of poisoning. The studying of the systemic effects of ingestion of hair dye was conducted by oral administration of hair dye in different doses (500, 200, 100, and 50 mg/ kg b.w.) to four groups of albino rats. The result, revealed that about a fifth of the acute poisoning fatalities investigated by Assiut forensic chemical laboratory were due to ingestion of hair dye. The highest majority of them were suicide cases, particularly in Quna, Sohag and Aswan Governorates respectively, with a female predominance. Death occurred within five minutes in the first group, within ten minutes in the second group and within an hour in the third group. The animals of the fourth group survived until sacrificed after one week. The most common histopathological changes in all studied organs were vascular congestion and lymphocyte infiltration, with degenerative changes in the hepatocytes and the destruction of the renal tubules. Deliberate self-poisoning by hair dye is a major problem in Upper Egypt particularly in females. The main toxic effects were directed to the liver and kidneys while the other studied organs were affected to a mild extent. Also, there was a well-established dose-effect relationship.
2.Introduction
3.Material and Methods
3.1.Chemicals
3.2.Samples
3.3.Cases
3.4.Studying of Acute Poisoning Fatalities
3.5.Studying of the Histopathological Effects of Ingesting of Hair Dye
4.Results and Discussion
4.1.Case Study
4.2.Toxicological Analysis
5.Conclusion
6.Acknowledgments
7.References
Keywords
P-Henylenediamine; Upper Egypt; Assiut Forensic Chemical Laboratory.
Introduction
Nowadays, millions of consumers use hair dye; all of them have the desire to improve their appearance. In general, cosmetics and their ingredients must have no harmful effects to human health, this property of cosmetics contradicts to drugs which when assessed a risk-benefit relationship is considered [1]. The researchers emphasized that Para-phenylenediamine (PPD) is the main toxic ingredient of hair dyes [2]. PPD is often found in permanent hair dyes, sometimes called “coal tar” dyes [3] and stone hair dye SHD [4]. PPD can be found in either black or red henna products [5], some of these products are produced in countries where they labeling and warning is sparse or non-existent. In France, Germany and Sweden, PPD was banned as a hair dye because it was thought to be too dangerous for health. PPD induced tissue damage result in hematological and biochemical changes. In treatment rats, there are a significant increases in the plasma enzymes AST, GPT, creatinine, glucose, and decreases in total proteins. PPD was not detected in the tissues of treated rats; these due to toxic effects which possibly produced by metabolites of PPD and not by the parent compound itself [6]. The most common histopathological changes in organs were vascular congestion and lymphocytic infiltration which may be attributed to inflammatory or hypersensitivity reaction [7]. Liver was found to be the target organ in PPD intoxication, that many degenerative changes appeared in the form of vacuolated cytoplasm and irregular deeply stained nuclei of the hepatocytes. Also when laboratory animals were fed with benzidine derived dyes, cancerous and precancerous liver conditions were found similar to the damage produced by known liver carcinogens, in addition to great quantities of benzidine were found in the urine of the dosed rats. The histopathological pattern of renal affection indicated the occurrence of acute tubular necrosis, which led to acute renal failure that may contribute to the occurrence of death. Acute tubular necrosis and renal failure as a result of exposure to PPD containing dye have been documented in several studies [8, 9]. The aim of this work, is to study the clinical manifestation and common histopathological changes to various aspects of acute poisoning and study their dose effect relationship.
All solvents were chemical grade from Sigma. Para-phenylenediamine (CAS no. 106-50-3, 97% pure, Aldrich), Methanol (Lichrosolv, HPLC grad > 99.8% pure), Second water obtained using a MilliQ system with Q-PAK Purification Paks (Millipore Corp., Bedford, MA.
Twenty five male guinea pigs weighing 250±150 g were procured from animal breeding unite of the Faculty of Medicine Assuit University – Assuit - Egypt and housed in an air-conditioned room and maintained on standard pellet diet and water. The animals were housed in cages provided with rice husk as bedding materials and kept under ambient temperature of 23 ± 2°C. The animals were kept in the laboratory condition for 1 week to adapt the climate condition and for the commencement of treatment protocol. The rats were divided into five groups (control and four test groups) on the basis of using the commercial hair dye as oral administration; each comprising six rats. (group 1, 2, 3, and 4) orally administered with (500, 200, 100 and 50 mg/kg b.w.) of commercial hair dye, respectively.
Ninety-five cases of fatal acute PPD poisoning were admitted to Upper Egypt hospitals (El-Minia, Assuit, Sohag, Qena and Aswan) for evaluation and management within the period 2009- 2015. Full autopsies were investigated by the office of the chief medical examiner, medico-legal department, and ministry of justice. The history, clinical manifestations and management were obtained from the clinical sheets of the cases from the receiving hospitals.
The records of fatalities due to acute poisoning by hair dye at five governors (El-Menia, Assuit, Sohage, Qena and Aswan) in Upper Egypt investigated by Assiut Forensic Chemical Laboratory in the period from January 2009 to December 2015 were examined as regards type of poison, pattern, incidence, age, sex, geographical distribution and mode of poisoning.
The studying of the systemic effects on ingestion of hair dye was conducted by oral administration of hair dye in different doses (50, 100, 200, 500 mg/kg b.w.) to four groups of albino rats, and distilled water for the control group. The clinical manifestations were observed, after sacrificed [10]. Small pieces of the liver, kidney, heart and lung were fixed at 10 % buffered formalin solution and then processed for the preparation of histopathological sections. After a routine processing, paraffin sections were cut at 5μm thickness and stained with haematoxylin and eosin for microscopic examination [11], and the light microscopic examination of sections of vital organs was done.
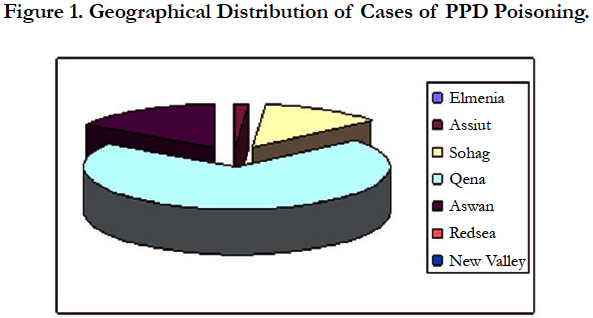
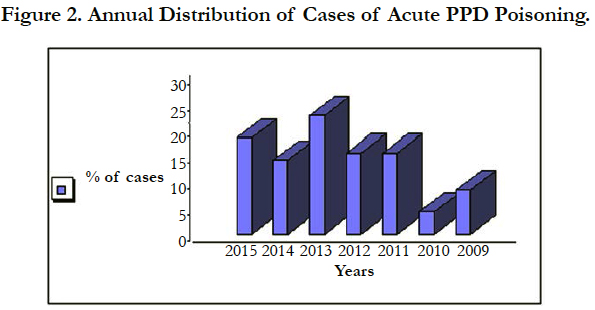
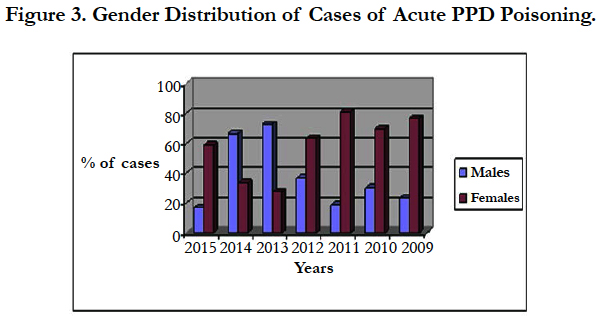
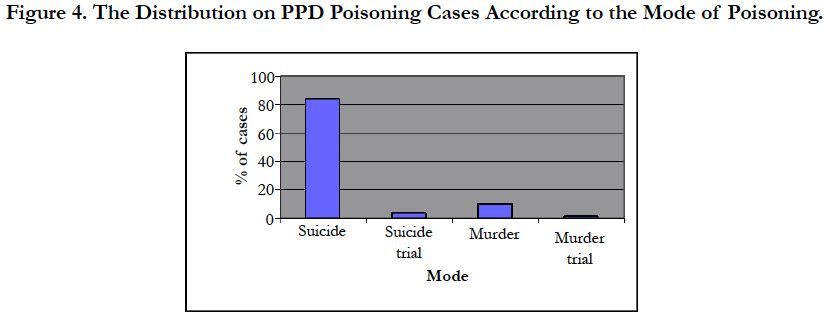
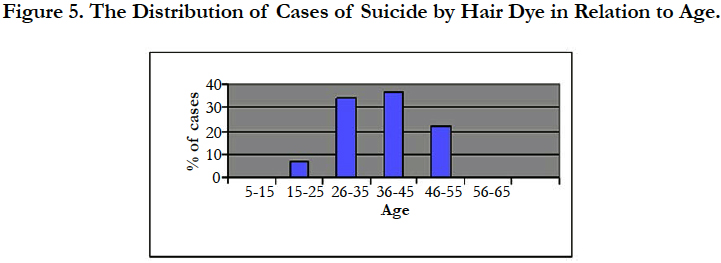
The examining of intense harming fatalities explored by Assiut Forensic Chemical Laboratory uncovered that around one fifth of the cases were because of ingestion of hair dye. The most noteworthy number of cases was found in Qena (70), Aswan (15.71), Sohag (12.86) Assiut (1.11) trailed by Elmina (0.32%) governorates as delineated in Figure 1, this concur with (Mohamed), who clarified by the way that the utilization of PPD as a hair color and as a restorative contrasts in ubiquity in various habitations where it is exceptionally utilized as a part of South Valley governorates [12]. The most astounding incidence was found in the year 2013 (25%), 2015 (19.5), 2012 (15.5), 2011 (14.81), 2014 (14.19), 2009 (6.89), trailed by 2010 (4.11%), Figure 2. The greater part of cases were suicidal cases Figure 4, this concur with (Mohamed) [12], concerning the way of death, the suicidal cases were the most elevated (91.7) trailed by homicidal (7.1) and in conclusion accidental (1.2%) [12], with a female's predominance (65.71%), Figure 3, this alluded to relationship amongst females and cosmetics when all is said in done and the inexpensiveness of this stone making it in the compass of their hands [12]. The highest percentage was found in the age group (36-45), (26-35), (46-55) years, trailed by (15-25) years, Figure 5.
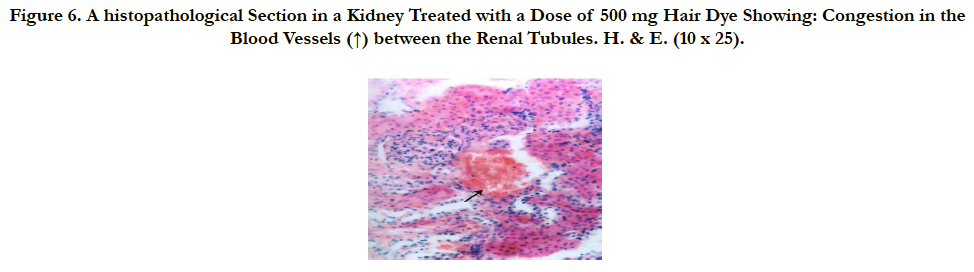
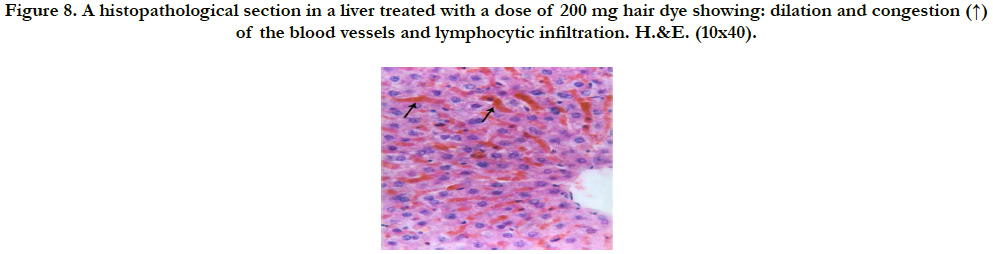
This study was done to assess the hair dye toxicity by utilizing commercial hair dye as a part of an approach to gauge the perils of this dye on rats, since it is realized that harmful impacts in people are for the most part in an indistinguishable range from those of trial creatures. PPD is the main constituent in hair dye and is an organic derivative of paranitroaniline, when ingested in a dose-dependent manner, results in severe hypersensitivity (itching, angioedema, asphyxia) and rhabdomyolysis (paresis of extremities, cola-colored urine, oliguria, markedly elevated creatinine phosphokinase and lactate dehydrogenase, hyperkalemia, hypophosphatemia and hypocalcaemia) [13, 14]. Different features, for example, iron deficiency, leukocytosis, hemoglobinemia, hemoglobinurea, and liver corruption have been accounted for [15]. In animal model, PPD induces rhabdomyolysis leakage of calcium ions from the smooth endoplasmic reticulum, followed by continuous contraction and irreversible structural changes in the muscles [16]. In this study, the ingestion of hair dye revealed that death occurred within five minutes in the first group, within ten minutes in the second group and within an hour in the third group, as dose application (500, 200 and 100 mg/kg b.w.), respectively. The animals of the fourth group survived until sacrificed after one week, (50 mg/kg b.w.). The most common histopathological changes in all studied organs were vascular congestion and lymphocyte infiltration [17]. The results revealed that the target organs of PPD were the liver and kidneys. The histological changes of the liver revealed severe vascular congestion of the blood sinusoids so that hepatocytes appeared smaller in comparison to those of the control liver [17]. The hepatocytes showed vacuolated cytoplasm and irregular deeply stained nuclei. The kidney showed destruction of the renal tubules, congestion of the glomerular capillaries and narrowing of the filtration spaces [17]. The cardiac muscle cells showed deeply stained nuclei and the muscle fibers were separated by wide spaces [17], Figures (6-17). The present study reveals the presence of a dose- effect relationship, the larger the dose; the earlier and more severe the effects.
Figure 6. A histopathological Section in a Kidney Treated with a Dose of 500 mg Hair Dye Showing: Congestion in the Blood Vessels (↑) between the Renal Tubules. H. & E. (10 x 25).
Figure 7. A histopathological section in a lung treated with a dose of 500 mg hair dye showing: congestion (↑) of the blood vessels and lymphocytic infiltration (Ly). H. & E. (10 x 25).
Figure 8. A histopathological section in a liver treated with a dose of 200 mg hair dye showing: dilation and congestion (↑) of the blood vessels and lymphocytic infiltration. H.&E. (10x40).
Figure 9. A histopathological section in a kidney treated with a dose of 200 mg hair dye showing: a slight congestion (↑) of the blood vessels between the renal tubules. The proximal convoluted tubules (P) show destructed brush border. H.&E. (10 x 25).
Figure 10. A Histopathological Section in a Lung Treated with a Dose of 200 mg Hair Dye Showing Vascular Congestion (↑) and Lymphocytic Infiltration (Ly). H. & E. (10 x 25).
Figure 11. A Histopathological Section in a Heart Treated with a Dose of 200 mg Hair Dye Showing Dilation of the Blood Vessels and Vascular Congestion (↑). H. & E. (10 x 25).
Figure 12. A Histopathological Section in a Suprarenal Gland Treated with a Dose of 200 mg Hair Dye Showing: a Slight Congestion (↑) of the Blood Capillaries between the Cells of the Suprarenal Cortex. H. & E. (10 x 25).
Figure 13. A Histopathological Section in a Cerebral Cortex Treated with a Dose of 200 mg Hair Dye Showing Vascular Congestion (↑) and Dilation of Blood Vessels. H. & E. (10 x 25).
Figure 14. A Histopathological Section in a Liver Treated with a Dose of 100 mg Hair Dye Showing: A Slight Dilation and Congestion (↑) of the Blood Vessels and Central Vein CV Compared to the Control Group. H.&E. (10 x 40).
Figure 15. A Histopathological Section in a Heart Treated with 100 mg Hair Dye showing that the Muscle Fibers are Separated by Wide Spaces (S). H. & E. (10 x 25).
Figure 16. A Histopathological Section in a Liver Treated with a Dose of 50 mg Hair Dye Showing: a Sight Dilation and Congestion (↑) of the Blood Vessels and Central Vein (CV) Compared with the Control Group. H. & E. (10x40).
Figure 17. A Histopathological Section in a Kidney Treated with a Dose of 50 mg Hair Dye Showing Destruction of the Brush Borders of the Proximal Tubules with Widening of the Lumen and Vascular Congestion of the Glomerular Capillaries and the Blood Vessels between the Renal Tubules H. & E. (10 x 25).
Conclusion
Deliberate self- poisoning by ingestion of hair dye is a major problem in Upper Egypt particularly in females. The main toxic effects were directed to the liver and kidneys while the other studied organs were affected to a mild extent. Also there was a wellestablished dose- effect relationship.
Acknowledgments
The author thankful to, Faculty of Medicine Assuit University – Assuit- Egypt, Assiut Forensic Chemical Laboratory, ministry of justice - Assuit- Egypt and the department of forensic chemistry, college of forensic sciences, Naïf Arab University for Security Sciences, for providing us the opportunity to pursue research and grateful to the president of Naïf Arab for Security Sciences forgive us this chance.
Ashraf W, Dawling S, Farrow LJ. Systemic paraphenylenediamine poisoning: A case report and review. Hum Exp Toxicol.1994; 13:167-170.
References
- Altekruse SF, Henley SI, Thun MJ (1999) Death from hematopoietic and other cancers in relation to permanent hair dye use in large prospective study. Cancer Causes and Control. 10(6): 617- 625.
- Oumeish YO (2001) The cultural and philosophical concept of cosmetics in beauty and art through the medical history of mankind. clin Dermatol. 19(4): 375.
- Drevitch G (2001) Body art or body mutilation. Scholastic choices. 16(5): 6-9.
- Hatem AMA, Ragaa MAM, Fathy FAL, Adel MKE, Kamal ME, et al., (2013) Different Analytical Methods of Para-Phenylenediamine Based Hair Dye. JCDSA. 3: 17-25.
- Txilar NC.2004; http://www.hennaforhair.com/ppd/08/26/04, p: 1.
- Saad H, Musa A, Badreldin, Mohamed BA (2000) Some Toxicological Observations on Paraphenyl Diamine (Hair Dye) in Rats and Chickens. Pak J Biol Sci. 3(6): 953-956.
- Rajka C, Blohm SG (1970) The allergenicity of paraphenylenediamine. Acta Dermatolo- Venercologia. 50: 51.
- Kallel H, Chelly H, Dammak H, Bahloul M, Ksibi H, et al., (2005) Clinical manifestations of systemic paraphenylenediamine intoxication. J Nephrol. 18(3): 308-11.
- Salma MS, Mirghani F, Mohamed EN, Musa AR, Babiker M, et al., (11995) Poisoning with hair dye containing paraphenylene diamine: ten years’ experience. Saudi J Kidney Dis Transplant. 6(3): 286-9.
- Bryan BT, Tim CM, Paul T (1993) General and Applied Toxicology. 1: 233.
- Mc Manus JF, Mowry RW (1965) Staining methods. Histological and Histochemical. Harper and Row, New York. 136.
- Dressler W (1999) Hair dye Absorption. Bronough R L, Maibach H I, (Eds). Percutaneous Absorption, Drud and the Pharmaceutical Sciences. Marcel Dekker, New York, Basel. 685-716.
- Sandeep Reddy Y, Abbdul Nabi S, Apparao C, Srilatha C, Manjusha Y, et al., (2012) Hair dye related acute kidney injury--a clinical and experimental study. Ren Fail. 34(7): 880-884.
- Soni SS, Nagarik AP, Dinaker M, Adikey GK, Raman A (2009) Systemic toxicity of paraphenylenediamine. Indian J Med Sci. 63(4): 164-166.
- Singla S, Miglani S, Lal AK, Gupta P, Agarwal AK (2005) Para-phenylenediamine (PPD) poisoning. JIACM. 6(3): 236-238.
- Curtis DK, Mary OA, John Doull (1986) Casarett and Doulls Toxicology- The basic Science of Poisons. 3rd (Edn), Macmillan Publ co., New York.
- Ajay Pal Singh, Jatav OP, Manish D (2009) Myocarditis in hair dye poisoning. Indian Heart J. 61(3): 306- 307.