Assessment of Knowledge and Patient Counseling to the Patient with Diabetes on Diabetic Foot Care in Tertiary Care Hospital
Dr. Udaya Bhaskar A1*,Dr. Venkata Sankar Reddy K1, Dr. Praneeth Sagar K1, Dr. Kishore K1, Dr. Madhan Mohan Rao M2, Chinni Krishna V3
1 Annamacharya College of Pharmacy, Rajampet, A.P, India. JNTU, Ananthapur, A.P, India.
2 Associate Professor, Department of General Medicine, Rajiv Gandhi Institute of Medical Sciences, Kadapa, A.P, India.Dr. NTR University of Health Sciences. Vijayawada, A.P, India.
3 Associate Professor, Department of Pharmacology, Annamacharya College of Pharmacy, Rajampet, A.P, India. JNTU, Ananthapur, A.P, India.
*Corresponding Author
Dr. Annamaraju Udaya Bhaskar, Pharm D.
Annamacharya College of Pharmacy, Rajampet, A.P, India.
Tel: 7674044126
E-mail: udaybhaskar606@gmail.com
Dr. Venkata Sankar Reddy K, Pharm D.
Annamacharya College of Pharmacy, Rajampet, A.P, India.
Tel: 9908807084.
E-mail: venkatasankarreddyk@gmail.com
Received: January 07, 2019; Accepted: February 14, 2019; Published: February 20, 2019
Citation: Dr. Udaya Bhaskar A, Dr. Venkata Sankar Reddy K, Dr. Praneeth Sagar M, Dr. Kishore K, Dr. Madhan Mohan Rao M, Dr. Chinni Krishna V. Assessment of Knowledge and Patient Counseling to the Patient with Diabetes on Diabetic Foot Care in Tertiary Care Hospital. Int J Diabetol Vasc Dis Res. 2019;7(1):223-242. doi: dx.doi.org/10.19070/2328-353X-1900045
Copyright: Dr. Udaya Bhaskar, Dr. Venkata Sankar Reddy KA© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
To measure the awareness among diabetes patient related to diabetic foot. To counsel diabetic patients who are lacking awareness about their disease, medications and Lifestyle modifications. To minimize the diabetic foot amputations and diabetes complications.
2.Introduction
3.Classification Of Diabetes Mellitus
4. Epidemiology of Diabetes
5. Classification of Diabetic Foot Ulcers
6. Etiopathogenesis of Giabetic Foot Lesions
7. The Major challenges Relating to Diabetes Foot are
8. Factors increasing the Risk of Diabetic Foot Ulceration
9. Treatment Goals of Diabetic Foot Wound
10. Prevention Programmes of Diabetic Foot Ulcers
11. Patient Foot Care Education
12. Literature Survey
13. Experimental Work
14. Experimental Results
15. Discussion Of Results
16. Summary
17. Research Outcome
18. References
Abbreviations
HDL: High-Density Lipoprotein; GDM: Gestational Diabetes; WHO: World Health Organization; IDF: International Diabetes Federation; DM: Diabetes Mellitus; DFU: Diabetic Foot Ulcers; PVD: Peripheral Vascular Disease; PAD: Peripheral Arterial Disease; PN: Peripheral Neuropathy; PVD: Peripheral Vascular Disease.
Introduction
Diabetes mellitus is a metabolic disorder characterized by chronic hyperglycemia with disturbances of carbohydrate, fat and protein metabolism resulting from defects in insulin secretion, insulin action, or both [1]. Diabetes is a chronic disease that occurs when the pancreas does not produce enough insulin, or alternatively, when the body cannot effectively use the insulin it produces.
The chronic hyperglycemia of diabetes is associated with long-term damage, dysfunction, and failure of various organs, especially the eyes, kidneys, nerves, heart, and blood vessels. Several pathogenic processes are involved in the development of diabetes. These range from autoimmune destruction of the β-cells of the pancreas with consequent insulin deficiency to abnormalities that result in resistance to insulin action. The basis of the abnormalities in carbohydrate, fat, and protein metabolism in diabetes is deficient action of insulin on target tissues. Deficient insulin action results from inadequate insulin secretion and/or diminished tissue responses to insulin at one or more points in the complex pathways of hormone action [1, 2].
Impairment of insulin secretion and defects in insulin action frequently coexist in the same patient, and it is often unclear which abnormality, if either alone, is the primary cause of the hyperglycemia. Symptoms of marked hyperglycemia include polyuria, polydipsia, weight loss, sometimes with polyphagia, and blurred vision. Impairment of growth and susceptibility to certain infections may also accompany chronic hyperglycemia.
Acute, life-threatening consequences of uncontrolled diabetes are hyperglycemia with ketoacidosis or the nonketotic hyperosmolar syndrome. Long-term complications of diabetes include retinopathy with potential loss of vision; nephropathy leading to renal failure; peripheral neuropathy with risk of foot ulcers, amputations, and Charcot joints; and autonomic neuropathy causing gastrointestinal, genitourinary, and cardiovascular symptoms and sexual dysfunction. Patients with diabetes have an increased incidence of atherosclerotic cardiovascular, peripheral arterial, and cerebrovascular disease. Hypertension and abnormalities of lipoprotein metabolism are often found in people with diabetes [1-3].
In some individuals with diabetes, adequate glycemic control can be achieved with weight reduction, exercise, and/or oral glucose lowering agents. These individuals therefore do not require insulin. Other individuals who have some residual insulin secretion but require exogenous insulin for adequate glycemic control can survive without it. Individuals with extensive β-cell destruction and therefore no residual insulin secretion require insulin for survival. The severity of the metabolic abnormality can progress, regress, or stay the same [1-3].
Classification Of Diabetes Mellitus
The disease states underlying the diagnosis of diabetes mellitus are classified into four categories: type 1, insulin-dependent diabetes; type 2, noninsulin-dependent diabetes; type 3, other; and type 4, gestational diabetes mellitus (Expert Committee, 2003).
The hallmark of type 1 diabetes is selective β-cell destruction and severe or absolute insulin deficiency. Administration of insulin is essential in patients with type 1 diabetes. Type 1 diabetes is further subdivided into immune and idiopathic causes. The immune form is the most common form of type 1 diabetes.
Although most patients are younger than 30 years of age at the time of diagnosis, the onset can occur at any age. Type 1 diabetes is found in all ethnic groups, but the highest incidence is in people from northern Europe and from Sardinia. Susceptibility appears to involve a multifactorial genetic linkage but only 10-15% of patients have a positive family history [1, 2].
Type 2 diabetes is characterized by tissue resistance to the action of insulin combined with a relative deficiency in insulin secretion. A given individual may have more resistance or more β-cell deficiency, and the abnormalities may be mild or severe. Although insulin is produced by the β-cells in these patients, it is inadequate to overcome the resistance, and the blood glucose rises. The impaired insulin action also affects fat metabolism, resulting in increased free fatty acid flux and triglyceride levels and reciprocally low levels of high-density lipoprotein (HDL).
Individuals with type 2 diabetes may not require insulin to survive, but 30% or more will benefit from insulin therapy to control the blood glucose. It is likely that 10-20% of individuals in whom type 2 diabetes was initially diagnosed actually have both type 1 and type 2 or a slowly progressing type 1, and ultimately will require full insulin replacement. Although persons with type 2 diabetes ordinarily do not develop ketosis, ketoacidosis may occur as the result of stress such as infection or use of medication that enhances resistance, eg, corticosteroids. Dehydration in untreated and poorly controlled individuals with type 2 diabetes can lead to a life-threatening condition called nonketotic hyperosmolar coma. In this condition, the blood glucose may rise to 6-20 times the normal range and an altered mental state develops or the person loses consciousness. Urgent medical care and rehydration is required [1, 2].
The type 3 designation refers to multiple other specific causes of an elevated blood glucose: non-pancreatic diseases, drug therapy [1].
Gestational diabetes (GDM) is defined as any abnormality in glucose levels noted for the first time during pregnancy. Gestational diabetes is diagnosed in approximately 4% of all pregnancies in the USA. During pregnancy, the placenta and placental hormones create an insulin resistance that is most pronounced in the last trimester. Risk assessment for diabetes is suggested starting at the first prenatal visit. High-risk women should be screened immediately. Screening may be deferred in lower-risk women until the 24th to 28th week of gestation [3].
Epidemiology of Diabetes
Diabetes is a complex metabolic disease which can give rise to many circulatory and neurological disorders. According to the report of World Health Organization (WHO) the number of diabetic patients in 2000 reached to 171 million [4] and was predicted to increase 380 million by 2025. So, at now in most countries diabetes is becoming as an epidemic disorder.
Diabetic has become a problem of great magnitude recently. It is estimated that 10-12% of the urban and 4-6% of rural population of India are now diabetic. DM has emerged as a major health care problem in India. According to diabetes atlas published by international diabetic federation (IDF) there were estimated 40 million people with diabetes in 2007 and this number predicted to rise to almost 70 million people by 2025.
The countries with largest number of diabetes will be in India, China and USA by 2030. It is estimated that every 5th person with diabetes will be an Indian [5]. India is known as the “diabetes capital” of the world with more than 40 million people with diabetes [6].
A study was conducted to estimate the prevalence of diabetes and the number of all age which diabetes for year 2000 and 2030. The prevalence of diabetes for all age group world wide was estimated to be 2.8% in 2000 and 4.4% in 2030 the total number of people with diabetes project to rise from 171 million in 2000 to 366 million in 2030 [4].
The Even minor trauma can lead to infection of foot ulcers and amputation is major course of morbidity, disability and cost for people with diabetes mellitus. Ultimately, diabetes prevention needs “political will”, societal and community support and behavioral change on the part of individual and their families. Now is the time for India to wake up to the imminent problem of diabetes mellitus and act - before it is too late [7].
Diabetic Foot
Diabetic foot is defined by WHO as foot in diabetics with neurologic disorders, some degree of vascular involvement with or without metabolic complications of diabetes in lower extremity and prone to infection, scarring, with or without deep tissue damage [8].
One of the most important and disabling complications of diabetes mellitus (DM) is the diabetic foot ulcers (DFU). Development of DFU is traditionally believed to result from a combination of oxygen deficiency caused by peripheral vascular disease, peripheral neuropathy, minor foot traumas, foot deformities, and infection [32-35].
During the life span of a diabetic patient, the danger of ulcerations to the lower foot is as high as 25% [10]. In some studies saying that DFU, incidence of 1-4%, and prevalence of 5.3% to 10.5% [36, 37] in all diabetic patients, accounts for more than half of the non-traumatic lower-extremity amputations in the world [38-42]. Globally, one lower limb is lost every 30 seconds because of DFU [43]. The range of mortality following diabetic foot amputation is 39-80% after 5 years, which is worse than the mortality rate for most malignancies [36].
One-third of all diabetic patients have significant peripheral neuropathy and/or peripheral vascular disease (PVD). Diabetic foot problems are the commonest reason for hospitalization of diabetic patients (about 30% of admissions) and absorb some 20% of the total health-care costs of the disease more than all other diabetic complication [54, 55]. In India prevalence of foot ulcers in diabetic patients in clinic population is 3%, which is much lower than reported in the western world. A possible reasoning for the low prevalence in Indians is younger age and shorter duration of diabetes [56, 57]. PVD has been reported to be low among Asians [58-61] ranging between 3-6% as against 25-45% in Western patients [62-64].
The prevalence of PVD increases with advancing age and is 3.2% below 50 years of age and rises to 55% in those above 80 years of age [65] Similarly it also increases with increased duration of diabetes, 15% at 10 years and 45% after 20 years [66].
Ulcers of the low foot are generally related to an increased danger of amputation due to loss of sensitivity and bad hemostasis; conditions that, if combined with long term bad control of the blood glucose, create the necessary substratum for trauma infection and gangrene [10].
Foot ulcers and their complications are an important cause of morbidity and mortality in patients with diabetes. Annual incidence of foot ulcers is 1% to 4% and prevalence 5% to 10% in patients with diabetes [11]. About 50% of patients undergoing non-traumatic lower limb amputations have diabetes [12]. These patients have a high mortality following amputation, ranging from 39% to 80% at 5 years [11].
Diabetic foot ulcer is the most general cause of hospitalization in diabetic patients [21]. On the other hand, these ulcers can lead to infection, gangrene, amputation and even death if the necessary care is not provided [22]. In addition, lower extremity amputation is associated with prolonged hospitalization and rehabilitation and also is required to home care and social support [23]. Overall, the rate of lower limb amputation in diabetic patients is 10-30 times higher than non diabetics [24, 25]. The studies showed that every 30 seconds one leg is amputated due to diabetes in the world [26]. In the first two years after amputation, there is a 50 percent risk of re-amputation [27] and three years after lower limb amputation, 50% of patients may be dead [28]. The prevalence of diabetic foot in Iran was estimated at 3% in 2001 [29].
Approximately, 20% of hospital admissions among diabetic patients are in consequence of foot problems [44]. Furthermore, DFU is among the most prevalent causes of hospitalization and morbidity [41, 45] and is responsible for more days of hospital stay than any other chronic complication of DM [46, 47].
Foot ulcers can cause severe disability and hospitalization to patients and considerable economic burden to families and health systems [81, 82]. Infection, occurring in about half of the diabetic foot ulcers, is a further complication [48, 83]. About 85% of diabetes-related amputations are preceded by foot ulcers, and it accounts for more than half of non-traumatic lower limb amputations [83, 84]. Individuals who develop foot ulcers have a decreased health-related quality of life [16, 73].
Diabetic foot and also cause to impose heavy economic burden on the health system [19]. Among diabetes’ complications, different types of foot problems such as ulcers and infections are common and it has shown an increasing trend in the past decade [20].
DFU lesions are significant health and socioeconomic problem as they exert adverse effects on patients’ quality of life and impose heavy economic burden on the patient and the state due to rising the need for rehabilitative and home care services [48, 49]. Given the DFU’s high prevalence, heavy burden, and severe impact on patients’ life quality, it is advisable that sufficient heed be paid to prevention of this particular complication of DM. Furthermore, while effective treatment and formulation of prevention guidelines require a thorough understanding of characteristics of DFU patients and their ulcers.
The cost of care for amputation is financially great for both the patient and the healthcare provider with surgery, post-operative care followed by rehabilitation and the need for adaptations to home and prosthesis fitting. But the personal involvement to the patient in pain, loss of mobility, even life-long dependence on others and limitations imposed by the change of role is incalculable (ICDF) [80].
The treatment of diabetic foot is expensive all around the world. In developed countries, more than 5% of diabetics have foot ulcers and 20% of total health care resources spent on care of the diabetic foot in these countries.
High economic burden for solving this problem requires close collaboration among health system and people; develop national and international strategies and interaction with other health team members. By this approach, providing adequate and effective health services are necessary for patients and their families Also, improving the quality of clinical performance can lead to changes in client and patient societies [18].
Most of the patients developed DFU in 5th and 6th decades of their life, with the mean age being 59.3 years. Other studies also have found the average age of developing DFU to be about 55-60 years [50-53].
Poor knowledge of foot care and poor foot care practices were identified as important risk factors for foot problems in diabetes [17]. Evidence suggests that consistent patient education with prophylactic foot care for those judged to be at highest risk may reduce foot ulceration and amputations [28].
The most important point is that 85% of diabetic foot amputations are preventable with appropriate care and education [30]. Ideal management for prevention and treatment of diabetic foot is as follow: regular perception of foot, determine at risk foot, education to patient and health staff, appropriate foot coverage, and early treatment of foot problems [31].
As a result, educating medical and nursing personnel, applying screening and prevention guidelines, and allocating more resources are of great importance in treatment of DFU patients.
Classification of Diabetic Foot Ulcers
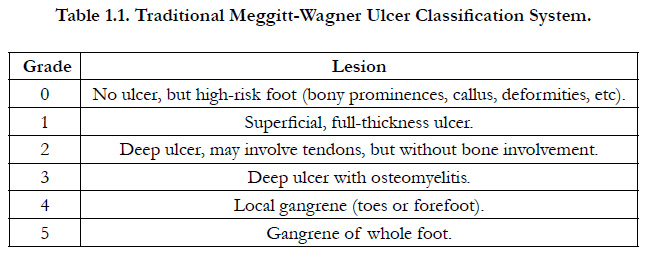
Classification systems grade ulcers (Table-1.1) and wound (Table-1.2) according to the presence and extent of various physical characteristics, such as size, depth, appearance and location.
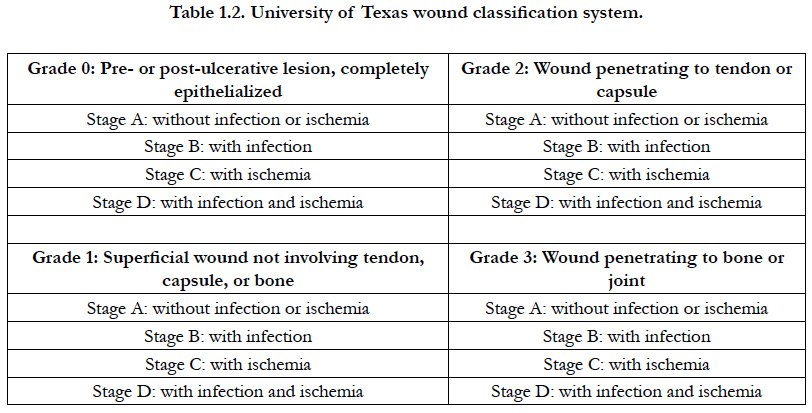
In most patients, peripheral neuropathy and peripheral arterial disease (PAD) (or both) play a central role and DFUs are therefore commonly classified as:
Neuropathic
Ischaemic
Neuroischaemic (Figures 1.1–1.3).
Neuroischaemia is the combined effect of diabetic neuropathy and ischaemia, whereby macrovascular disease and, in some instances, microvascular dysfunction impair perfusion in a diabetic foot [77, 78].
Charcot joint is a form of neuroarthropathy that occurs most often in the foot and in people with diabetes. Nerve damage from diabetes causes decreased sensation, muscle atrophy and subsequent joint instability, which is made worse by walking on an insensitive joint. In the acute stage there is inflammation and bone reabsorption, which weakens the bone. In later stages, the arch falls and the foot may develop a ‘rocker bottom’ appearance (Figure: 1.4-1.6). Early treatment, particularly offloading pressure, can help stop bone destruction and promote healing [77].
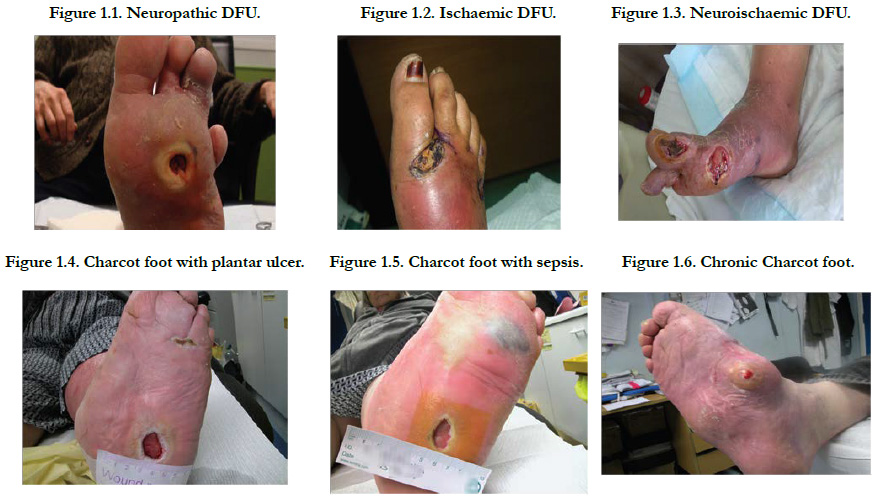
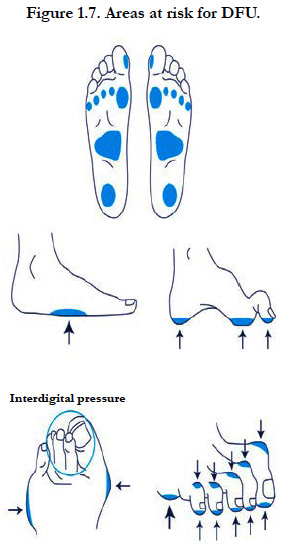
Foot deformity; A combination of motor neuropathy, cheiroarthropathy and altered gait patterns are thought to result in the “high risk” neuropathic foot with clawing of the toes, prominent metatarsal heads, high arch and small muscle wasting. Callus forms under weight-bearing areas (Figure: 1.7) as a consequence of dry skin (autonomic dysfunction), insensitivity and repetitive moderate stress from high foot pressure. It acts as a foreign body and cause ulceration [78].
Etiopathogenesis of Giabetic Foot Lesions
Diabetic foot ulcers result from the simultaneous action of multiple contributing causes [67, 68]. The major underlying causes are noted to be peripheral neuropathy and ischemia from peripheral vascular disease [69].
More than 60% of diabetic foot ulcers are the result of underlying neuropathy [69, 70]. The development of neuropathy in affected patients has been shown in animal and in vitro models to be a result of hyperglycemia-induced metabolic abnormalities [71-73]. One of the more commonly described mechanisms of action is the polyol pathway [72]. In the development of neuropathy, the hyperglycemic state leads to an increase in action of the enzymes aldose reductase and sorbitol dehydrogenase. This results in the conversion of intracellular glucose to sorbitol and fructose. The accumulation of these sugar products results in a decrease in the synthesis of nerve cell myo inositol, required for normal neuron conduction.
Additionally, the chemical conversion of glucose results in a depletion of nicotinamide adenine dinucleotide phosphate stores, which are necessary for the detoxification of reactive oxygen species and for the synthesis of the vasodilator nitric oxide. There is a resultant increase in oxidative stress on the nerve cell and an increase in vasoconstriction leading to ischemia, which will promote nerve cell injury and death.
Hyperglycemia and oxidative stress also contribute to the abnormal glycation of nerve cell proteins and the inappropriate activation of protein kinase C, resulting in further nerve dysfunction and ischemia.
Neuropathy in diabetic patients is manifested in the motor, autonomic, and sensory components of the nervous system [69]. Damage to the innervations of the intrinsic foot muscles leads to an imbalance between flexion and extension of the affected foot. This produces anatomic foot deformities that create abnormal bony prominences and pressure points, which gradually cause skin breakdown and ulceration.
Autonomic neuropathy leads to a diminution in sweat and oil gland functionality. As a result, the foot loses its natural ability to moisturize the overlying skin and becomes dry and increasingly susceptible to tears and the subsequent development of infection.
The loss of sensation as a part of peripheral neuropathy exacerbates the development of ulcerations. As trauma occurs at the affected site, patients are often unable to detect the insult to their lower extremities. As a result, many wounds go unnoticed and progressively worsen as the affected area is continuously subjected to repetitive pressure and shear forces from ambulation and weight bearing.
Peripheral arterial disease (PAD) is a contributing factor to the development of foot ulcers in up to 50% of cases [74, 75]. It commonly affects the tibial and peroneal arteries of the calf. Endothelial cell dysfunction and smooth cell abnormalities develop in peripheral arteries as a consequence of the persistent hyperglycaemic state [71]. There is a resultant decrease in endothelium-derived vasodilators leading to constriction. Further, the hyperglycemia in diabetes is associated with an increase in thromboxane A2, a vasoconstrictor and platelet aggregation agonist, which leads to an increased risk for plasma hypercoagulability [76]. There is also the potential for alterations in the vascular extracellular matrix leading to stenosis of the arterial lumen [76].
Moreover, smoking, hypertension, and hyperlipidemia are other factors that are common in diabetic patients and contribute to the development of PAD [67]. Cumulatively, this leads to occlusive arterial disease that results in ischemia in the lower extremity and an increased risk of ulceration in diabetic patients.
Diabetic peripheral neuropathy is one of the most common predisposing factors leading to foot ulceration and is the most common cause of hospital admissions in patients with diabetes. People with diabetes are 50 times more likely to develop a foot ulcer than non-diabetics (IWGDF 2007) [79].
Neuropathy, mechanical stresses, and angiopathy are the major etiopathological factors in the development of foot ulcers in people with diabetes [85]. Diabetic peripheral neuropathy is a heterogeneous disorder that includes mononeuropathies, polyneuropathies, plexopathies, and radiculopathies [86]. As diabetic neuropathy frequently leads to foot ulcer, it is recommended to screen all individuals with diabetes at least annually [87]. Of all the complications of diabetes, those that occur in the foot are considered the most preventable.
The Major challenges Relating to Diabetes Foot are
1. Foot ulceration is common, affecting up to 25% of patients with diabetes during their lifetime [49].
2. Over 85% of lower limb amputations are preceded by foot ulcers and Diabetes remains a major cause of non-traumatic amputation across the world with rates being as much as 15 times higher than in the non-diabetic population.
3. Strategies aimed at preventing foot ulcers are cost-effective and can even be cost saving if increase education and effort are focused on those patients with recognized risk factors for the development of foot problem [89].
4. Prevention is the first step towards solving diabetic foot problems. Although it was estimated that an ankle is lost to diabetes somewhere in the world every 30 seconds, a more
important fact is that up to 85% of all amputations in diabetes should be preventable [88].
5. Diabetes is now the most common cause of Charcot neuroarthropathy in Western countries, another condition that should be generally preventable [90].
Factors increasing the Risk of Diabetic Foot Ulceration
The risk factors for each of the above mentioned complications are:
Unmodifiable risk factors:
1. Disease duration
2. Age
3. Heredity
4. Gender (most common in men)
5. Race (e.g. African Americans)
6. Height
Modifiable risk factors:
1. Hyperglycemia
2. High blood pressure (mainly diastolic)
3. Dyslipidemia
4. Abnormal microcirculation (modifiable with anticoagulant treatment)
5. Use of alcohol
1. Smoking
2. Dyslipidemia
3. Hypertasis
4. Atherosclerosis
5. Peripheral neuropathy
6. Gender (most common in men)
7. Obesity
8. Way of life
9. Hyperglycemia
10. Hyperinsulinemia
11. Homocysteine.
Successful diagnosis and treatment of patients with DFUs involves a holistic approach that includes:
Optimal diabetes control
Effective local wound care
Infection control
Pressure relieving strategies
Restoring pulsatile blood flow
Treatment Goals of Diabetic Foot Wound
To improve function and quality of life.
To control infection.
To maintain health status.
To prevent amputation.
To reduce costs.
Prevention Programmes of Diabetic Foot Ulcers
Most of the ulcerations heal, 70% of the cases recur, frequently progressing to unavoidable limb amputation. Several factors are involved in the development of this process which include Peripheral Neuropathy (PN), Peripheral Vascular Disease (PVD), limited joint mobility and repeated trauma from abnormal load distribution on the foot [13, 14]. However, this unfavorable progression can be modified provided effective preventive measures are adopted such as adequate guidance regarding:
1) Lack of sensitivity and/or presence of peripheral vascular disease and its implications,
2) Hygiene and moisturizing practices,
3) Use of adequate footwear (when indicated),
4) Mandatory daily self-care (self-examination).
These guidelines should be extended to family members and caregivers as many diabetic patients at risk for complications such as obesity are frequently impaired for fulfilling self-examination. Therefore, preventive and care practices should provide guidance on the correct way to wash, dry and moisturize the feet as well as on how to cut nails and not trim cuticles, or use pumice stones and similar abrasive objects, use appropriate footwear, perform regular foot and footwear inspection and never walk barefoot [15-17].
Evidently, steps need to be taken towards two basic directions:
A. Creation of Health Structures, Health Professionals Awareness.
B. Training the patients.
The Diabetic Foot World Organization recommends: yearly examinations of the low foot for every diabetic and training in self care, every 3 months examination for patients with an ulcer, neuropathy or malformation history. In cases of ulcer relapse the patient needs to visit a specialized doctor within 2 weeks.
Studying the medical records one year before and three months after the seminar has shown improvement, as far as practical care of the diabetic foot is concerned, on matters of:
1. Patients’ training by health professionals on care of the diabetic foot.
2. Diagnosis and record of the peripheral vascular disease.
3. Record of the practices of self care of the diabetic foot.
4. Reference to the appropriate special podiatrists and diabetologists whenever necessary.
The American “Orthopedic Foot and Ankle” Society has developed specific guidelines for the health professionals aiming at the prevention of diabetic foot ulcers.
Some of those are:
A. Screening examinations for
- Evaluation of peripheral neuropathy
- Evaluation of skin integrity
- Evaluation of ulcers and wounds
- Malformations
- Vascular insufficiency
- Special shoes
B. Training patients in order to self examine their low foot and for special practices of self care. Individual special care should be taken for peripheral neuropathy patients.
C. Treatment: to be determined by the level of risk as defined by the presence of peripheral neuropathy, malformations and the history of ulcers. It combines:
- Training patients
- Orthoses
- Special shoes
- Charters of continuous care of nails and skin.
Ulcer care consists of:
1. Calluses care
2. Surgical cleaning of infected or dead tissues
3. Dressing
4. Member discharge.
Basic steps to be taken by every patient:
1. Observing the blood glucose levels and maintaining it within the natural limit
2. Proper eating and exercising
3. Quit smoking [101].
1. Since you could not be able to feel minor injuries, check your feet every morning, before you put on your shoes. Do the same each night before you go to bed. Check for red spots, wounds, blisters, even for small ones. Do not forget to check between your toes and your sole. If you are unable to do so yourself, ask someone else to help you.
2. Keep your toe nails cut. If you can do so yourself, use a nailclipper and polish the edges with a nail-file. Do not cut the nails in a round shape as this may lead the nail entering the skin. If you are unable to do so yourself, ask a specialist to do it.
3. Ask your doctor to examine your foot every 3 to 6 months, or more often if there are problems. Do not try to extract calluses on your own. Every time you visit your doctor take your shoes off in order to remind him to check your feet.
4. Take foot-baths every day using warm water (29–35°C). Do not use hot water as it can cause burns without you realising it. Dry your feet well when you finish, especially between your toes. Apply hydrating cream on the top and bottom of your feet, but not between your toes.
5. If you can, keep your feet up while seating. Do not cross your legs to your knees or ankles, since this obstructs blood circulation. Move your heel and toes up and down 2 or 3 times a day for 5 min. Do not use warm blankets, as they may cause burns without you realising it [101].
1. Always wear comfortable shoes that fit your foot well. Make sure there is enough space for your toes. Avoid sandals, openfront shoes or shoes with lasses between the toes. Never walk barefoot.
2. Wear clean cotton socks every day and make sure that they are not tight under your knee. If you wear panty hose make sure they are not too tight and they do not have design or holes that could rub against your skin.
3. Every day you must inspect your shoes before wearing them to make sure there are not any other objects inside them that could hurt your feet.
4. If you observe an injury do not try to take care of it on your own. Seek your doctor’s assistance. Remember that it is not just a simple wound and it therefore requires special care and attention [101].
Patient Foot Care Education
Patient education should be an integral part of management and prevention. Treatment outcomes will be directly influenced by patients’ knowledge of their own medical status, their ability to care for their wound and concordance with their treatment [95, 96]. Patients with diabetes and high-risk foot conditions should be educated regarding their risk factors and appropriate management. A non-judgmental assessment of a person’s current knowledge and care practices should be obtained first.
Patients at risk should understand the implications of the loss of protective sensation, the importance of foot monitoring on a daily basis, the proper care of the foot, including nail and skin care, and the selection of appropriate footwear. The patient’s understanding of these issues and their physical ability to conduct proper foot surveillance and care should be assessed. Patients with neuropathy should be advised to break in new shoes gradually to minimize the formation of blisters and ulcers. Patients with visual difficulties, physical constraints preventing movement, or cognitive problems that impair their ability to assess the condition of the foot and to institute appropriate responses will need other people, such as family members, to assist in their care. Patients at low risk may benefit from education on foot care and footwear.
The development of an ulcer is a major event and a sign of progressive disease. It is important to discuss the impact of the ulcer on life expectancy with the patient. Education should be offered on ways in which patients can help to improve outcomes by making lifestyle changes (eg smoking cessation) and working with practitioners to reduce the risk of recurrence and lifethreatening complications [95].
A Cochrane systematic review found that educating people with diabetes about the need to look after their feet improves their foot care knowledge and behaviour in the short term. There was insufficient evidence that education alone, without any additional preventive measures, effectively reduces the occurrence of ulcers and amputations [97].
Patient education should be a planned life-long process, starting from the point of diagnosis and remaining as an essential component of diabetes care.
For both Type 1 and Type 2 diabetes the aim of patient education should be to optimise:
1. Knowledge of diabetes and the aims of its management and the prevention of complications [91].
2. Motivation and attitudes to self-care - potential barriers to selfcare need to be assessed and addressed.
3. Ability to define and agree personal health-care targets and develop strategies for meeting them.
4. Behaviours which interact with diabetes management.
5. Empowerment in self management and communicating with the professional members of the healthcare team effectively.
Whilst medical treatments are important, long-term outcomes are also influenced by choices that people with diabetes make about diet, physical activity and other health-related behaviours. These choices will in part reflect knowledge about their condition and their ability to monitor it [98].
It is therefore necessary for patient education to incorporate both:
• Information giving/awareness raising, mainly to enable initial management of diabetes, but should also be on-going to meet the variable needs of the individual and match life events.
• Supporting behaviour change and self-care skills to ensure better outcomes in the long-term.
Maintaining behaviour change is essential in achieving positive longer-term benefit [105-107] and this is a challenging area which requires the use of appropriate skills, such as adult learning skills and a range of psychosocial methods. Interventions using enhanced methods including visual aids, behavioural learning and patient-centred techniques (eg patient participation) produce larger effects than those using didactic methods [107]. Acknowledging people’s feelings and concerns and helping them to set achievable goals are achieved by using a patient-centred approach and motivating behavioural change.
Facilitating self-management involves helping individuals to find their own best combination of behaviours. It is suggested that educator skills and training should include motivation methods, psychology, peer review and working with groups [98].
Patients and healthcare professionals need to have access to adequate information resources that are:
1. Accurate and consistent.
2. Timely.
3. In the appropriate format.
a. Diversity in preferences for information presentation needs to be recognised.
b. The education material has to be available in the appropriate language and needs to be acceptable in cultural terms.
c. Information should be in a suitable format to meet any cognitive or physical impairment needs.
It would be ideal if an individualised plan can be prepared and filled in by both patient and ‘educator’ at different stages and it can be kept with the person’s diabetes health-care record file for personal care plans to help empower people with diabetes and patient held/accessed records to facilitate self-care.
eg: take-home material, brief follow-up calls, support groups or regular follow-up visits, will be critical to maintaining the success of any educational intervention. Obviously this will depend on adequate staffing and sufficient time assigned for education services.
Patient counseling refers to the process of providing information, advice and assistance to help patients use their medications appropriately.
Patient counselling is the part of educating the patient towards diseases and proper use of medication. In this part is also counsel awareness to diseases and preventive measures.
Counselling instructions for diabetes patients: At and shortly after diagnosis, basic facts are necessary for the initial management of diabetes and patient education should provide the minimum instruction to obtain control over the new situation and basic supportive information on:
1. The nature, symptoms and outcomes of diabetes and risks associated with the condition [91].
2. Identifying and addressing fears, anxieties and preconceived ideas of diabetes and answering questions [91].
3. Healthy eating.
4. Physical activity.
5. Initiating treatment whether tablets or insulin - with insulin, guidance with self-injecting.
6. Awareness of acute complications such as hypoglycaemia and to deal with them.
7. Self-monitoring.
8. Confidence building for self-management [91].
In the months following diagnosis, continuing education will expand on these topics covered initially and in addition will cover elements essential to living with diabetes such as:
1. Ensuring optimal and appropriate use of therapy, whether tablets or insulin.
2. Managing effectively nutrition and physical activity.
3. Being able to detect and manage acute complications of therapy such as hypoglycaemia.
4. Being aware of late complications preventing, detecting and
treating them, and of the need for regular assessment.
5. Being able to monitor, record and act appropriately on the
results of therapy.
6. Making appropriate responses to unpredicted and new problems.
7. Dealing with special situations, eg. travelling, illness.
8. Making appropriate lifestyle changes (eg. smoking, alcohol, drugs) and dealing adequately with stress.
9. Dealing with psychological aspects of living with diabetes.
10. Being aware of pre-conception care and implications of pregnancy.
11. Accessing healthcare professionals when needed.
Family members, partners and care takers should be included in the education process as appropriate. The nature and level of information, as well as the timing of when provided, will ultimately be determined by the assessed needs of the individual and the format of the educational intervention [92-94].
1. Importance of diet in diabetes management and cardiovascular risk factor reduction, and role for achieving optimum metabolic control.
2. Recommendations for a healthy diet: guidance on recommended daily intakes of carbohydrate, fats, protein, fibre, nutritional labels etc.
3. Dietary assessment and addressing specific dietary needs.
4. Consideration and discussion of cultural/religious needs.
5. Discussion of dietary changes/ meal planning/cooking and recipe modification.
6. Benefits and strategies for weight management if appropriate.
7. Alcohol: drinking guidelines, risk of hypoglycaemia etc.
1. Importance of physical activity in control of blood glucose and blood pressure, improving insulin sensitivity and general health.
2. Appropriate types of activity and personal goals.
3. Sport and leisure: safety and regulations, precautions, adjusting food and insulin, preventing and treating hypos, more frequent monitoring.
Literature Survey
1. Bijoy cv, et al., [102] 2012. Conducted a study on “knowledge assessment and patient counseling on diabetic foot care”. The study concludes that the well structured foot care education by a clinical pharmacist have a significant impact in the prevention of recurrent foot infections and complications which may lead to amputation due to the lack of diabetic foot care knowledge.
2. Murtaza Gondal, et al., [103] 2007. Conducted a study on “evaluation of knowledge and practices of foot care in patients with chronic type 2 diabetes mellitus”. The results of this study demonstrate patients with diabetes who are at risk for the development of diabetic foot ulcers should receive ongoing footspecific patient education.
3. Hanu George, et al., [79] 2013. Conducted a study on “foot care knowledge and practices and the prevalence of peripheral neuropathy among people with diabetes attending a secondary care rural hospital in southern india” The study concludes that knowledge and practices regarding foot care. Male gender, low education, and lesser duration of diabetes are associated with poor knowledge scores. The prevalence of diabetic peripheral neuropathy is high.
4. Nima Madanchi, et al., [104] 2013. Conducted a study on “Who are diabetic foot patients? A descriptive study on 873 patients” The study concludes that Number of patients with DFU is increasing. Recurrence of DFU is a major point of concern which underscores the importance of patient education to prevent secondary ulcers. As a result, educating medical and nursing personnel, applying screening and prevention guidelines, and allocating more resources are of great importance regarding treatment of DFU patients.
5. Beverley Meaney, [105] 2012. Demonstrated a study on “DIABETIC FOOT CARE: PREVENTION IS BETTER THAN CURE” the study concludes that patient’s understanding, knowledge and awareness in relation to these problems which needs attention. Constant surveillance of their own feet is necessary for patients to help avoid complications and early detection of any problems will help maintain their independence and health.
6. Maria I Anselmo, et al., [106] 2010. Conducted a study on “The effectiveness of educational practice in diabetic foot: a view from Brazil” The study concludes that the planned and multidisciplinary educational approach enabled high compliance of the ulcer prevention care needed in diabetic patients at risk for complications. the use of footwear provided was extremely low, demonstrating that the issue of its acceptability should be further and carefully addressed.
7. Syed Fahd Shah, et al., [107] 2011. Conducted a study on “Evaluation and Management of Diabetic Foot: A Multicenter study conducted at Rawalpindi, Islamabad” The study concludes that Effective glycemic control, timely hospital admissions, appropriate surgical/medical treatment along with patient education in foot care, can decrease morbidity and mortality due to diabetic foot disease.
8. Konstantikaki V. RN, MSc, PhD, [108] 2008. Demonstrated a study on “The role of primary care in the prevention of diabetic foot amputations” the study concludes that the prevention of ulcers through the implementation of health education programs on the population and through training programs for the health professionals. It is estimated that 85% of low amputations of the diabetic foot could be prevented with the growth of the development health education programs.
9. O.O. DESALU, et al., [109] 2011. Conducted a study on “diabetic foot care: self reported knowledge and practice among patients attending three tertiary hospital in nigeria” the study concludes that study has highlighted the gaps in the knowledge and practice of foot care in DM patients and underscores the need for an educational programme to reduce of diabetic foot complication.
10. Nadia Saeed, [110] 2010. Demonstrated a study on “Frequency of patients with diabetes taking proper foot care according to international guidelines and its impact on their foot health” this study concluded that This study demonstrated that very few patients with diabetes were practicing proper foot care according to the ADA Guidelines. High risk behaviours were common which could lead to preventable foot complications.
11. Wipa Sae-Sia, et al., [111] 2013. Conducted A study on “effect of a self-management support program on diabetic foot care behaviors” The result indicates that a five-week SM program effectively enhanced DFCB. Thus, nurses are recommended to apply this program in improving DFCB in order to prevent diabetic foot ulcers or other foot complications.
12. Nikhil P. Hawal, et al., [112] 2012. Conducted a study on “Knowledge, attitude and behaviour regarding self-care practices among type 2 diabetes mellitus patients residing in an urban area of South India” this Results revealed good attitude but poor knowledge and practices (behaviour) towards diabetes. We concluded that there is a need for structured programmes to improve attitude and practices of diabetic patients to promote better compliance towards diet, exercise and drug regimen.
13. Thomas C, et al., [113] 2008. A study was to assess the “knowledge and practices among the diabetic patients regarding foot care”. This study conclude that About one third of diabetic patients had poor knowledge about foot care and only very few patients had good practices for foot care.
14. Shaibi GQ, et al., [114] 2008. A study was done to assess the disease “knowledge in patients attending a diabetic foot clinic”. This simple quality initiative reinforces the nation that patients with diabetes who are at risk for the development of diabetic foot ulcers should receive ongoing foot-specific patient education.
15. Ray JG, et al., [115] 2008. A study was done to determine knowledge and practice of foot care in people with diabetes. The results highlight areas where efforts to improve knowledge and practice may contribute to the prevention of foot ulcers and amputation.
16. Maty SC, et al., [116] 2008. The study was to “evaluate an intensive diabetes foot care education program at high risk for foot ulcer”. This study conclude that the patients also reported improved satisfaction with foot care; Intensive education program improved the foot care knowledge and behavior of high-risk patients.
17. T. Haas, et al., [117] 1994. The study was conducted to “assess the knowledge and practices regarding foot care”. Only one-third of the patients had received diabetic education. The best results were obtained in educated and younger patients. Our findings demonstrate that elderly diabetics can benefit from an education program and prove a real insufficiency in current education of elderly diabetics.
18. Sayeed MA, et al., [118] 2007. The study was conducted to “assessed the knowledge of the diabetic patient on foot care research”. This study conclude that could be taken is that the clients knew about the care that they must have with their feet to don't have complications, but the "own care" is not well done.
19. Um HD, et al., [119] 2008. A study was conducted to “assess the effectiveness of patient education on the prevention of foot ulcers in patients with diabetes mellitus”. this study conclude that Weak evidence suggests that patient education may reduce foot ulceration and amputations, especially in high-risk patients.
20. Puepet FH, et al., [120] 2008. A study on “Identification of risk factors for the development of type 2 diabetes mellitus is a necessary step in planning prevention programmes for diabetes mellitus”. This study conclude that Inactivity alcohol usage and excess weight appear to be dominant risk factors for development of type 2 DM in this group.
21. Weiss R, et al., [121] 2008. This descriptive study was conducted in an Arab-Muslim town to assess the level of “knowledge, beliefs, and concerns about diabetes care”. This study conclude that there is a need for interventions focused on overcoming these barriers to improve diabetes treatment and self-care in this population.
22. Wang J, et al., [122] 2008. A study was conducted at a Veterans Administration Hospital to “evaluate patient capability for self-management” found that over 35 per cent of the patients interviewed lacked any formal training. The results indicate the need for systematic analysis of patient knowledge and the evaluation of training programs.
23. Qi L, et al., [123] 2008. The study was developed to explore the “psychological and behavioral factors that may influence both the incidence of chronic wounds and their progression”. This study conclude that patients may find it difficult understanding the rationale underlying prevention and treatment of foot ulcers; ulcerated patients may find it difficult to engage in the management of their foot ulcer outside consultations.
24. Parichehr Kafaie, et al., [124] 2012. A study conducted on ”Evaluation of Patients' Education on Foot Self-Care Status in Diabetic Patients” this study conclude that foot self-care education could improve knowledge and performance of patients about various foot problems, and was significantly important in preventing ulcers.
25. M. Riaz, et al., [125] 2013. A study conducted on “Health related quality of life in patients with diabetes using SF-12 questionnaire” this study conclude that diabetes is associated with decreased levels of both physical and emotional wellbeing. The deterioration in quality of life was more evident in the physical than in the emotional wellbeing. Diabetes education results in improved quality of life.
It is a prospective cohort study and the study would be conducted over a period of 6 Months.
Diabetic patients attending Medical Outpatient and inpatient Departments in Rajiv Gandhi institute of medical sciences (RIMS) Government Hospital, Kadapa.
Diabetic patients who fulfill the inclusive criteria will be considered as the sample and the sample size is 150-200.
The study includes,
Male and female patients who were diagnosed with type I and type II diabetes mellitus aged between 31 to 75 years.
Diabetic patients able to understand Telugu or English.
Diabetic patients who are willing to participate.
The study excludes,
Diabetic patients who are not willing to participate.
Patient with cognitive impairment, visual or hearing loss.
Pregnancy, planned pregnancy, or lactation.
Patients will be selected from department of general medicine wards (I.P/O.P). The required baseline will be collected from diabetes I.P/O.P in the patients or their relatives. Data collection proforma by chart review method with a well-suited to assess the results. Selection of patients will be identified by seeing their diagnosis which is conformed by the physician.
Informed consent is obtained from the each patient before participating the study (ANNEXUE-4). Data collection from the patients will include 4 parts.
In this part we are taking the information about case history from the patient or from their case sheet. This will includes the Demographic data, If he/she is a known case of diabetes and duration of diabetes, habits (Smoker/Alcoholic/ food habits/physical activity), family history, and the treatment. (ANNEXURE-1)
In this part we are going to list out the responses of patients to our questionary form about the knowledge of patient towards the disease and drugs.
It contains the questions up to 20 and give them score and divided in to poor, fair and good categories based on their scores. (ANNEXURE-2)
Here we are going to know the knowledge about patient’s disease through obtaining the questionnaire responses.
The questionary forms are prepared based on the patients mentality, attitudes, locality and that would be prepared by the researchers. The questionnaire had questions which were of the close ended type and comprised of yes/no/don’t know variety of answers. The structured questionnaires were administered to the parents who completed them on the spot. Those who could not read and write were assisted by the researchers.
After completing the information we will give the standard patient counseling regarding disease condition, complications, smoking, foot wear, nail care, foot care, food habits and exercises were given to the selected patient with poor and satisfactory knowledge and this is very useful to patients and practitioners for better patient care. Patient information leaflets about patient counseling brochures are distributed to the patient for better understand and further beneficials (ANNEXURE-3).
1. Graph Pad Prism 5.04 software. Simple frequency distribution has to be generated for dependent and independent variables.
2. Chi-square test was applied to find out statistical significance of socio-economic factors on knowledge regarding foot care in diabetic patients.
Experimental Results
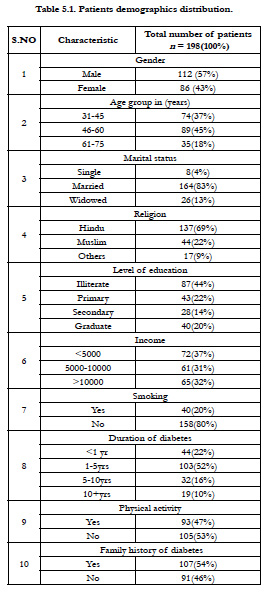
A total of 198 diabetic patients were included in our study during a period of six months. The demographic detail among the subjects reveals that 112(57%) were males while 86(43%) were females.
Among the subjects 72(37%) had an income of <5000, 61(31%) had 5000-10000 per month and 65(32%) had their income more than 10000 per month. Based on the literacy status 87(44%) of subjects were illiterates, 43(22%) were primary education level and 28(14%) were secondary education level and 40(20%) were graduation level. Patients were asked about their smoking habits 158(80%) were non-smokers and 40(20%) were smokers. Patients’ demographic details are shown in Table 5.1.
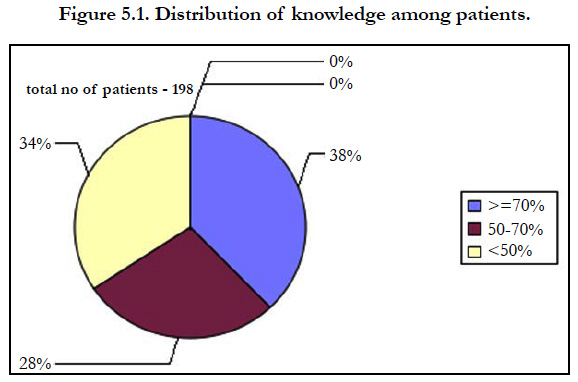
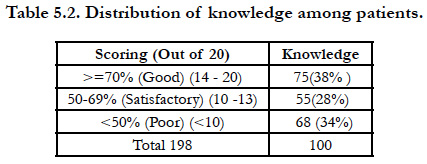
Among the patients 75(38%) had good knowledge, 55(28%) had satisfactory and 68(34%) had poor knowledge regarding diabetic foot care (Table 5.2).
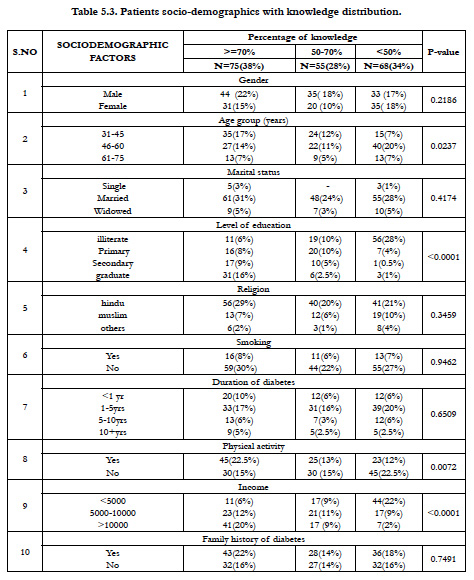
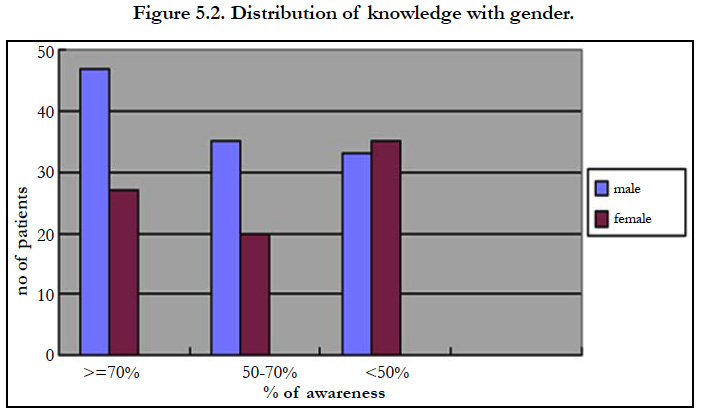
The association between demographic variables and foot care knowledge was found out by using chi-square test. In association with sex and knowledge, 44(22%) male patients had good, 35(18%) had satisfactory and 33(17%) had poor knowledge. In females 31(15%) had good, 20(10%) had satisfactory and 35(18%) had poor knowledge. The chi- square value obtained was 3.014. Sex was not significantly associated in relation to knowledge (p=0.2186) regarding foot care.
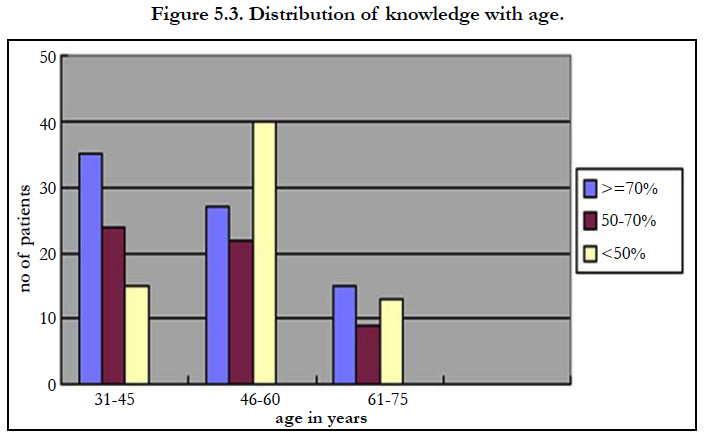
Subjects under the age group 31-45 years, 35(17%) had good, 24(12%) had satisfactory and 15(7%) had poor knowledge. The age group of 46-60 years shows that 27(14%) had good, 22 (11%) had satisfactory and 40(20%) had poor knowledge. Under the age group 61-75 years, 13(7%) of them had good, 9(5%) had satisfactory and 13 (7%) had poor knowledge. The chi-square value obtained was 3.199 (p=0.0237) which has statistically no association with knowledge regarding foot care.
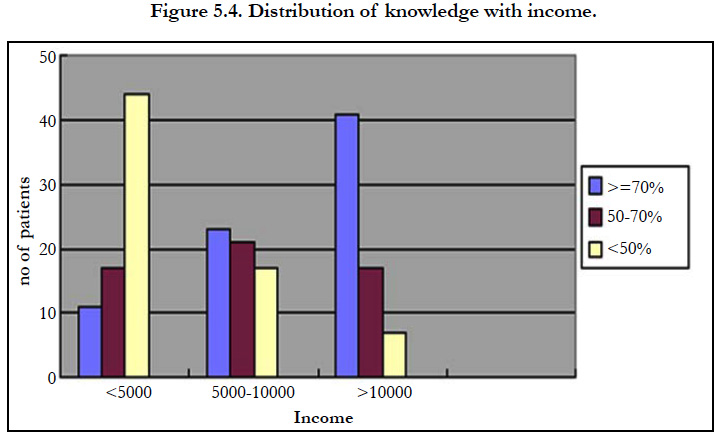
Regarding income and knowledge on those subjects with a monthly income of <5000, 11(6%) had good, 17(9%) had satisfactory and 44(22%) had poor knowledge. Those with monthly income 5000- 10000, 23(12%) of them had good, 21(11%) had satisfactory and 17(9 %) had poor knowledge. On patients with income >10000, 41(20%) of them had good, 17(9%) had satisfactory and 7(2%) had poor knowledge. The chi-square value obtained was 49.55 (p<0.0001) which is highly significant. Income per month has shown statistical association with the knowledge regarding foot care.
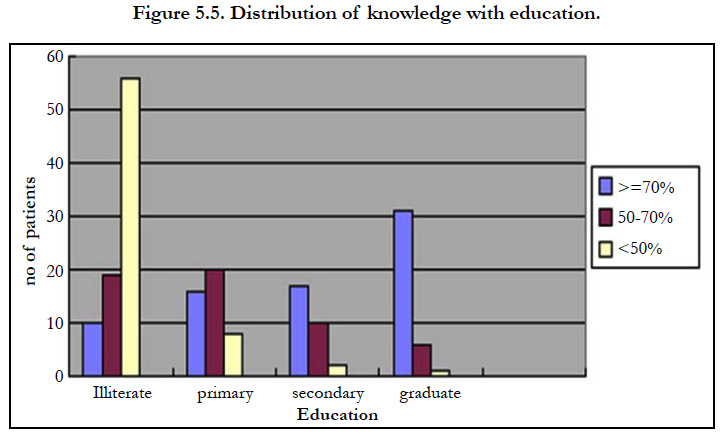
Among the subjects who are illiterates, 11(6%) had good, 19(10%) had satisfactory and 56(28%) had poor knowledge. In primary education level subjects 16(8%) had good knowledge, 20(10%) had satisfactory and 7(4%) had poor knowledge. In secondary level subjects 17(9%) had good knowledge, 10(5%) had satisfactory and 1(0.5%) had poor knowledge. It was found that 31(16%) of graduation level subjects had good, 6(2.5%) had satisfactory and 3(1%) had poor knowledge. It shows a chi-square value of 91.05., the role of education has shown an impact on the knowledge (p<0.0001) regarding foot care.
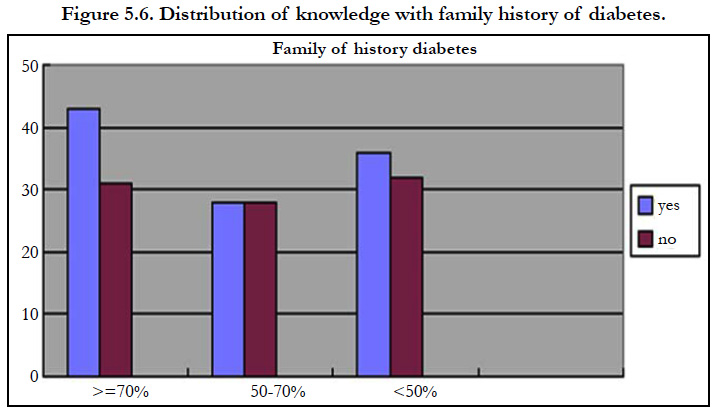
Subjects with a family history of foot diabetes 43(22%) had good knowledge, 28(14%) had satisfactory knowledge and 36(18%) had poor knowledge. In subjects without family history of diabetes 32(22%) had good knowledge, 28(14%) had satisfactory knowledge and 32(16%) had poor knowledge. History of foot infection has shown statistically no association with the knowledge (p= 0.646) regarding foot care.
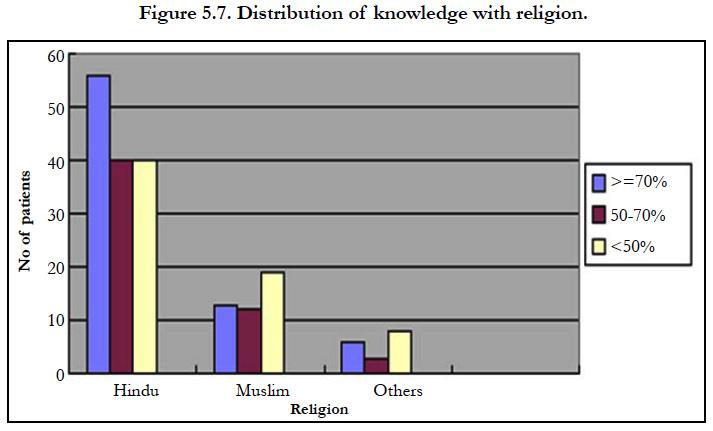
patients had good, 40(20%) had satisfactory and 4(2%) had poor knowledge. In muslims 13(7%) had good, 12(6%) had satisfactory and 19(10%) had poor knowledge. In others 6(2%) had good, 3(1%) had satisfactory and 8(4%) had poor knowledge. The chisquare value obtained was 4.472. Religion was not significantly associated in relation to knowledge (p=) regarding foot care.
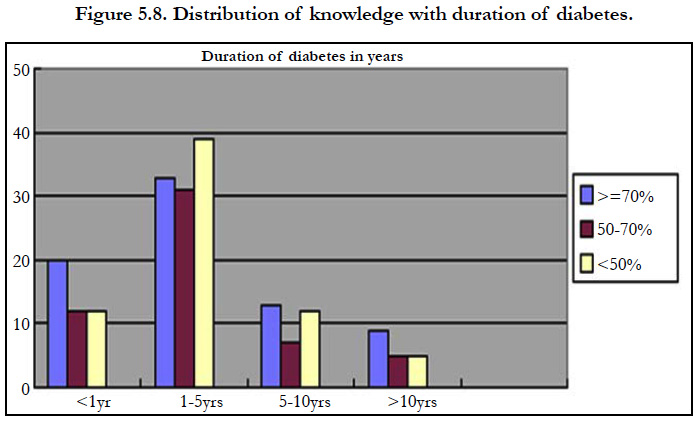
Subjects with duration of diabetes 20(10%) had good knowledge in <1year and 12(6%) had satisfactory knowledge and 12(6%) had poor knowledge. In subjects with 1-5 years diabetes 33(17%) had good knowledge, 31(16%) had satisfactory knowledge and 39(20%) had poor knowledge. In subjects with 5-10 years diabetes 13(6%) had good, 7(3%) had satisfactory and 12(6%) had poor knowledge. In subjects with more than 10 years diabetes 9(5%) had good, 5(2.5%) had satisfactory and 5(2.5%) had poor knowledge. History of duration of diabetes has shown statistically no association with the knowledge (p= 0.6509.) regarding foot care.
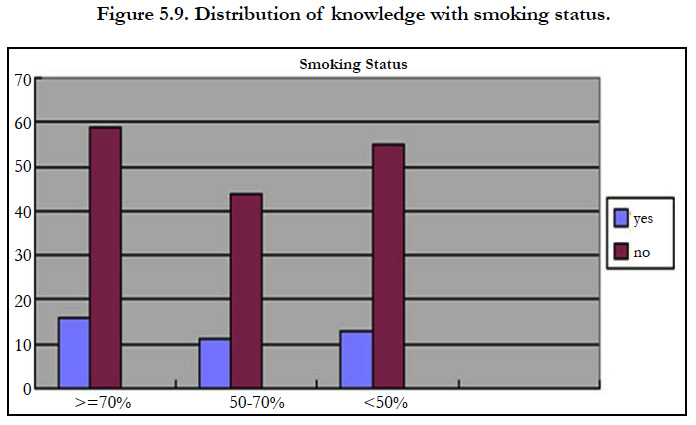
Subjects with a smoking history 16(8%) had good knowledge, 11(6%) had satisfactory knowledge and 13(7%) had poor knowledge. In subjects without smoking history 59(8%) had good knowledge, 44(22%) had satisfactory knowledge and 55(27%) had poor knowledge. History of smoking has shown statistically no association with the knowledge (p= 0.646) regarding foot care.
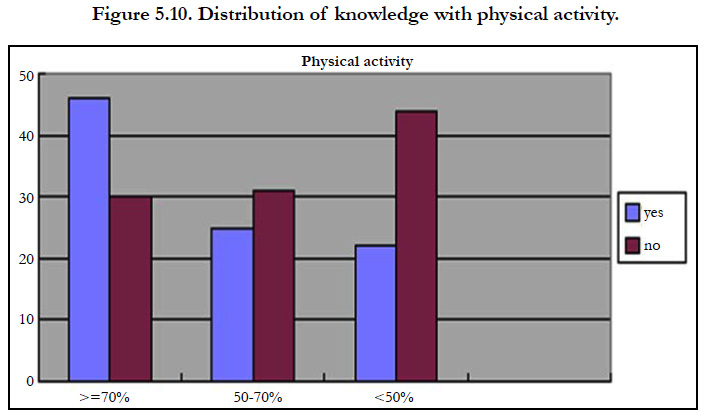
Subjects with a history of physical activity 45(25%) had good knowledge, 25(13%) had satisfactory knowledge and 23(12%) had poor knowledge. In subjects without physical activity 30(15%) had good knowledge, 30(15%) had satisfactory knowledge and 45(22.5%) had poor knowledge. History of physical activity has shown statistically association with the knowledge (p=0.646) regarding foot care.
We are given counseling to the poor and satisfactory patients about diabetic foot care according to who guidelines.
Discussion Of Results
Diabetic foot care is essential for preventing complications of diabetic neuropathy and vascular insufficiency. A substantial proportion of diabetic patients are not offered adequate foot care, even in the presence of major risk factors for lower limb complications. In our study we found that patient knowledge and practices are strongly related to literacy status, income and foot care education.
In this study sex has no relationship regarding knowledge on foot care, the results in the above referred study conducted by Seema Hasnain et al., are consistent with our study. Low scores of foot care were common in males than in females. However this can be explained on the basis that in this study there were more males than females [123].
Out of 198 patients majority were males and belong to the age group between 40-60 years. This shows that diabetic foot problem is mainly concentrated on elderly which increases the morbidity in them due to diabetes.
In a study conducted by C. H. Ding et al., to assess the knowledge of diabetic and non diabetic patients in Klinik Kesihatan Seremban found that higher education and higher income were associated with higher knowledge score [124]. In this study also the income level which is mostly influenced by occupation has shown a positive relationship with foot care knowledge.
A study conducted by Seema Hasnain et al., to assess the knowledge and practices of the diabetic patients on foot care. It concluded that literacy has significant association with the knowledge related to foot care.
Regarding knowledge, only 29% respondents had good information (>70%) about foot care and formal education had a role in better knowledge about foot care [123]. In this study, there were 34 (46.5%) respondents who were illiterate and their score was <50% and 21(31.5%) respondents whose educational qualifications were matric and above matric, their score regarding knowledge was more than >70%. almost same we found in our tudy.
A study by Fabio Batista et al., suggests by their study that a few diabetic patients were appear to be adequately educated on potential morbidity of diabetic foot ulcers or preventive measures to avoid foot specific morbidity [125]. The data's obtained from their study supports that coordinated program combining preventive foot specific patient education, skin and nail care and foot wear decrease the diabetic foot disease. The present study also reveals that patient education regarding these aspects of foot care in poor knowledge was improved. Thus the foot care education has shown an impact on knowledge regarding foot care.
Patients with diabetes who are at risk for the development of diabetic foot ulcers should receive ongoing foot-specific patient education. This information needs to be constantly reinforced, as retention drops with time. Preventive practices must be stressed and reinforced so those without foot ulcers should not develop ulcers. A diabetic educator should be present in each diabetes outpatient clinic and in medical indoor departments.
By our study we can say that to provide a better foot care to the diabetic patient a clinical pharmacist can play pioneer role which is much more important in today's health scenario in India where due to overload of patients in hospitals or clinics a physician is not able to provide these vital information due to his/her busy schedule.
Summary
Our study shows that among the patients 75(38%) had good knowledge, 55(28%) had satisfactory and 68(34%) had poor knowledge regarding diabetic foot care.
The awareness and attitude regarding the diabetic foot care is poor among diabetic patients with low income and illiterates. This may cause lower extremity complications and recurrent foot infections, if left untreated which ultimately lead to amputation. From the study it is identified that the well structured patient counseling by a clinical pharmacist regarding diabetic foot care can be beneficial in the improvement of their knowledge.
Research Outcome
1. From this study we can say that to provide a better foot care to the diabetic patient a clinical pharmacist can play pioneer role which is much more important in today's health scenario in India where due to overload of patients in hospitals or clinics a physician is not able to provide these vital information due to his/ her busy schedule.
2. This study provides Counselling to the poor and satisfactory knowledge patients about diabetic foot care according to WHO guidelines.
References
- Peyrin-Biroulet L. Homocysteinemia, a new marker of severity in IBD ?. J Gastrointest Oncol. 2007 Mar 1;14(2):149-56.
- Quillard M, Berthe MC, Sauger F, Lavoinne A. Plasma determination of homocysteine on CPC Immulite 2000: comparison with determination on IMX Abbott. Ann Biol Clin (Paris). 2003 Nov-Dec;61(6):699-704. PubMed PMID: 14711612.
- Demets JP. A study by Harvard University researchers showed that too much homocysteine in the blood has a risk factor that can lead to cardiovascular disorders. But what is homocysteine? [Internet]. 2017 [cited 2017 Apr 17]. Available from: http://www.masantenaturelle.com
- Grunitzky K, Balogou K, Bark-kombate R, Kombate D, Amouzou K. Homocysteinemia and ischemic strokes at the CHU Campus of Lomé. Afr. J Neurol Sci. 2008;27(2).
- Vangelder E, Delecourt F, Cardozo MB, Dhondt JL, Forzy G. Hyperhomocysteinemia and Type 2 Diabetes. Ann Clin Microbiol Antimicrob. 2006 Sep 1;64(5):485-489.
- Guldener CV, Stehouwer CD. Homocysteine and vascular complications of diabetes. Diabetes Voice. 2003;48:31-33.
- Momin M, Jia J, Fan F, Li J, et al. Relationship between plasma homocysteine level and lipid profiles in a community-based Chinese population. Lipids Health Dis. 2017 Mar 14;16(1):54. PubMed PMID: 28288621.
- Yapo AE, Assayi M, et al. The reference values of 21 biochemical blood constituents of adult Ivorian presumed healthy. Afr Med Pub. 1990;(110):49- 57.
- Faeh D, Chiolero A, Paccaud F. Homocysteine as a risk factor for cardiovascular disease: should we (still) worry about it?. Swiss Med Wkly. 2006 Dec 2;136(47-48):745-56. PubMed PMID: 17225194.
- Labrousse C. Statistics: corrected exercises with course reminders. Dunod; 1978.
- Demuth K. Homocysteine and cardiovascular prevention in the elderly. Ann Biol Clin (Paris). 2001 Jul 24;59(4):465-8.
- Hultberg B, Agardh CD, Agardh E, Lövestam-adrian M. Poor metabolic control, early age at onset, and marginal folate deficiency are associated with increasing levels of plasma homocysteine in insulin-dependent diabetes mellitus. A five-year follow-up study. Scand J Clin Lab Invest. 1997 Jan 1;57(7):595-600.
- Drzewoski J, Czupryniak L, Chwatko G, Bald E. Hyperhomocysteinemia in poorly controlled type 2 diabetes patients. Diabetes Nutr Metab. 2000 Dec;13(6):319-24. PubMed PMID: 11232756.
- Hoogeveen EK, Kostense PJ, Beks PJ, Mackaay AJ, Jakobs C, Bouter LM, Heine RJ, Stehouwer CD. Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non–insulin-dependent diabetes mellitus: a population-based study. Arterioscler Thromb Vasc Biol. 1998 Jan;18(1):133-8. PubMed PMID: 9445267.
- Laraqui A, Bennouar N, Meggouh F, et al. Homocysteine, lipoprotein (a): risk factors for coronary heart disease. Ann Biol Clin (Paris). 2002 Sep- Oct;60(5):549-57. PubMed PMID: 12368140.
- Hegab Z, Gibbons S, Neyses L, Mamas MA. Role of advanced glycation end products in cardiovascular disease. World J Cardiol. 2012 Apr 26;4(4):90- 102. PubMed PMID: 22558488.
- Jarir J, Mohammadi H, Benazzouz B, Naamane A, et al. Study of Homocysteine and Lipid Metabolism in Moroccan Children with Type I Diabetes. Eur J Sci Res. 2012 Oct; 89 (4): 542-54.
- Qujeq D, Omran TS, Hosini L. Correlation between total homocysteine, low-density lipoprotein cholesterol and high-density lipoprotein cholesterol in the serum of patients with myocardial infarction. Clin Biochem. 2001 Mar;34(2):97-101. PubMed PMID: 11311217.
- Anan F, Masaki T, Umeno Y, Yonemochi H, Eshima N, et al. Correlations between homocysteine levels and atherosclerosis in Japanese type 2 diabetic patients. Metabolism. 2007 Oct;56(10):1390-5. PubMed PMID: 17884450.
- De Luis DA, Fernandez N, Arranz ML, Aller R, Izaola O, Romero E. Total homocysteine levels relation with chronic complications of diabetes, body composition, and other cardiovascular risk factors in a population of patients with diabetes mellitus type 2. J Diabetes Complications. 2005 Jan-Feb;19(1):42-6. PubMed PMID: 15642489.
- Yadav AS, Bhagwat VR, Rathod IM. Relationship of plasma homocysteine with lipid profile parameters in ischemic heart disease. Indian J Clin Biochem. 2006 Mar;21(1):106-10. PubMed PMID: 23105579.
- Thampi P, Stewart BW, Joseph L, Melnyk SB, Hennings LJ, Nagarajan S. Dietary homocysteine promotes atherosclerosis in apoE-deficient mice by inducing scavenger receptors expression. Atherosclerosis. 2008 Apr;197(2):620-9. PubMed PMID: 17950295.
- Zittoun J. Homocysteine and vascular pathology. Hematol. 1998 Jan 27; 4(1):7-16.
- Rais L, Wafi M, Lahbil D, Iraki M, et al., Ocular and systemic complications of homocystinuria: a report of five cases. J Fr Ophtalmol. 2003 Dec;26(10):1045-50. PubMed PMID: 14691398.
- Houston M. Homocysteine–a risk factor for vascular diseases: Guidelines for the clinical practice. J Am Nutra Assoc. 2004;7(1):11-21.
- Girs N, Giet D. Is the dosage of homocysteine relevant to the General Practitioner ?. Med J Lig. 2006;61(5-6):352-61.
- Booth GL, Wang EE. Preventive health care, 2000 update: screening and management of hyperhomocysteinemia for the prevention of coronary artery disease events. CMAJ. 2000 Jul 11;163(1):21-9. PubMed PMID: 10920726.
- Stanger O, Hermann W, Pietrzik K, Fowler B, Geisel J, Weger M. 2012. Consensus Article of DACH-Liga Homocysteine on the Rational Clinical Use of Homocysteine, Folic Acid and B vitamins in cardiovascular and thrombotic diseases. Guidelines and Recommendations [Internet]. 2017[cited 2017 Mar 20]. Available from: http://www.dach-liga-homocystein.org.
- Mishra PK, Tyagi N, Sen U, Joshua IG, Tyagi SC. Synergism in hyperhomocysteinemia and diabetes: role of PPAR gamma and tempol. Cardiovasc Diabetol. 2010 Sep 9;9:49. PubMed PMID: 20828387.
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972 Jun;18(6):499-502. PubMed PMID: 4337382.