Role Of Occlusal Adjustment As An Adjunct To Scaling And Root Planing In The Management Of Periodontitis
R. Saravanan, Sheeja Varghese, Arvina
1 Post Graduate Student, Department of Periodontics, Saveetha dental college and Hospital, Chennai-600077, Tamil Nadu, India.
2 Dean and Faculty of Department, Department of Periodontics, Saveetha dental college and Hospital, Chennai-600077, Tamil Nadu, India.
3 Senior Professor, Department of Periodontics, Saveetha Dental College and Hospital, Chennai-600077, India.
*Corresponding Author
Dr. Sheeja Varghese,
Faculty of Dentistry, Department of Oral Medicine and Radiology, Meenakshi Academy of Higher Education & Research; Meenakshi Ammal Dental College, Chennai, Tamil
Nadu, India.
Tel: 09940588033
E-mail: sangaviramesh12@gmail.com
Received: July 17, 2021; Accepted: November 10, 2021; Published: November 12, 2021
Citation: R. Saravanan, Sheeja Varghese, Arvina. Role Of Occlusal Adjustment As An Adjunct To Scaling And Root Planing In The Management Of Periodontitis. Int J Dentistry Oral Sci. 2021;8(11):4997-5000. doi: dx.doi.org/10.19070/2377-8075-210001008
Copyright: Dr. Sheeja Varghese©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The role of excessive occlusal forces in the progression of periodontal disease was explored for several years. If
occlusal trauma has any relationship to the progression of periodontitis, then its elimination should improve clinical outcomes
of periodontal disease. Occlusal adjustment is commonly recommended for patients with periodontitis and traumatic occlusion.
However, the scientific evidence linking occlusal adjustment to the improvement of periodontal parameters is limited.
Aim: This systematic review aims to analyse the available evidence for occlusal adjustment as an adjunct to conventional surgical
or non-surgical periodontal treatment in the management of periodontitis.
Materials And Methodology: A comprehensive search was done in electronic databases such as PubMed, Google Scholar,
Cochrane and hand search was made based on pre-determined eligibility criteria. Studies assessing the effectiveness of occlusal
adjustment as an adjunct to scaling and root planing in the management of periodontitis were selected after through screening.
Results: The selected 4 studies evaluated the influence of occlusal adjustment as an adjunct to periodontal therapy. All studies
assessed the clinical parameters including probing depth, clinical attachment level and tooth mobility. Out of 4 studies, 2
studies showed significant improvement in all clinical parameters among the group where occlusal adjustment was done along
with periodontal therapy. Whereas, 2 studies showed statistically insignificant differences between the groups with and without
occlusal adjustment along with periodontal therapy.
Conclusion: Available studies showed limited evidence to support the implementation of occlusal adjustment as an adjunct
to scaling and root planing in the management of periodontitis. However, the results are inconclusive because of the heterogeneity
of the studies.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Occlusion; Periodontitis; Occlusal Trauma; Occlusal Therapy.
Introduction
The role of occlusal trauma in the initiation and progression of
periodontitis remains a controversial subject in periodontology.
Occlusal trauma is defined as the injury of the attachment apparatus
of the periodontium resulting from functional or parafunctional
occlusal forces that exceed its adaptive capacity. It is characterized
by progressive tooth mobility, widening of periodontal
ligament space, thermal sensitivity, cemental tear, angular defects
in the bone, root resorption.[1]
Since occlusal trauma is a histologic event, it is debatable if occlusion
has any relationship with periodontitis. In the early 20th
century, investigators suggested that excessive occlusal force was
the cause of periodontitis and the forces need to be controlled
to treat periodontitis successfully.[3-6] In a study done using human
autopsy material, it was concluded that gingival inflammation
extending into the supporting bone was the cause for periodontal
destruction.[7] In a subsequent animal study, it was suggested that
the excessive occlusal forces caused alteration in the direction of
the periodontal ligament fibers and hence the gingival inflammation
entered directly into such areas.[8] Later, it was further proposed that inflammation begins in gingiva due to bacterial plaque
and progresses into the supporting periodontal tissues and hence
there is an alteration in the pathway of spread of inflammation
in teeth subjected to occlusal trauma. This combined effect of
occlusal trauma and bacterial plaque-induced inflammation was
termed ďco-destruction.Ē[9, 10].
In order to prove the relationship between traumatic occlusion
and periodontal disease, studies were performed on animal models
in the presence and absence of bacterial plaque. In the presence
of bacterial plaque and occlusal trauma, there was more
bone loss and progressive tooth mobility, but loss of connective
tissue attachment was the same as on teeth subjected to periodontitis
alone. When occlusal trauma was combined with periodontitis,
there was an accelerated loss of connective tissue attachment.
In contrast, when oral hygiene was maintained and inflammation
was controlled, occlusal trauma resulted in increased mobility and
loss of bone density without loss of connective tissue attachment,
during the length of the study. If the occlusal forces were
removed, the loss of bone density was reversible.[11-13] These
findings concluded that without inflammation, occlusal trauma
does not cause irreversible bone loss or loss of attachment. However,
none of the animal studies were able to reproduce all aspects
of human periodontitis. Also, these studies used excessive
occlusal forces and were conducted for a relatively short duration.
Therefore, these studies failed to prove the causal relationship between
occlusal trauma and the initiation of periodontal disease.
In parallel, researchers started to assess the effect of occlusal adjustments
on periodontal parameters in patients with periodontitis.
A series of studies tested the influence of occlusal adjustments
in association with periodontal therapy on attachment levels,
pocket depth, and tooth mobility. The findings from these studies
suggested that teeth that received occlusal reduction presented
better improvement in clinical attachment level. However, there
was no significant difference in reduction of tooth mobility and
probing depth between the groups with and without occlusal adjustment.[
14-16, 2] On the contrary, Vollmer et al.[17] suggested
no effect of occlusal adjustment on the degree of gingival inflammation.
Also, Hakkarainen et al.[18] studied the effect of occlusal
adjustment of teeth with deep periodontal pockets as an adjunct
to scaling to root planing and reported no additive effect of occlusal
adjustment in terms of mobility and probing pocket depth.
In summary, data obtained from the existing interventional studies
do not provide strong evidence to support occlusal therapy as
an adjunct to scaling and root planing. Nonetheless, occlusal adjustment
as a part of the periodontal treatment is recommended,
scientific support is still inconclusive. In this context, the objective
of this systematic review was to analyze the available evidence
for occlusal adjustment as an adjunct to conventional surgical or
non-surgical periodontal treatment in the management of periodontitis.
Materials And Methodology
A comprehensive search was done in electronic databases such as
PubMed, Google Scholar, Cochrane and hand search was made
and the article selection was carried out according to PRISMA
guidelines. Studies which assess the effectiveness of occlusal adjustment
as an adjunct to scaling and root planing in the management
of periodontitis were selected after through screening.
The search terms were identified based on the following PICO
format.
Population: Patient with chronic periodontitis
Intervention: Occlusal adjustment
Comparison: No occlusal adjustment but with conventional surgical
or non-surgical periodontal treatment alone.
Outcome: Tooth mobility, Probing pocket depth, Clinical attachment
level.
Inclusion Criteria
1. Randomised controlled clinical trials or clinical trials wherein
the effectiveness of occlusal adjustment in periodontitis patients
were evaluated with respect to clinical or radiographic parameters
2. Any cohort study which assessed the effectiveness of occlusal
adjustment in periodontitis patients were evaluated with respect
to clinical or radiographic parameters.
Exclusion Criteria
1. Animal studies
2. No statistical analysis of data
3. The study without a group with no occlusal adjustment done
4. The study without evaluation of clinical or radiographic parameters but only other parameters such as GCF flow
Results and Discussion
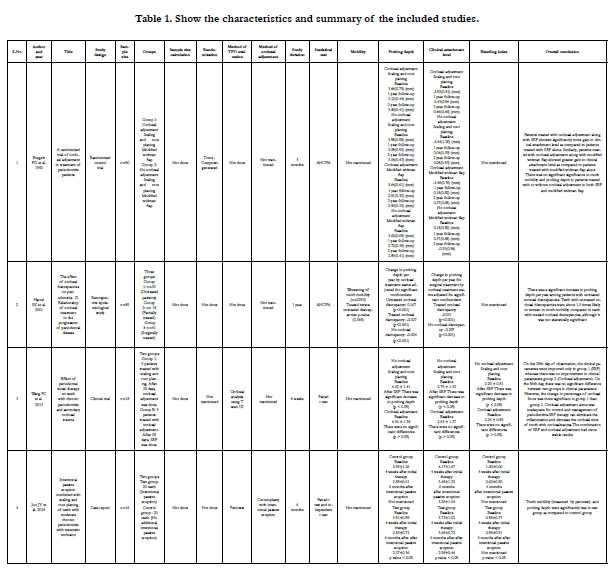
The selected 4 studies evaluated the influence of occlusal adjustment
as an adjunct to periodontal therapy. All studies assessed the
clinical parameters including probing depth, clinical attachment
level and tooth mobility. Out of 4 studies, 1 study showed significant
improvement in clinical attachment level among the group
where occlusal adjustment was done along with periodontal therapy
when compared with the group who had undergone periodontal
therapy alone without occlusal adjustment. But in the same
study there was no significant difference in tooth mobility and
probing depth in patients treated with or without occlusal adjustment.[
2] Whereas, 2 studies showed significant reduction in tooth
mobility and probing depth in patients treated with occlusal adjustment.
Teeth with untreated occlusal discrepancies were about
1.3 times likely to worsen in tooth mobility compared to untreated
teeth with occlusal discrepancies.[19, 20] Another study showed
statistically insignificant differences between the groups with and
without occlusal adjustment along with periodontal therapy.[21]
The role of trauma from occlusion in the etiology of periodontal
disease has been discussed since the early 90s. The literature
evidence supports that trauma from occlusion causes disorganisation
of periodontal tissues, impairing their normal repair function.[
22, 23] Also, the occlusion trauma acts as a co-destructive
zone, influencing the spread of inflammation directly to the periodontal
ligament, eliciting a combined lesion of trauma from occlusion
and periodontitis.[24, 25] Conversely, few studies showed
no causative association between trauma from occlusion and periodontal
disease, indicating little to no correlation between trauma
from occlusion and periodontitis.[26-28] Despite extensive research
over many decades, the role of occlusion in the etiology
and pathogenesis of periodontal disease is still not completely
understood. Thus, we carried out this systematic review with the contemporary methodological principles to reflect the highest
available evidence.
A systematic review involves the application of methodological
strategies that limit bias and evaluate and summarize crucial scientific
evidence. These systematic analyses can help practitioners
be aware of the scientific literature. The search strategy results in
4 studies, all studies assessed the role of traumatic occlusion and
occlusal adjustment in the treatment of periodontitis.
Burgett FG et al conducted a randomized control trial to evaluate
the influence of occlusal adjustment as an adjunct to non-surgical
and surgical periodontal therapy. It was found out that the gain
in clinical attachment was significantly more in the group where
occlusal adjustment was done along with either non-surgical or
surgical periodontal therapy, whereas in terms of probing pocket
depth there was no significant improvement. Also, there was no
significant difference in reduction of tooth mobility between the
groups with and without occlusal adjustment. In addition, the
reduction in tooth mobility was similar with either surgical and
non-surgical periodontal therapy. Another finding of this study
was the initial tooth mobility and initial severity of periodontal
disease did not affect the clinical attachment response to occlusal
adjustment.[2]
Similarly, Harrel SK et al investigated the effect of treatment of
occlusal discrepancies on periodontitis through a retrospective
epidemiological study. In this study, when worsening in teeth mobility
was observed over time, it was found that teeth with no initial
occlusal discrepancies were significantly less likely to worsen
in mobility when compared to either treated or untreated occlusal
discrepancies. In addition, there was no statistical significant difference
between teeth with treated occlusal discrepancies and
teeth with untreated occlusal discrepancies in terms of worsening
in mobility over time. However, it was observed that the mean
increase in probing depth per year among teeth with untreated
occlusal discrepancies was statistically significant and greater than
either teeth with no occlusal discrepancies or those with treated
occlusal discrepancies.[19]
Wang PC et al investigated the effect of scaling and root planing
and occlusal adjustment in terms of probing depth, clinical attachment
loss, occlusal time, percentage of occlusal force on patients
with chronic periodontitis and secondary occlusal trauma. In this
study, at baseline, one group was treated by full-mouth scaling and
root planing and the other group was treated by occlusal adjustment
in occlusal trauma site and after 28 days, the treatment was
exchanged between both the groups. After scaling and root planing
alone, all the clinical parameters were significantly decreased
whereas, none of the parameters exhibited significance difference
after occlusal adjustment alone. After the treatments were
exchanged between both the groups, the reduction in parameters
was not statistically significant between two groups, however the
reduction of occlusal time and percentage of occlusal force were
more significant in patients who had undergone scaling and root
planing followed by occlusal adjustment than the patients who
had undergone occlusal adjustment followed by scaling and root
planing [21].
Joo JY et al evaluated the effectiveness of occlusal adjustment in
the form of intentional passive eruption using occlusal reduction
on patients with chronic periodontitis and traumatic occlusion. In
this study, teeth with intentional passive eruption were compared
to teeth with additional intentional passive eruption in terms of
probing depth, clinical attachment level, tooth mobility and marginal
bone loss. The teeth with additional intentional passive eruption
showed a significantly greater decrease in pocket depth, tooth
mobility and marginal bone loss when compared to the teeth with
intentional passive eruption. However, there was no significant
change in clinical attachment level in both the groups.[20]
Conclusions
Available human studies showed that there is limited evidence
that the combination of scaling and root planing and occlusal adjustment
may achieve more stable results in the management of
periodontal diseases. More randomized control studies with long
term follow-up are required to support the implementation of occlusal
adjustment as an adjunct to scaling and root planing in the
treatment of periodontitis.
Acknowledgement
The authors are thankful to the Director of academics, Chancellor
and Dean of Saveetha Dental College and Hospitals for providing
a platform to do research activities.
References
-
[1]. Stillman PR. What is traumatic occlusion and how can it be diagnosed and
corrected?. The Journal of the American Dental Association (1922). 1925
Nov 1;12(11):1330-8.
[2]. Burgett FG, Ramfjord SP, Nissle RR, Morrison EC, Charbeneau TD, Caffesse RG. A randomized trial of occlusal adjustment in the treatment of periodontitis patients. J Clin Periodontol. 1992 Jul;19(6):381-7. PubMed PMID: 1634627.
[3]. Reinhardt RA, Pao YC, Krejci RF. Periodontal ligament stresses in the initiation of occlusal traumatism. J Periodontal Res. 1984 May;19(3):238-46. PubMed PMID: 6235340.
[4]. Stones HH. An Experimental Investigation into the Association of Traumatic Occlusion with Parodontal Disease: (Section of Odontology). Proc R Soc Med. 1938 Mar;31(5):479-95. PubMed PMID: 19991440.
[5]. Comar MD, Kollar JA, Gargiulo AW. Local irritation and occlusal trauma as co-factors in the periodontal disease process. J Periodontol. 1969 Apr;40(4):193-200. PubMed PMID: 4977238.
[6]. Weinmann JP. Progress of gingival inflammation into the supporting structures of the teeth. The Journal of Periodontology. 1941 Jul;12(2):71-82. [7]. MACAPANPAN LC, WEINMANN JP. The influence of injury to the periodontal membrane on the spread of gingival inflammation. J Dent Res. 1954 Apr;33(2):263-72. PubMed PMID: 13152264.
[8]. Glickman I, Smulow JB. Further observations on the effects of trauma from occlusion in humans. J Periodontol. 1967 Jul-Aug;38(4):280-93. PubMed PMID: 5230022.
[9]. Glickman I. Inflammation and trauma from occlusion, co-destructive factors in chronic periodontal disease. The Journal of Periodontology. 1963 Jan;34(1):5-10.
[10]. GLICKMAN I, SMULOW JB. EFFECT OF EXCESSIVE OCCLUSAL FORCES UPON THE PATHWAY OF GINGIVAL INFLAMMATION IN HUMANS. J Periodontol. 1965 Mar-Apr;36:141-7. PubMed PMID: 14261862.
[11]. Polson AM. Trauma and progression of marginal periodontitis in squirrel monkeys. II. Co-destructive factors of periodontitis and mechanicallyproduced injury. J Periodontal Res. 1974;9(2):108-13. PubMed PMID: 4277746.
[12]. Lindhe J, Svanberg G. Influence of trauma from occlusion on progression of experimental periodontitis in the beagle dog. J Clin Periodontol. 1974;1(1):3-14. PubMed PMID: 4532114.
[13]. Polson AM, Zander HA. Effect of periodontal trauma upon intrabony pockets. J Periodontol. 1983 Oct;54(10):586-91. PubMed PMID: 6580411.
[14]. Ismail AI, Morrison EC, Burt BA, Caffesse RG, Kavanagh MT. Natural history of periodontal disease in adults: findings from the Tecumseh Periodontal Disease Study, 1959-87. J Dent Res. 1990 Feb;69(2):430-5. PubMed PMID: 2407756.
[15]. Wagner RL. Tooth Mobility, Probing Depth, and Gingivitis as Risk Factors for Response to Periodontal Treatment: A Dissertation Submitted in Partial Fulfillment. Master of Science in Periodontics. University of Michigan; 1992.
[16]. Wang HL, Burgett FG, Shyr Y, Ramfjord S. The influence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J Periodontol. 1994 Jan;65(1):25-9. PubMed PMID: 8133412.
[17]. Vollmer WH, Rateitschak KH. Influence of occlusal adjustment by grinding on gingivitis and mobility of traumatized teeth. J Clin Periodontol. 1975 Aug;2(3):113-25. PubMed PMID: 1058212.
[18]. Hakkarainen K, Uitto VJ, Ainamo J. Collagenase activity and protein content of sulcular fluid after scaling and occlusal adjustment of teeth with deep periodontal pockets. J Periodontal Res. 1988 May;23(3):204-10. PubMed PMID: 2841442.
[19]. Harrel SK, Nunn ME. The effect of occlusal discrepancies on periodontitis. II. Relationship of occlusal treatment to the progression of periodontal disease. J Periodontol. 2001 Apr;72(4):495-505. PubMed PMID: 11338302.
[20]. Joo JY, Kwon EY, Lee JY. Intentional passive eruption combined with scaling and root planing of teeth with moderate chronic periodontitis and traumatic occlusion. J Periodontal Implant Sci. 2014 Feb;44(1):20-4. PubMed PMID: 24616830.
[21]. Wang PC, Tang HR, Xu J, Zhang R, Liu LX, Wang QT. [Effect of periodontal initial therapy on teeth with chronic periodontitis and secondary occlusal trauma]. Zhonghua Kou Qiang Yi XueZaZhi. 2013 May;48(5):266-71. Chinese. PubMed PMID: 24004621.
[22]. Jin LJ, Cao CF. Clinical diagnosis of trauma from occlusion and its relation with severity of periodontitis. J ClinPeriodontol. 1992 Feb;19(2):92-7. Pub- Med PMID: 1602041.
[23]. Ericsson I, Lindhe J. Effect of longstanding jiggling on experimental marginal periodontitis in the beagle dog. J ClinPeriodontol. 1982 Nov;9(6):497- 503. PubMed PMID: 6960025.
[24]. Hakkarainen K. Relative influence of scaling and root planing and occlusal adjustment on sulcular fluid flow. J Periodontol. 1986 Nov;57(11):681-4. PubMed PMID: 3550034.
[25]. Harrel SK, Nunn ME. The association of occlusal contacts with the presence of increased periodontal probing depth. J ClinPeriodontol. 2009 Dec;36(12):1035-42. PubMed PMID: 19930093.
[26]. Wentz FM, Jarabak J, Orban B. Experimental occlusal trauma imitating cuspal interferences. The Journal of Periodontology. 1958 Apr;29(2):117-27. [27]. Yuodelis RA, Mann WV Jr. The prevalence and possible role of nonworking contacts in periodontal disease. Periodontics. 1965 Sep-Oct;3(5):219-23. PubMed PMID: 5212904.
[28]. Shefter GJ, McFall WT Jr. Occlusal relations and periodontal status in human adults. J Periodontol. 1984 Jun;55(6):368-74. PubMed PMID: 6588194.