Various Treatment Approaches for the Management Of Midline Diastema - A Retrospective Analysis
Gokul Gunasekaran1, Raghu Sandhya2*, Sri Rengalakshmi3
1 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
2 Reader, Department of Conservative Dentistry and Endodontics , Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
3 Senior Lecturer, Department of Orthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
*Corresponding Author
Raghu Sandhya,
Reader, Department of Conservative Dentistry and Endodontics , Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University,
Chennai, 600077, India.
Tel: 9884610410
E-mail: sandhya.sdc@saveetha.com
Received: September 06, 2020; Accepted: October 09, 2020; Published: October 27, 2020
Citation:Gokul Gunasekaran, Raghu Sandhya, Sri Rengalakshmi. Various Treatment Approaches for the Management Of Midline Diastema - A Retrospective Analysis. Int J Dentistry Oral Sci. 2020;7(10):942-945. doi: dx.doi.org/10.19070/2377-8075-20000186
Copyright: Raghu Sandhya©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
A maxillary midline diastema is a common complaint of dental patients. It can be closed with treatment from different disciplines,
including operative dentistry and orthodontics. A comprehensive smile analysis is also a necessity before beginning treatment. The
aim of the study was to assess the various treatment approaches for the management of midline diastema. Retrospective study
design was formulated for the evaluation of 346 patients with midline diastema was done and the treatment performed for each
case was evaluated. The study population included healthy patients aged from 13 to 55 years, both male and female. MS-Excel
tabulation was done, descriptive statistics and Chi-square analysis were performed using SPSS software. 93.6% of the patients were
treated with fixed appliances for diastema closure while 4.4% of the patients were treated with direct restoration (Composite) and
2% of the patients were treated with indirect restoration (Ceramic). Fixed appliance was the most common preferred treatment of
choice for midline diastema among younger age groups while indirect/direct veneering was preferred among the older age groups
and gender does not influence the choice of treatment among the patients.
2.Introduction
3.Materials and Method
4.Results and Discussion
5.Conclusion
6.Acknowledgement
7.References
Keywords
Midline Diastema; Fixed Appliance; Direct Veneering; Indirect Veneering; Veneers.
Introduction
A space between adjacent teeth is called a diastema. Midline diastema
(or diastemas) occurs in approximately 98% of 6 year olds,
49% of 11 year olds and 7% of 12– 18 year olds [1]. In most
children, the proper eruption path of the maxillary lateral incisors
and canines, will lead to normal closure of this space [2]. In few
individuals, the diastema does not close normally and presence of
a diastema persists between the maxillary central incisors in adults
often is considered an esthetic or malocclusion problem [3]. Midline
diastema can be physiological, due to bony defect, due to a
missing tooth, due to peg shaped lateral, midline supernumerary
teeth, proclination of the upper labial segment, high frenal attachment
or due to a self-inflicted pathology by tongue piercing [4, 5].
The presence of an abnormal frenum is also a cause of midline
diastema [6]. The extent and the etiology of the diastema must be
properly evaluated inorder to provide appropriate treatment and
can produce positive results early in the mixed dentition. Proper
case selection, appropriate treatment selection, adequate patient
cooperation, and good oral hygiene all are important [7, 8].
Many patients seek closure of a diastema for aesthetic reasons. In
the case of normal physiological development, diastemas of less
than 2mm in nine-year-old children are close to normal physiological
function [9]. Smaller diastema (less than 2mm) can be
closed with finger springs on a removable appliance or with a
split Essix plate [10]. In adults with wider diastemas, fixed appliances
are required for correction so that the crown and root of
the teeth are properly angulated [7, 8]. The etiology, pathogenesis
and diagnosis of maxillary median diastema have been somewhat
controversial over the years. Previously our team had conducted
numerous clinical trials [11-17] and lab studies [18-22] and in-vitro studies [23-25] over the past 5 years. Now we are focussing on
epidemiological surveys. The idea for this study stemmed from
the current interest in our community. The aim of this study is to
assess the various treatment approaches for the management of
midline diastema.
The study was conducted with the approval of the Institutional
Ethics Committee [SDC/SIHEC/2020/DIASDATA/
0619-0320]. The study consisted of one reviewer, one assessor
and one guide.
The study was designed to include all dental patients of the ages
13-55 years undergoing treatment for midline diastema . The patients
who did not fall into this inclusion criteria were excluded.
The study was based on a non probability consecutive sampling
method. To minimise sampling bias, all case sheets of patients
who underwent fixed appliance therapy, direct veneering (composite)
and indirect veneering(ceramic) were reviewed and included.
Data Collection was done using the patient database with the
timeframe work 01 June 2019 and 31 march 2020. About 316 case
sheets were reviewed and those fitting under the inclusion criteria
were included. Cross verification was done with the help of Photographs
and radiographic evidence. To minimise sampling bias
all data were included. The exclusion criteria was patients with
systemic illness. Data was downloaded from DIAS and imported
to Excel, Tabulation was done. The values were tabulated and
analysed.
Descriptive statistics were performed using SPSS by IBM on the tabulated values. Chi-Square test was performed and the p value
was determined to evaluate the significance of the variables it was
used to evaluate the association between the age and gender with
the type of treatment done for each patient. The results were obtained
in the form of graphs and tables.
Results and Discussion
After the analysis of 86,000 cases sheets from June 2019 to March
2020, 316 patient case sheets were separated and analysed using
SPSS software. The study population consists of 193 (55.7%)
males and 123 (44.3%) females in which 122 (38.6%) were in the
age group 10-20 years, 190 (60.1%) in 21-31 years, 3 (0.9%) in 32-
42 years, 1 (0.3%) in 43-53 years. Among the patients, 196 (93.6%)
had undergone fixed appliance treatment, 16 (5%) had undergone
direct veneering (composite) and 6 (1.4%) had undergone indirect
veneering (ceramic).
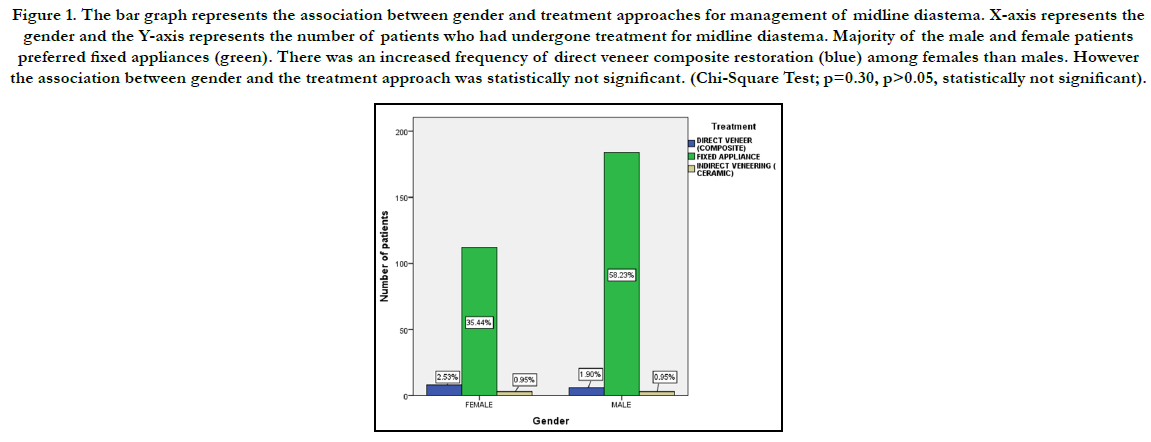
In the present study, fixed appliance was preferred by 35.4% females
and 58.2% males, direct veneering was preferred by 2.5%
females and 1.9% males and indirect veneering was preferred by
0.9% females and males (Figure 1 ). We found that the majority
of the patients with midline diastema have undergone fixed appliance
treatment, followed by direct veneering and the least had undergone
indirect veneering. Higher numbers of patients preferred
fixed appliances while females had a slight inclination towards
direct veneering. However, it was not statistically significant. (Chisquare
test; p=0.30- not significant). Thus, it was inferred that
gender did not influence the choice of treatment.
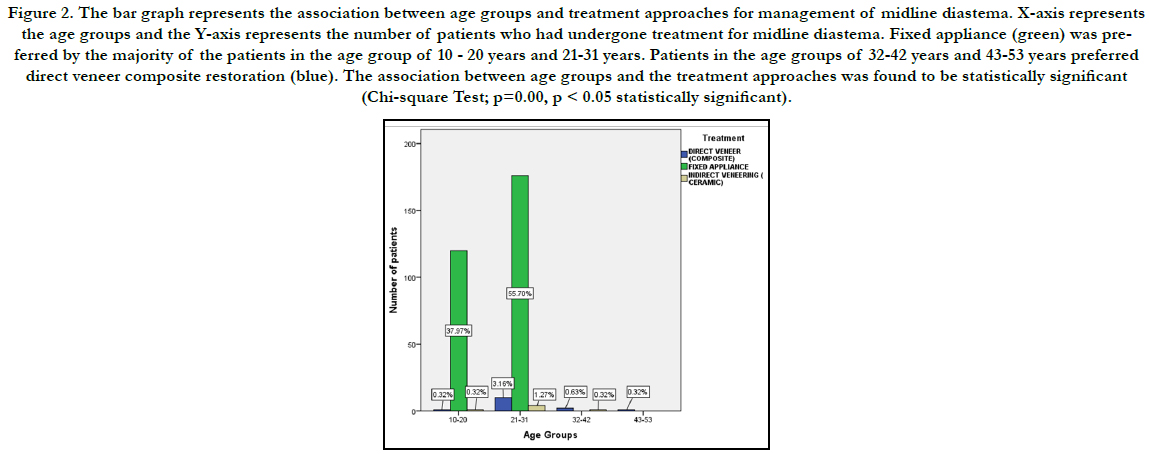
Among the age group of 10-20 years, 120 underwent fixed appliance
treatment, 1 direct veneer and 1 indirect veneering. Among
the age group of 21-31 years, 176underwent fixed appliance treatment,
10 underwent direct veneering and 4 underwent indirect
veneering. Among the age group of 32-42 years, none of the patients
prefered fixed appliance treatment at all, 2 underwent direct
veneering and 1 indirect veneering. Among the age group of 43-
53 years, none of the patients preferred fixed appliance treatment,
1 underwent direct veneering and none of the patients preferred
indirect veneering.
Figure 1. The bar graph represents the association between gender and treatment approaches for management of midline diastema. X-axis represents the gender and the Y-axis represents the number of patients who had undergone treatment for midline diastema. Majority of the male and female patients preferred fixed appliances (green). There was an increased frequency of direct veneer composite restoration (blue) among females than males. However the association between gender and the treatment approach was statistically not significant. (Chi-Square Test; p=0.30, p>0.05, statistically not significant).
Figure 2. The bar graph represents the association between age groups and treatment approaches for management of midline diastema. X-axis represents the age groups and the Y-axis represents the number of patients who had undergone treatment for midline diastema. Fixed appliance (green) was preferred by the majority of the patients in the age group of 10 - 20 years and 21-31 years. Patients in the age groups of 32-42 years and 43-53 years preferred direct veneer composite restoration (blue). The association between age groups and the treatment approaches was found to be statistically significant (Chi-square Test; p=0.00, p < 0.05 statistically significant).
It was found that the majority of the patients who had undergone fixed appliance treatment for midline diastema are in the age group 21-31 years and 10-20 years while the older age groups prefer indirect and direct veneering i.e (32-42 years and 43-53 years). It was found to be statistically significant. (Chi-square test; p=0.00, p <0.05, statistically significant). Thus, it was inferred that an increase in age influences the choice of treatment.
A midline diastema is a space greater than 0.5 mm between the mesial surfaces of maxillary central incisors. This space can be a normal growth characteristic during the primary and mixed dentition period and for most children, with the eruption of the canines, the diastema closure occurs. For some individuals, however, the diastema does not close spontaneously 7,8. Midline diastema are caused due to genetical, physiological, dentoalveolar defects, or due to a missing tooth, due to peg shaped lateral, midline supernumerary teeth, proclination of the upper labial segment, prominent frenum and due to a self-inflicted pathology by tongue piercing [26, 27]. Midline diastema has a racial and familial background but no specific genes have been investigated for its genetic etiogenesis [28] but there are many syndromes and congenital anomalies which contained midline diastema one of their component e.g. Ellis-van Creveld syndrome, Pai Syndrome, lateral incisor agenesis and cleft palate, median cyst.
According to Springate et al, the use of neodymium-iron-boron micro-magnets as a fixed retainer can be used for treating midline spacing [29]. Putter et al., reported two combined modalities of treatment with orthodontic and porcelain laminate placement to facilitate diastema closure. In his report, Geristore, a dual-cure fluoride-releasing composite was mixed to bond orthodontic brackets in place. H-6 elastic bands were used with the orthodontic brackets to close the diastemas sufficiently and to allow the placement of cerinate porcelain laminates to produce a beneficial cosmetic effect [30]. Bell [31] argued for the immediate closure of diastema by subapical and interdental osteotomy, justifying that there is a great unpredictability of diastole orthodontic closure stability and that this approach is difficult and takes a long time. In addition, the author believes that the alveolar bone is the major factor responsible for the difficulty in the orthodontic movement of the teeth and for the final stability, as opposed to the majority of authors who consider the labial frenulum and adjacent soft tissues as the main factor for relapse. The characteristic diastema due to the upper labial frenal attachment naturally closes after the upper lateral incisors and canines erupt. In cases where the diastema does not close, the inferior position of an abnormal frenum can be related to the diastema [32, 33].
There is no proper literature about whether the maxillary labial frenum hypertrophy is the cause or consequence of midline diastema, or about the ideal intervention period for treatment [34]. Frenulum hypertrophy could be a causative factor for relapse of the midline diastema post orthodontic treatment and furthermore, it interferes with the patient’s esthetics and phonetics [35]. According to Attia, if the diastema results from the congenital absence of a lateral incisor, initial treatment is to bring the central incisors together, followed by moving the canines forward into the lateral position or by moving them distally to allow for prosthetic replacement [36]. In other cases, unusually small central or lateral incisors may result in a diastema. Here too, reconstruction by bonding or jacket crowns will solve the problem. According to Kinderknecht and Kupp, resin-bonded porcelain veneer restorations can be used to correct diastema caused by tooth position or discrepancies in the tooth size/arch development [37].
From the above data, we were able to see that the majority of the diastema closure treatment is done using fixed appliance therapy/ orthodontic treatment. However, it is important to establish a treatment plan and determine the cause of the diastemas; they are not recommended when there is ample space between the teeth, because it will not offer a natural solution to the patient [38, 39]. Concern over the stability of results obtained with treatment has existed for more than a century [40]. Almeida et al., [41] have mediated that the closure of diastema in the mixed dentition phase is much more stable than if treated in the permanent dentition. Therefore, it does not require definitive containment, as long as the habit is removed and, in case of interincisal gingival hypertrophy, surgical correction is performed before removal of the device. Fixed retention is often quoted as the only satisfactory method to promote stability for the closure of previous diastemas. However, even if there is a discrepancy of dental size, orthodontic treatment may be an auxiliary tool to redistribute the spaces between the teeth before the restorative procedure. This allows the dentition in the anterior teeth to be performed according to the golden ratio, obtaining a better esthetic result [42, 43].
Conclusion
Within the limitations of the study, it was concluded that the various treatment approaches for the management of midline diastema
included fixed appliance, direct veneer composite restoration,
and indirect veneer ceramic restoration. Majority of the male and
female patients preferred fixed appliances. It was found that fixed
appliance was more preferred among the younger age groups and
direct/indirect veneering was preferred in the older age groups.
Acknowledgement
The authors thank Saveetha Dental College for constant support
in providing the data for analysis.
References
- Keene HJ. Distribution of diastemas in the dentition of man. Am J Phys Anthropol. 1963 Dec;21(4):437-41.
- Taylor JE. Clinical observations relating to the normal and abnormal frenum labii superioris. Am J Orthod Oral Surg. 1939 Jul 1;25(7):646-50.
- Oesterle LJ, Shellhart WC. Maxillary midline diastemas: a look at the causes. J Am Dent Assoc. 1999 Jan;130(1):85-94.Pubmed PMID: 9919036.
- Kaimenyi JT. Occurrence of midline diastema and frenum attachments amongst school children in Nairobi, Kenya. Indian J Dent Res. 1998 Apr- Jun;9(2):67-71.Pubmed PMID: 10530193.
- Angle EH. Treatment of Malocculsion of the Teeth. SS White dental manufacturing Company; 1907.
- McCoy JD. Applied orthodontia: an introductory text for students and practitioners of dentistry. Lea & Febiger; 1922.
- Huang WJ, Creath CJ. The midline diastema: a review of its etiology and treatment. Pediatr Dent. 1995 May-Jun;17(3):171-9. PMID: 7617490.
- Bishara SE, Saunders WB. Textbook of orthodontics. Saunders Book Company; 2001 Mar 21.
- Proffit WR, Fields 3rd HW. Contemporary orthodontics 3rd ed. St. Louis: CV Mosby. 2000:185-95.
- Jacobson A. The Essix appliance technology: applications, fabrication and rationale. American Journal of Orthodontics and Dentofacial Orthopedics 2003; 124: 749.
- Ramamoorthi S, Nivedhitha MS, Divyanand MJ. Comparative evaluation of postoperative pain after using endodontic needle and EndoActivator during root canal irrigation: A randomised controlled trial. Aust Endod J. 2015 Aug;41(2):78-87.Pubmed PMID: 25195661.
- Ramanathan S, Solete P. Cone-beam Computed Tomography Evaluation of Root Canal Preparation using Various Rotary Instruments: An in vitro Study. J Contemp Dent Pract. 2015 Nov 1;16(11):869-72.
- Shenoy A, Bolla N; Sayish, Sarath RK, Ram CH; Sumlatha. Assessment of precipitate formation on interaction of irrigants used in different combinations: an in vitro study. Indian J Dent Res. 2013 Jul-Aug;24(4):451-5. Pubmed PMID: 24047837.
- Rajakeerthi R, Ms N. Natural Product as the Storage medium for an avulsed tooth–A Systematic Review. Cumhur. Dent. J. 2019;22(2):249-56.
- Rajendran R, Kunjusankaran RN, Sandhya R, Anilkumar A, Santhosh R, Patil SR. Comparative Evaluation of Remineralizing Potential of a Paste Containing Bioactive Glass and a Topical Cream Containing Casein Phosphopeptide- Amorphous Calcium Phosphate: An in Vitro Study. Pesqui. Bras. Odontopediatria Clín. Integr. 2019;19.
- Hussainy SN, Nasim I, Thomas T, Ranjan M. Clinical performance of resinmodified glass ionomer cement, flowable composite, and polyacid-modified resin composite in noncarious cervical lesions: One-year follow-up. J Conserv Dent. 2018 Sep-Oct;21(5):510-515.Pubmed PMID: 30294112.
- Kumar D, Antony S. Calcified Canal and Negotiation-A Review. Res J Pharm Technol. 2018;11(8):3727-30.
- Ravinthar K. Recent advancements in laminates and veneers in dentistry. Res J Pharm Technol. 2018;11(2):785-7. .
- Noor S. Chlorhexidine: Its properties and effects. Res J Pharm Technol. 2016;9(10):1755-60.
- Teja KV, Ramesh S, Priya V. Regulation of matrix metalloproteinase-3 gene expression in inflammation: A molecular study. J. Conserv. Dent. 2018 Nov;21(6):592.
- . Janani K, Palanivelu A, Sandhya R. Diagnostic accuracy of dental pulse oximeter with customized sensor holder, thermal test and electric pulp test for the evaluation of pulp vitality: an in vivo study. Braz. Dent. Sci. 2020 Jan 31;23(1):8-p.
- Jose J, Subbaiyan H. Different Treatment Modalities followed by Dental Practitioners for Ellis Class 2 Fracture–A Questionnaire-based Survey. Open Dent J. 2020 Feb 18;14(1).
- Teja KV, Ramesh S. Shape optimal and clean more. Saudi Endod. J. 2019 Sep 1;9(3):235.
- . Manohar MP, Sharma S. A survey of the knowledge, attitude, and awareness about the principal choice of intracanal medicaments among the general dental practitioners and nonendodontic specialists. Indian J Dent Res. 2018 Nov-Dec;29(6):716-720.Pubmed PMID: 30588997.
- Nandakumar M, Nasim I. Comparative evaluation of grape seed and cranberry extracts in preventing enamel erosion: An optical emission spectrometric analysis. J Conserv Dent. 2018 Sep-Oct;21(5):516-520.Pubmed PMID: 30294113.
- Edwards JG. The diastema, the frenum, the frenectomy: a clinical study. Am. J. Orthod. 1977 May 1;71(5):489-508.
- Qazi HS, Ataullah K. Treatment of midline diastema–multidisciplinary managment: a case report. POJ. 2009;1(1):23-7.
- Gass JR, Valiathan M, Tiwari HK, Hans MG, Elston RC. Familial correlations and heritability of maxillary midline diastema. Am J Orthod Dentofacial Orthop. 2003 Jan;123(1):35-9.Pubmed PMID: 12532061.
- Springate SD, Sandler PJ. Micro-magnetic retainers: an attractive solution to fixed retention. Br J Orthod. 1991 May;18(2):139-41.Pubmed PMID: 1911693.
- Putter H, Huberman A, Scherer W. Diastema closure: a case report. J Esthet Dent. 1992; 4 Suppl: 9–11.
- Bell WH. Surgical-orthodontic treatment of interincisal diastemas.Am. J. Orthod. 1970 Feb 1;60:29-32.
- Delli K, Livas C, Sculean A, Katsaros C, Bornstein MM. Facts and myths regarding the maxillary midline frenum and its treatment: a systematic review of the literature. Quintessence Int. 2013 Feb;44(2):177-87.Pubmed PMID: 23444184. .
- Suter VG, Heinzmann AE, Grossen J, Sculean A, Bornstein MM. Does the maxillary midline diastema close after frenectomy? Quintessence Int. 2014 Jan;45(1):57-66.Pubmed PMID: 24392496.
- Wheeler B, Carrico CK, Shroff B, Brickhouse T, Laskin DM. Management of the Maxillary Diastema by Various Dental Specialties. J Oral Maxillofac Surg. 2018 Apr;76(4):709-715.Pubmed PMID: 29245001.
- Koora K, Muthu MS, Rathna PV. Spontaneous closure of midline diastema following frenectomy. J Indian Soc Pedod Prev Dent. 2007 Mar;25(1):23-6. Pubmed PMID: 17456963.
- Attia Y. Midline diastemas: closure and stability. Angle Orthod. 1993 Fall;63(3):209-12.Pubmed PMID: 8214789.
- Kinderknecht KE, Kupp LI. Aesthetic solution for large maxillary anterior diastema and frenum attachment. Pract Periodontics Aesthet Dent. 1996 Jan-Feb;8(1):95-102.Pubmed PMID: 9028276.
- Sundfeld RH, Machado LS, de Oliveira FG, Santos EA, Lugato IC, Sundfeld Neto D. Conservative reconstruction of the smile by orthodontic, bleaching, and restorative procedures. Eur J Dent. 2012 Jan;6(1):105-9.Pubmed PMID: 22229015.
- Prabhu R, Bhaskaran S, Geetha Prabhu KR, Eswaran MA, Phanikrishna G, Deepthi B. Clinical evaluation of direct composite restoration done for midline diastema closure - long-term study. J Pharm Bioallied Sci. 2015 Aug;7(Suppl 2):S559-62.Pubmed PMID: 26538917; PMCID: PMC4606659.
- Reitan K. Principles of retention and avoidance of posttreatment relapse. Am J Orthod. 1969 Jun;55(6):776-90.Pubmed PMID: 4890739.
- Almeida RR, Garib DG, Almeida-Pedrin RR, Almeida MR, Pinzan A, Junqueira MH. Diastema interincisivos centrais superiores: quando e como intervir?. Revista Dental Press de Ortodontia e Ortopedia Facial. 2004 Jun;9(3):137-56.
- Mondelli J, Pereira MA, Mondelli RF. Etiologia e tratamento dos diastemas dentários. Rev Biodonto. 2003 May;1(3):11-111.
- Furuse AY, Franco EJ, Mondelli J. Esthetic and functional restoration for an anterior open occlusal relationship with multiple diastemata: a multidisciplinary approach. J Prosthet Dent. 2008 Feb;99(2):91-4.Pubmed PMID: 18262008.