Bulk Fill Resin Restoration: Clinical Considerations and Case Report
Feitosa FA1*, Esteves SR1, Crastechini E1, Ferraz Caneppele T2, Bresciani E2
1 Department of Restorative Dentistry, São José dos Campos School of Dentistry, Univ Estadual Paulista, Unesp, São José dos Campos, SP, Brazil.
2 Assistant Professor, Department of Restorative Dentistry, São José dos Campos School of Dentistry, UNESP - Univ Estadual Paulista, São Paulo,
Brazil.
*Corresponding Author
Fernanda Alves Feitosa,
Department of Restorative Dentistry, São José dos Campos School of Dentistry,
Univ Estadual Paulista, Unesp, São José dos Campos, SP, Brazil.
Tel: +55 (12) 99738-9265
Fax: +55 (12) 3947-9010
E-mail: fer.feitosa@hotmail.com
Received: July 26, 2018; Accepted: August 28, 2018; Published: August 29, 2018
Citation:Feitosa FA, Esteves SR, Crastechini E, Ferraz Caneppele T, Bresciani E. Bulk Fill Resin Restoration: Clinical Considerations and Case Report. Int J Dentistry Oral Sci. 2018;5(8):655-660. doi: dx.doi.org/10.19070/2377-8075-18000129
Copyright: Feitosa FA©2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The objective of this paper was to present a case report of bulk fill resin restoration, discussing treatment planning and clinical protocol, presenting the follow-ups, and discussing the available literature on the issue. The case report presents a resolution for an extensive carious lesion on the distal surface of the second left maxillary premolar using bulk fill composite. Cavity preparation was made with diamond and carbide round burs. After rubber dam isolation was performed, sectional matrix Unimatrix system and rubber wedge were positioned. Cavity conditioning was performed by etching enamel for 30s and dentin for 15s with 37% phosphoric acid. Cavity was further washed with air/water spray and water excess was removed with cotton ball. The adhesive system was actively applied for 20s, followed by a 5s air blast and light curing for 10s. A single 4mm resin composite (SDR bulk fill – Dentsply) increment was inserted into the cavity being dispensed at the deepest cavity portion and light cured for 20s. Approximately 2mm room was left to allow the insertion of a layer of nanofilled resin to finish the restorative procedure. Finishing and polishing of restoration were performed after 7 days in service and the restoration was evaluated according to Modified USPHS and FDI parameters. After 6 months and 1 year, new assessments were performed following parameters previously cited. No changes in parameters from baseline were detected. The restoration was rated as successful at both evaluation periods.
2.Introduction
3.Materials and Methods
3.1 Diagnosis and Treatment Plan
3.2 Tooth Preparation
3.3 Restorative Procedures
4.Results and Discussion
5.Conclusion
6.References
Keywords
Bulk Fill Composites; Class II Restoration; Clinical Evaluation; Posterior Restoration.
Introduction
Durable resin composite restorations are still challenging in Dentistry. Factors like resin contraction and polymerization stress, and thickness of increments and cusps deflection in composite resin restorations are issues constantly discussed and reviewed by researchers and clinicians, but they still lack a satisfactory solution [1-3].
Resin composite restorations in class II (MOD) cavities, according to Black´s classification, seem to be more subjected to failure [1, 4]. Additionally to previously mentioned problems, such restorations undergo a great incidence of masticatory forces, the contact point/area is difficult to be reestablished, during restorative procedure there are restricted access and vision, they are weaker with increasing cervical length, and they are highly susceptible to poor polymerization [5, 6].
The initial indication of flowable resin composites was intended to assist the dissipation of masticatory forces in deep restorations, being the restoration shrinkage/expansion also less aggressive to the interface tooth/restoration. That technique was recommended as a more flexible liner is used to intermediate the contact between resin composite and tooth substrate [7]. The use of flowable resin composite relies on its less filler content, adequate flow characteristics, low elastic modulus, and proper adhesion to tooth structure [8].
Despite the large number of advantages, the first generation of flowable resin composites, presented in 1996, was not well accepted by clinicians due to lower mechanical properties compared to conventional resins, and still the presence of high degree of polymerization shrinkage, possibly resulting in premature failure of restorations [9].
Currently, flowable resin composites, known as flowable bulk fill resins, were updated. They present increased filler content (approximately 60% in volume), by combining nanosized and larger particles. The use of nanoparticles resulted in lower polymerization shrinkage and therefore lower stresses generation [2]. It has been reported in literature the marginal adaptation in cervical enamel region is similar to restorations performed with bulk fill resin or using conventional incremental technique [10]. The improvements in bulk fill resins were also possible by modifying resin components such as diluents and photo-initiators in its composition [2, 10].
One of the main benefits of restoring teeth with bulk fill resins is the reduced time of the procedure and the maintenance of treatment quality. The conversion degree of resin composites during light curing gradually reduces with depth, decreasing resin physical properties and leading to possible premature failure and pulp damage. ISO 4049 regulates the cure depth of resins by setting 2mm as the maximum thickness suitable for proper polymerization. However, bulk fill resins are reported to light cure in thickness up to 4mm, once they reach hardness properties similar to conventional resin composites after polymerization [11]. The possibility of light curing layers up to 4mm leads to reduced clinical time, resulting in more comfortable procedure for patient and dentist.
Moreover, considering the thickness of resin increments, studies have reported cusp deflection of teeth restored with bulk fill resin was reduced compared to tooth restored using conventional resin composite and the oblique increments technique [2, 11].
Although presenting adequate in vitro results and numerous structural advances, the clinical procedures directly influence the durability of resin composite restorations. Thus, operator skills, and the choice of materials and techniques might favor or impair the outcome. Currently there are restrict in vivo studies and clinical case reports to assist clinicians on proper technique and employment of bulk fill resin composites. Based on that, the objective of this paper is to present a case report of bulk fill resin restoration, discussing treatment planning and clinical protocol, presenting the follow-ups, and also discussing the available literature on the issue.
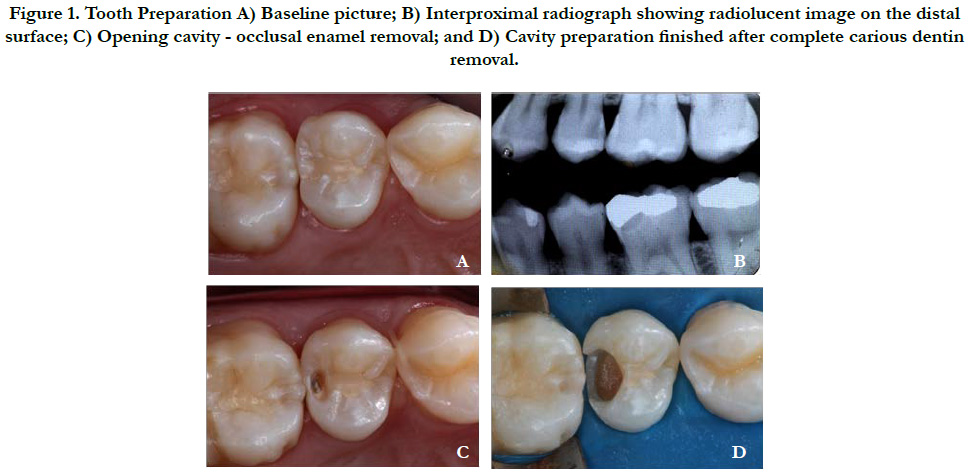
A 24 years-old female patient was admitted for dental treatment at the Dental Clinic of the Institute of Science and Technology - Univ. Estadual Paulista - UNESP in São José dos Campos, Brazil. Her main complaint was the presence of stimulated pain and sensibility on the second left maxillary premolar. Medical history was noncontributory. Clinical and radiographic examinations of target tooth were performed (Figures 1A and 1B). An extensive carious lesion was detected on the distal surface of that tooth, leading to the need of tooth restoration. The choice for resin composite restoration was based on her good oral hygiene and also due to patient’s esthetic requirements. The use of bulk fill resin composite relied on the possibility of proper matrix contouring during the restorative procedures, adequate wedge adaptation and possible reduced time procedure.
Tooth prophylaxis with sodium bicarbonate jet was initially performed to remove dental biofilm (Figure 1A). Tooth color was assessed with classic Vita scale (Vita Zahnfabrik. H. Rauter Gm bH & Co BädSackingen, Germany) under natural light, prior to rubber dam isolation to avoid tooth dehydration. Color A3 color was selected.
Cavity preparation at the distal part of the occlusal surface was initiated with diamond round burs at high speed to remove enamel and access dentin lesion (Figure 1C). Upon reaching the carious dentin, around carbide bur at low speed was used to remove carious tissue (Figure 1D). The leather consistency was the parameter used to determine the complete removal of infected dentin, following the minimum intervention in Dentistry philosophy.
Figure 1. Tooth Preparation A) Baseline picture; B) Interproximal radiograph showing radiolucent image on the distal surface; C) Opening cavity - occlusal enamel removal; and D) Cavity preparation finished after complete carious dentin removal.
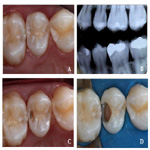
After rubber dam isolation was performed, sectional matrix nimatrix system and rubber wedge were positioned to provide proper cervical adaptation and adequate proximal contour and contact point (Figure 2A).
Cavity conditioning was performed by etching enamel for 30s (Figure 2B) and dentin for 15s (Figure 2C) with 37% phosphoric acid. Cavity was further washed with air/water spray and water excess was removed with cotton ball, avoiding dentin dehydration (Figure 2D).
Figure 2. Cavity Conditioning A) Sectional matrix system – Unimatrix, in position; B) Enamel etching with 37% phosphoric acid for 30s; C) Dentin etching with 37% phosphoric acid for 15s; D) water excess removal with cotton pellet.
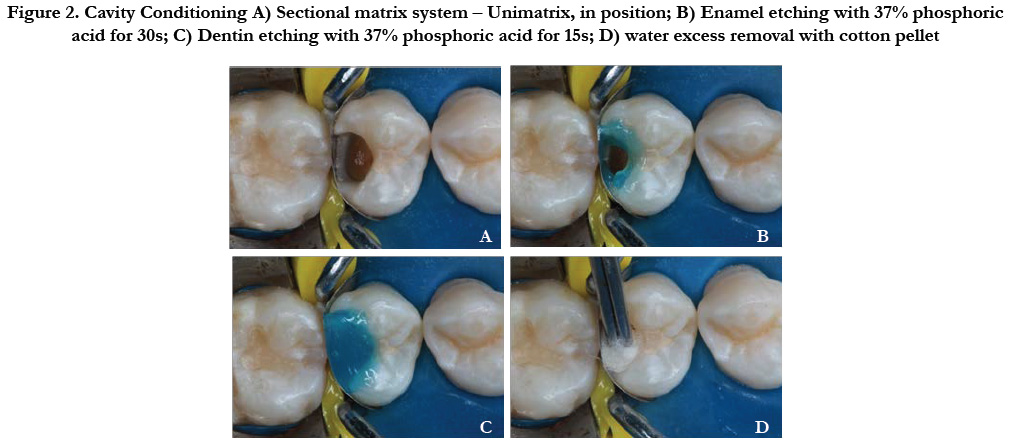
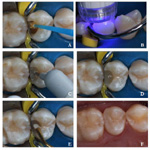
The adhesive system, Single Bond Universal (3M/ESPE) was actively pplied for 20s (Figure 3A), followed by a 5s air blast and light curing for 10s (Figure 3B).
A single 4mm resin composite (SDR bulk fill - Dentsply) increment was inserted into the cavity. Resin insertion was performed according manufacturer instructions, being dispensed at the deepest cavity portion. The applicator tip was submerged for even resin distribution (Figure 3C), avoiding bubble occurrence within the increment (Figure 3D). That single increment was light cured for 20s. Approximately 2mm room was left to allow the insertion of a layer of nanofilled resin (Filtek Z350) (Figure 3E) to finish the restorative procedure. This layer is required due to better mechanical properties of conventional resins in comparison to flowable bulk fill resins.
Finishing and polishing of restoration were performed after 7 ays in service (Figure 3F) and the restoration was evaluated according to the following parameters:
Figure 3. Restorative Procedures A) Application of the adhesive system; B) light curing of adhesive layer for 10s; C) Insertion of SDR Bulk Fill resin composite; D) Cavity filled with SDR Bulk Fill after light curing; E) insertion of nanofilled resin composite Filtek Z350 in the 2mm remaining cavity; F) Final aspect of the restoration after finishing and polishing.
• Modified USPHS - Parameters: retention, marginal discoloration, marginal adaptation, caries recurrence, anatomic form, and post-operative sensitivity were evaluated.
• FDI world dental Federation - Parameters: Contact point, radiographic examination, and periodontal response adjacent to restoration were evaluated.
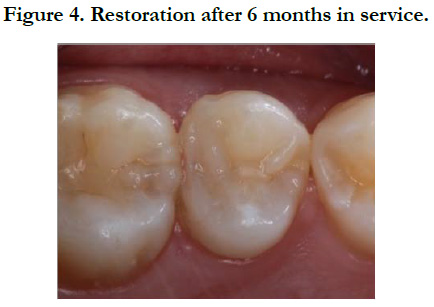
After 6 months (Figure 4) and 1 year, new assessments were performed following parameters previously cited. No changes in parameters from baseline were detected. The restoration was rated as successful at both evaluation periods.
Results and Discussion
Conventional resin composite restorations are usually performed through the incremental technique, inserting 2 mm thick oblique increments. That technique was developed for proper light penetration and to reduce the harmful effects generated by polymerization shrinkage, one of the biggest disadvantages of resin composites. However, the incremental procedure is time consuming, it increases the risk of contamination, if rubber dam is not employed, and empty spaces may exist between increments.
Bulk-fill resins are practical. Resin increments can be up to 4mm in thickness, and its fluid characteristic allows proper resin flow and complete filling with no empty spaces. It presents great translucency and incorporated photoactive group that enables light curing at greater thicknesses [2, 12]. SDR technology has a polymerization modulator to help monomers to form a more flexible polymer network in slower mode, which compensates the effects of volumetric shrinkage.
Investigations showed that bulk fill resins present acceptable mechanical properties compared to conventional resin composites [2, 9, 13, 14].
One quality of bulk fill resins is to significantly reduce cusp deflection during light curing compared to conventional resins restorations performed by the oblique incremental technique [2, 15]. Moorthy et al., 2012 [2], used bulk fill resin in class II as the present case report, and observed reduction of cusps deflection in comparison to restorations performed with multiple oblique increments. The authors believe that reduction was due to deflection of horizontally inserted material at gingival-occlusal direction, reducing the length of cusps and promoting their deflection [2]. The authors however, did not report the amount of material inserted (in volume), and if similar amount of resin is placed horizontally or obliquely the authors conclusion proceeds. A consideration on the comparison between oblique and horizontal increments should be stated on the volume issue; as bulk-fill resins are horizontally inserted in greater volume, that fact might negatively influence the deflection cusp. Cusp deflection of oblique resin increments is also supported by finite element studies. Versluis et al., identified by finite element analysis oblique incremental technique produced higher stress concentration at tooth/restoration interface compared to the horizontal filling techniques [16].
Zorzim et al., 2015 compared the polymerization shrinkage and curing degree of bulk fill resins compared to flowable conventional resins according to their volume. All investigated bulk fill resins presented sufficient polymerization with 4mm thick increments. Most bulk fill resins had lower polymerization volume shrinkage and lower stresses comparing to conventional flowable resin composite, corroborating with other study findings [12]. As manufacturers recommend inserting up to 4mm bulk fill resin increments for proper polymerization, the present clinical case followed those recommendations. The cavity depth was checked with a periodontal probe to assure the bulk fill increment did not exceed 4mm in thickness. An impression of the cavity with addition silicon was performed to determine cavity depth and volume for possible future failure correlations.
Light curing for thirty seconds has been reported to be effective for bulk fill resin polymerization [17]. Czasch P and N Ilie, 2013 reported the conversion degree and mechanical properties of 4mm bulk resin increment are adequate with only 20s light curing [18]. In this clinical case light curing of restoration was carried out for 40 seconds and after removal of the interproximal matrix, light curing was complemented by 20s light exposure on both buccal and lingual aspects. According to the manufacturer's instructions of the currently employed flowable bulk fill resin, 4 mm increments should be light cured for 40s, while 2mm increments require only 20s of light exposure. As there are controversies in the literature, the more adequate approach is to follow the manufacturer’s instructions as performed in the present case scenario.
For obtaining adequate resin polymerization in depth, there is a minimum required energy, fact that might influence the quality of restoration adaptation due to formation of increased stress at interface. The mechanical properties of resin composites are compromised when lower polymerization rates in the deeper areas of resin are detected [19]. Thus, it is necessary to evaluate the amount of transmitted energy by light curing units. The manufacturer recommends the use of a halogen or LED lights at power density equal or greater than 550mW/cm2. In the present clinical case we used the radii-calunit (SDI - Australia) with 1200mW/cm2 of power density, which is considered a high-power LED curing light. This ensures the polymerization of deeper layers of flowable bulk fill resins.
Effective polymerization in depth is related to greater translucency of bulk-fill resins [20], fact that help maintaining their mechanical properties [9, 12, 18]. It is known that light transmission is strongly linked to the opacity of materials [21], and also that increased translucency can be achieved by reduction of resin filler content [22].
Bulk-fill flowable resins have less filler content than the conventional resins but greater content than conventional flowable resins. By reducing the filler content the mechanical properties are reduced (tensile and compressive strengths, and resistance to abrasion), and water sorption is increased [23, 24]. Those concerns might explain the manufacturer’s indication to perform a 2mm occlusal layer of conventional resin when using a flowable bulk fill resin. It has also been reported the elastic modulus and surface hardness of flowable materials are also lower than conventional resins [25].
The proximal aspect of class II restoration performed with flowable bulk fill resin is not covered by conventional resin, so there is a risk of long-term loss of proximal contact due to material wear, greater water sorption water, and resin hydrolysis, being the last two related to material degradation. This possible negative outcome was not detected after one-year follow up in the present case report.
The reestablishment of contact point/area in direct resin restorations is more challenging compared to amalgam or indirect restorations. The main concern is related to wide buccal-lingual proximal cavities. Some techniques aid proximal contact point reestablishment when performing direct resin composites restorations, such as the use of contact spatula (reflective or not). For bulkfill restorations, the use of contact spatulas might difficult the procedure itself, once it is a flowable resin. To obtain proper contact point in present case report, which presents a wide buccallingual cavity, a concave sectional matrix, an individual ring, and a well-adapted wedge were employed.
According to FDI parameters for contact point evaluation, 25, 50 and 100μm metal strips are tested to pass at the target interproximal contact, and the ideal scenario is represented by passing the 25μm strip without exacerbated pressure. All evaluated periods (baseline, 7 days, 6 months and 1 year) of the present case report presented ideal contact point characteristics.
In a 3-year study comparing the same flowable bulk fill resin as used in the present case, the anatomical form, marginal adaptation, color, marginal staining, surface roughness, and the presence of secondary caries were evaluated. Failure rates were 1.3% for conventional restorations and 0% for bulk fill restorations, leading to a conclusion bulk-fill restoration showed acceptable clinical results comparable to conventional incremental technique [26].
Regarding postoperative sensitivity, the present patient reported discomfort at the first days, which had ceased at the one-week follow up. This fact has been also detected in a clinical trial, where only one out of 138 patients reported postoperative sensitivity during the first three weeks, as a result of temperature changes and occlusal forces [26]. The reason for sensitivity after restorative procedures is not completely known and, besides being subjective, it may be related to lack of irrigation during tooth preparation, to excessive drying of dentin during bonding procedures, and might also be related psychological condition of patients. Due to the short-term sensitivity present in the clinical case and the low incidence previously reported [26], this fact might not be a concern for employing the bulk fill resin approach.
More studies are required to improve bulk fill resin mechanical properties and to increase depth of cure, in order to allow their use in wider/deeper cavities. More long-term clinical studies are necessary to support evidence-based employment of bulk fill resins.
Conclusion
Bulk fill flowable resin restorations seem to be promising as they present acceptable mechanical properties and simplified clinical steps. Cavities receiving bulk fill resins can present 6mm in depth, and would be filled with two increments opposing to at least 3 increments using the conventional oblique technique. On the other hand, that simplification can be questioned, as the reestablishment of contact point/area is not facilitated and the use of covering layer of conventional resin composite is required.
References
- Dejak B, Młotkowski A. A comparison of stresses in molar teeth restored with inlays and direct restorations, including polymerization shrinkage of composite resin and tooth loading during mastication. Dent Mater. 2015 Mar;31(3):e77-87. doi: 10.1016/j.dental.2014.11.016. PubMed PMID: 25544104.
- Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJ. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent. 2012 Jun;40(6):500-5. doi: 10.1016/j.jdent.2012.02.015. PubMed PMID: 22390980.
- van Dijken JW. Durability of resin composite restorations in high C-factor cavities: a 12-year follow-up. J Dent. 2010 Jun;38(6):469-74. doi: 10.1016/j. jdent.2010.02.007. PubMed PMID: 20193727.
- Ferrario VF, Sforza C, Serrao G, Dellavia C, Tartaglia GM. Single tooth bite forces in healthy young adults. J Oral Rehabil. 2004 Jan;31(1):18-22. PubMed PMID: 15125591.
- Kuper NK, Opdam NJ, Bronkhorst EM, Huysmans MC. The influence of approximal restoration extension on the development of secondary caries. J Dent. 2012 Mar;40(3):241-7. doi: 10.1016/j.jdent.2011.12.014. PubMed PMID: 22226997.
- Lempel E, Tóth Á, Fábián T, Krajczár K, Szalma J. Retrospective evaluation of posterior direct composite restorations: 10-year findings. Dent Mater. 2015 Feb;31(2):115-22. doi: 10.1016/j.dental.2014.11.001. PubMed PMID: 25480695.
- Arslan S, Demirbuga S, Ustun Y, Dincer AN, Canakci BC, Zorba YO. The effect of a new-generation flowable composite resin on microleakage in Class V composite restorations as an intermediate layer. J Conserv Dent. 2013 May;16(3):189-93. doi: 10.4103/0972-0707.111311. PubMed PMID: 23833448.
- Alonso RC, Sinhoreti MA, Correr Sobrinho L, Consani S, Goes MF. Effect of resin liners on the microleakage of class V dental composite restorations. J Appl Oral Sci. 2004 Mar;12(1):56-61. PubMed PMID: 21365153.
- Van Ende A, De Munck J, Van Landuyt KL, Poitevin A, Peumans M, Van Meerbeek B. Bulk-filling of high C-factor posterior cavities: effect on adhesion to cavity-bottom dentin. Dent Mater. 2013 Mar;29(3):269-77. doi: 10.1016/j.dental.2012.11.002. PubMed PMID: 23228335.
- Agarwal RS, Hiremath H, Agarwal J, Garg A. Evaluation of cervical marginal and internal adaptation using newer bulk fill composites: An in vitro study. J Conserv Dent. 2015 Jan-Feb;18(1):56-61. doi: 10.4103/0972-0707.148897. PubMed PMID: 25657529.
- Flury S, Hayoz S, Peutzfeldt A, Hüsler J, Lussi A. Depth of cure of resin composites: is the ISO 4049 method suitable for bulk fill materials?. Dent Mater. 2012 May;28(5):521-8. doi: 10.1016/j.dental.2012.02.002. PubMed PMID: 22391146.
- Ilie N, Hickel R. Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent Mater. 2011 Apr;27(4):348-55. doi: 10.1016/j.dental.2010.11.014. PubMed PMID: 21194743.
- El-Safty S, Silikas N, Watts DC. Creep deformation of restorative resin-composites intended for bulk-fill placement. Dent Mater. 2012 Aug;28(8):928- 35. doi: 10.1016/j.dental.2012.04.038. PubMed PMID: 22656273.
- Roggendorf MJ, Krämer N, Appelt A, Naumann M, Frankenberger R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J Dent. 2011 Oct;39(10):643-7. doi: 10.1016/j.jdent.2011.07.004. PubMed PMID: 21801799.
- Tomaszewska IM, Kearns JO, Ilie N, Fleming GJ. Bulk fill restoratives: To cap or not to cap - That is the question?. J Dent. 2015 Mar;43(3):309-16. doi: 10.1016/j.jdent.2015.01.010. PubMed PMID: 25625673.
- Versluis AB, Douglas WH, Cross MB, Sakaguchi RL. Does an incremental filling technique reduce polymerization shrinkage stresses?. J Dent Res. 1996 Mar;75(3):871-8. PubMed PMID: 8675797.
- Zorzin J, Maier E, Harre S, Fey T, Belli R, Lohbauer U, et al. Bulk-fill resin composites: polymerization properties and extended light curing. Dent Mater. 2015 Mar;31(3):293-301. doi: 10.1016/j.dental.2014.12.010. PubMed PMID: 25582061.
- Czasch P, Czasch P, Ilie N. In vitro comparison of mechanical properties and degree of cure of bulk fill composites. Clin Oral Investig. 2013 Jan;17(1):227-35. doi: 10.1007/s00784-012-0702-8. PubMed PMID: 22411261.
- Campodonico CE, Tantbirojn D, Olin PS, Versluis A. Cuspal deflection and depth of cure in resin-based composite restorations filled by using bulk, incremental and transtooth-illumination techniques. J Am Dent Assoc. 2011 Oct;142(10):1176-82. PubMed PMID: 21965491.
- Bucuta S, Ilie N. Light transmittance and micro-mechanical properties of bulk fill vs. conventional resin based composites. Clin Oral Investig. 2014 Nov;18(8):1991-2000. doi: 10.1007/s00784-013-1177-y. PubMed PMID: 24414570.
- Shortall AC. How light source and product shade influence cure depth for a contemporary composite. J Oral Rehabil. 2005 Dec;32(12):906-11. Pub- Med PMID: 16297038.
- Lee YK. Influence of filler on the difference between the transmitted and reflected colors of experimental resin composites. Dent Mater. 2008 Sep;24(9):1243-7. doi: 10.1016/j.dental.2008.01.014. PubMed PMID: 18343494.
- Ferracane JL. Resin composite -- state of the art. Dent Mater. 2011 Jan;27(1):29-38. doi: 10.1016/j.dental.2010.10.020. PubMed PMID: 21093034.
- Valente LL, Peralta SL, Ogliari FA, Cavalcante LM, Moraes RR. Comparative evaluation of dental resin composites based on micron-and submicronsized monomodal glass filler particles. Dent Mater. 2013 Nov;29(11):1182-7. doi: 10.1016/j.dental.2013.09.006. PubMed PMID: 24095108.
- Ilie N, Bucuta S, Draenert M. Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Oper Dent. 2013 Nov- Dec;38(6):618-25. doi: 10.2341/12-395-L. PubMed PMID: 23570302.
- van Dijken JW, Pallesen U. A randomized controlled three year evaluation of “bulk-filled” posterior resin restorations based on stress decreasing resin technology. Dent Mater. 2014 Sep;30(9):e245-51. doi: 10.1016/j.dental. 2014.05.028. PubMed PMID: 24958689.