The Pioneer Bridge: A Long-Term, Non-Invasive, Esthetic Composite Bonded Bridge for the Replacement of Anterior Teeth
Fan (Stefanie) Wang1, Carlin V. Cera1, Olga J. Baker2*, Joel N. Janis2,3*
1 Graduate Student, Roseman University of Health Sciences College of Dental Medicine, S River Front Pkwy, South Jordan, Utah, USA.
2 Associate Professor, University of Utah, School of Dentistry, 530 South Wakara Way, Salt Lake City, UT, USA.
3 Associate Professor, Roseman University of Health Sciences College of Dental Medicine, S River Front Pkwy, South Jordan, Utah, USA.
*Corresponding Author
Olga J. Baker DDS, PhD,
Associate Professor,University of Utah,
School of Dentistry, 530 South Wakara Way, Salt Lake City, UT 84108, USA.
Tel: 801-587-1773
E-mail: olga.baker@hsc.utah.edu
Joel N. Janis DDS, PhD,
Associate Professor, Roseman University of Health Sciences College of Dental Medicine,
10894 S River Front Pkwy, South Jordan, Utah 84095, USA.
Associate Professor, University of Utah, School of Dentistry,
530 South Wakara Way, Salt Lake City Utah 84108, USA.
Tel: 801-587-1773
Fax: 801-595-6712
E-mail: joel.janis@hsc.utah.edu
Received: April 19, 2018; Accepted: April 27, 2018; Published: April 30, 2018
Citation:Fan (Stefanie) Wang, Carlin V. Cera, Olga J. Baker, Joel N. Janis. The Pioneer Bridge: A Long-Term, Non-Invasive, Esthetic Composite Bonded Bridge for the Replacement of Anterior Teeth. Int J Dentistry Oral Sci. 2018;5(4):630-634. doi: dx.doi.org/10.19070/2377-8075-18000123
Copyright: Olga J. Baker, Joel N. Janis©2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objectives: The purpose of this study was to evaluate the retentive strength of the Pioneer Resin Bonded Bridge design with no abutment teeth preparations in comparison to the standard Maryland Bridge design.
Materials and Methods: Sample Pioneer and Maryland Bridges were fabricated and tested with an Instron machine to evaluate the amount of Pound Force units necessary to cause bridge dislodgement. The Pioneer Bridges were fabricated with a zirconia framework and a porcelain fused to zirconia pontic. Then, Pioneer Bridges were locked to the teeth with micro hybrid composite while the Maryland bridges were cemented with Panavia.
Results: The Pioneer Bridges showed 4.0-fold higher retentive strength as compared to the Maryland Bridges tested in this study.
Conclusion: This study provides evidence indicating that Pioneer Bridges may improve the current treatment for adolescent patients with congenitally missing lateral incisors for whom implants are not a viable option due to incomplete skeletal growth as well a lower cost alternative for adult patients missing an anterior tooth who cannot afford an implant.
Clinical Implications: Esthetics are enhanced with Pioneer Bridges as compared to the Maryland Bridge, given the translucency of the former as compared to the metallic finish of the latter. Additionally, the Pioneer Bridge does not require that the adjacent incisors be damaged for anchoring purposes as is the case with the Maryland Bridge. Also, the Pioneer Bridge expands the age for which a bridge may be employed to adolescents, given that it is not permanently fixed and therefore can be removed with subsequent skeletal growth and replaced with a larger version of the same or an implant upon reaching adulthood. Finally, the cost of a Pioneer Bridge is expected to be significantly lower due to reduced clinician time owing to a lack of tooth preparation.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.References
Keywords
Anterior Teeth; Congenitally Missing Teeth; Debonding, Resin-Bonded Fixed Dental Prosthesis; Zirconia Ceramic Bonding.
Introduction
Previous studies have indicated a variety of both temporary and permanent solutions for the replacement of missing anterior teeth [1-3]. Specifically, various bonded bridge designs have been commonly used [4, 5]. The Maryland and Carolina Bridges are currently available as viable options; however, both designs have significant disadvantages [6-8]. The Maryland Bridge preparation requires tooth structure removal on the abutment teeth [7]. Clinicians can elect not to remove as much tooth structure; however, the lifespan of the bridge is significantly reduced [9, 10]. The recommendation for the fabrication of the Maryland Bridge is to carry the metal framework interproximally and add grooves to increase retention [11, 12]. In addition, the lingual wings on the abutment teeth have to be flush with the incisal edges to maxmize coverage and retention [7]. Metal show through is often a consequence of this requirement, resulting in patient dissatisfaction with esthetics [13]. Finally, the Rochette bridge could offer an alternative; however, this bridge has only a moderate rate of success due to the low retention bridge design (i.e., multiple randomly placed perforations) and cement failure over time [9, 14, 15].
The Carolina Bridge is one of the recent innovations in bonded bridges intended to resolve the esthetic problems associated with the Maryland Bridge design [8]. It requires minimum interproximal reduction of abutment teeth; however, the technique requires flattening of the interproximal surfaces of the abutment teeth up to 5 mm incisal-gingival length to obtain adequate bonding for retention [8]. This bridge design consists of bonding a porcelain pontic to the adjacent teeth with microhybrid composite interproximally without relying on lingual stabilizing wings, as previously required by the Maryland Bridge [8]. However, the Carolina Bridge is prone to pontic dislodgement, in which case the clinician is required to recontour and restore the abutment teeth prior to installing an implant supported crown.
Due to the amount of tooth structure removal and esthetic concerns involved with the bridges discussed above, we created a novel bridge design requiring little to no tooth structure removal with improved esthetics as well as solid longevity. This bonded bridge design is termed the “Pioneer Bridge.” The technique has been utilized by our corresponding author, Dr. Joel Janis, DDS for 30 years on patients in private practice and at the University of the Pacific Dental School Clinic, with an average lifespan of approximately 20 years (personal observation).
The initial design of the Pioneer Bridge was constructed with a metal framework to which a porcelain pontic was fused. In it, the metal framework covers the lingual surface excluding the incisal third of abutment teeth to prevent metal show-through on the translucent incisal edge of the abutment teeth. Due to the unique retentive features of the Pioneer Bridge, lingual surfaces of the wings do not need to extend to the incisal edge. In addition, the metal framework of the pontic is kept to the lingual surface while being covered with porcelain facially and interproximally to keep the metal out of the esthetic zone. Zirconia material has become an alternative choice for the framework of the fixed prosthesis due to its durability, similarity in color to natural teeth and affordability [16-18]. The original BruxZir material is superior in strength, toughness, and ability to tolerate stress and abuse compared to the new translucent zirconia formulations [19]. Therefore, the material of choice for the Pioneer Bridge in this study is the original formula of zirconia, “The Original BruxZir.” Note that while conventional zirconia has reduced transmission light, we overcome this issue by increasing the time of light curing.
The Pioneer Bridge technique can be utilized for the replacement of an anterior tooth. While the mandibular second premolar is the tooth most affected by agenesis, it is followed by the maxillary lateral incisor and the maxillary second premolar as the second most common missing teeth [20]. This design is a viable treatment option for adolescent patients with congenitally missing lateral incisors, allowing for minimal tooth structure removal on abutment teeth. Since implant placement is not indicated until the cessation of skeletal growth [21]. The Pioneer Bridge can be placed during the growth period to maintain the esthetics and the space for future implant placement.
Materials and Methods
Human studies have been approved by the University of Utah Institutional Review Board on September 26th 2017 under the number IRB_00105630. Teeth used in this study were selected based upon the following criteria: no existing restorations, void of fractures, no caries, and sound root structure. The mesiodistal width of the maxillary central incisors and maxillary canines were confined to 8-10 mm and 10-12 mm, respectively. Roots were notched 1 mm axially with an offset placement. Extracted teeth were mounted in poly(methyl methacrylate) (PMMA) material instead of traditional stone to give improved strength and prevent dislodgement of the teeth during the testing process. We created cingulum rest preparations using a #2 round in mounted teeth. Next,teeth with preparations were sent to Arrowhead Dental Laboratory (Sandy, UT) for fabrication per investigator instructions, as detailed below.
Upon receiving the completed bridges from the dental laboratory, a framework try-in was completed prior to cementation. The following cementation process was performed: internal surfaces of the framework and proximal surfaces of the porcelain pontic were micro-etched with aluminum oxide (50 microns) for 5 seconds followed by porcelain etch using 9.6% hydrofluoric acid applied on the proximal surfaces of the pontic for 2 min then thoroughly washed and dried. Next, proximal surfaces of the etched porcelain were coated with silane (coupling agent) and dried. Finally, dentin primer/bonding agent (Peak Universal, Ultradent) was rubbed in for 10 seconds followed by air thinning for 10 seconds. Light was then cured on the internal surface of retention wings and proximal surfaces of the pontic for 20 seconds. The teeth were then cleansed with flour of pumice in a prophylaxis cup, washed and dried. Then, enamel on lingual and proximal surfaces of the abutment teeth was etched with 35% phosphoric acid (Ultra-etch) for 20 seconds, washed and dried. Next, primer/adhesive (Peak Universal) was rubbed in for 10 seconds followed by air thinning for 10 seconds and light cured for 20 seconds. Following this procedure, micro hybrid composite (Amelogen Plus, Ultradent), a commonly used restorative material, was placed on the internal surfaces of framework wings and proximal surfaces of the pontic.
The Pioneer Bridge was gradually seated completely by engaging the cingulum rests, excess composite was expressed along the entire periphery of the framework, through the retentive holes, and from the labial embrasures. Excess composite was then removed from the labial, incisal, lingual, and gingival embrasures. The labial surface of the porcelain pontic was light cured for 2 seconds to fix the prosthesis in place, which leaves the lingual composite uncured to allow for the same procedure that was completed for the labial surface. All surfaces of the composite beneath the framework were then polymerized with a 40 second light cure from each angle for zirconia frameworks. Panavia F2.0 (Kuraray America, Inc.) was used as per the manufacturer’s instructions for the cementation of the Maryland Bridges. Testing was then performed using orthodontic NiTi 0.017X0.025 wires looped beneath the connector areas and attached to Instron Material Testing Machine 4467 (Instron). Finally, bridge retentive strength was evaluated in Pound Force units with tensile test straight pull of 1 mm/minute lift.
Results
The design purpose of the Pioneer Bridge was to preserve tooth structure on the abutment teeth and to prolong the lifespan of the bonded bridge, until the patient has completed skeletal growth and/or can afford an implant retained esthetic crown [21, 22]. The unique design features of the Pioneer Bridge, as shown in Fig.1A-B, include 1) interproximal bonding of etched porcelain to etched enamel, 2) 45º beveled edges on the periphery of the retentive wings to lock the prosthesis in position with a 1 mm bead of micro hybrid composite (Figure 1A), and 3) evenly spread countersunk holes to the lingual of retentive wings to enhance prosthesis by locking wings in position to gain maximum retention (Figure 1B). In addition, rest seats on abutment teeth prevent over seating of the bridge and preserve tooth structure with minimum tooth preparation in the enamel only. Micro etching the intaglio or internal surfaces of the retentive wings enhances a micromechanical bond. The location of the retentive holes must avoid the rest seat area as seen in Figure 1B.
The zirconia frameworks were designed using CAD/CAM technology and illustrated in Figure 1C-H. One maxillary central incisor and one maxillary canine were paired and mounted in poly methyl methacrylate material. The mounted casts were scanned prior to framework fabrication. The design of the zirconia framework follows the design features mentioned previously and requires porcelain (e.g., EMAX Ceram) fused to the zirconia to create a pontic that is both esthetically pleasing and allows optimal bond strength interproximally.
Figure 1. Framework designs of the Pioneer Bridge’s. Artist’s conception of retentive features of the Pioneer Bridge design. A) Pioneer Bridge lingual view, and B) Pioneer Bridge cross sectional view of canine. C) Pioneer Bridge CAD/CAM printouts of the lingual view. D) Pioneer Bridge CAD/CAM printouts of the incisal view. E) Maryland Bridge intaglio view. F) Fabricated Pioneer Bridge intaglio view, and G) Fabricated Pioneer Bridge incisal view. H) Pioneer Bridge Labial view of the illustrating composite bonded interproximally.
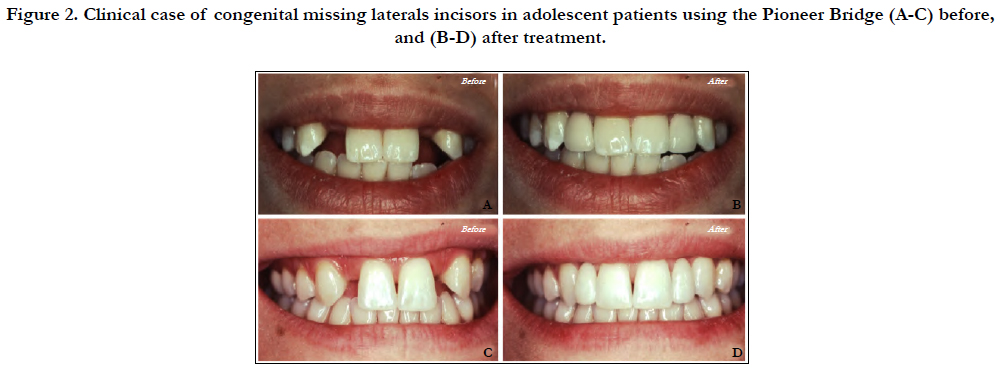
If cast metal is used for the framework, porcelain is fused to the pontic area and the metal framework is kept on the lingual surface to avoid metal showing through the abutment teeth. Figure 2A-B and Figure 2C-D illustrate two clinical cases of before and after treatment. By avoiding the incisal third and by having no metal placed interproximally, the metal framework has an improved esthetic result in comparison to the traditional Maryland Bridge, which requires bringing the metal (i.e., a non-precious dental alloy) interproximally for additional retention [23-25]. The illustrated cases consist of adolescent patients with congenitally missing maxillary lateral incisors that are replaced with a Pioneer Bridge to allow the option of an implant after the cessation of skeletal growth. Figure 2E provides an incisal view of bilateral bridges with metal framework that were placed for the replacement of missing maxillary lateral incisors. Patients were pleased with the esthetic outcome with the metal framework bridge. With the advances of today’s dental materials [4, 11] zirconia is used as the framework for the Pioneer Bridge and is recommended.
Figure 2. Clinical case of congenital missing laterals incisors in adolescent patients using the Pioneer Bridge (A-C) before, and (B-D) after treatment.
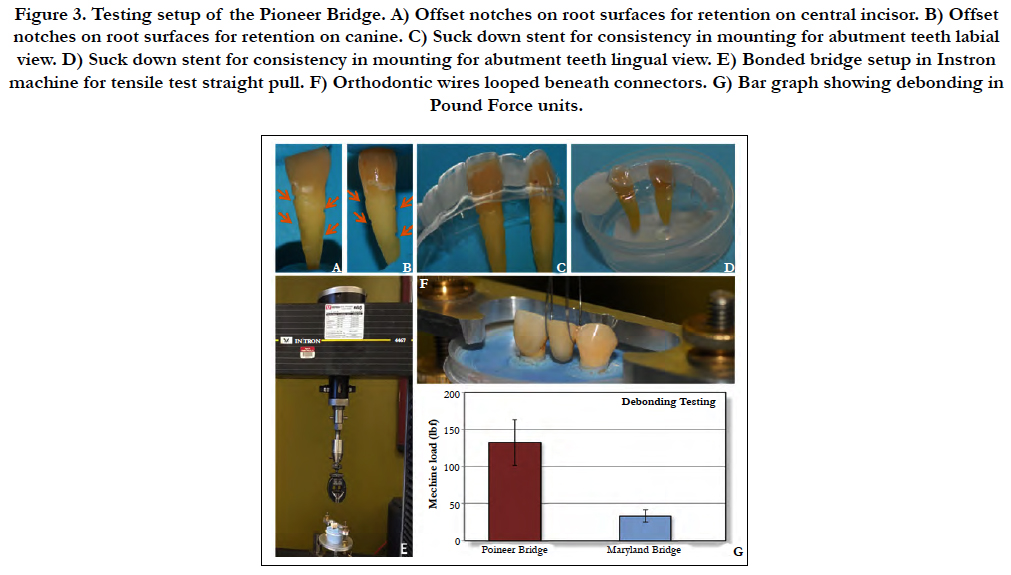
In order to quantify the debonding strength of the Pioneer Bridge and to compare the strength to the traditional cemented bridge design (i.e., the Maryland Bridge), extracted teeth were used for the fabrication of the bridges. Central incisors and canines were selected as abutment teeth. Three notches on the mesial and distal root surfaces were offset and 1 mm depth axially as seen in Figure 3A-B. To standardize the arch form and the pontic space, a suck down stent was fabricated from a Kilgore typodont (Cat# D95SDP- 200, Kilgore International Inc., Coldwater, MI), as shown in Figure 3C-D. A strip of bead wax was placed along the incisal edges of the internal surfaces of the stent to hold the paired central incisors and canines in place and to avoid shifting of the teeth during the mounting process. Poly methyl methacrylate was used to mount the teeth in the casts. Mounted teeth were scanned and bridges were fabricated. The Pioneer Bridge was bonded with Amelogen Plus micro hybrid composite. The Maryland Bridge was cemented with Panavia F2.0, as per the manufacturer’s instructions. The retentive strength of the bridges was tested with the Instron testing machine 4467 (Figure 3E). Orthodontic NiTi 0.017X0.025 wires were looped beneath the connector areas (Figure 3G). Bridge retentive strength was evaluated in Pound Force units with tensile test straight pull of 1 mm/minute lift (Figure 3F). The degree of fracture was evaluated through the Instron computer readout. The Maryland Bridges dislodged at an average of 33.2 Pound Force as seen in Figure 3H. The retentive strength of the Pioneer Bridge’s was at an average of 132.4 Pound Force (Figure 3H) which is 4.0-fold higher than that of the Maryland Bridge. Abutment teeth fractured simultaneously with debonding of the Pioneer Bridges. Conversely, the Maryland Bridges were debonded without tooth fracture.
Figure 3. Testing setup of the Pioneer Bridge. A) Offset notches on root surfaces for retention on central incisor. B) Offset notches on root surfaces for retention on canine. C) Suck down stent for consistency in mounting for abutment teeth labial view. D) Suck down stent for consistency in mounting for abutment teeth lingual view. E) Bonded bridge setup in Instron machine for tensile test straight pull. F) Orthodontic wires looped beneath connectors. G) Bar graph showing debonding in Pound Force units.
Discussion
For patients with congenitally missing lateral incisors, implants cannot be placed until cessation of skeletal growth [21]. Alternatively, fixed bonded bridges can be placed if the space is sufficient [7]. If the patient is going to undergo orthodontic treatment, then proper space maintenance is indicated [26, 27]; however, the Pioneer Bridges can be utilized during adolescence. If the patient requires orthodontic treatment, coordination with the orthodontist is helpful to ensure incisal clearance is 1 mm to allow for proper framework thickness and that there is adequate mesial distal space for an esthetic pontic. If there is less than 1 mm of incisal clearance, minor tooth movement is indicated as opposed to removal of enamel.
Initially this bonded bridge was designed using a porcelain fused to metal pontic and a metal framework. Now, zirconia frameworks have similar strength with several advantages [28-31]. For instance, light curing can pass through the zirconia material [32, 35]. Zirconia is tooth colored allowing for improved esthetics without possible metal show-through [36-39]. Porcelain can be fused to micro etched zirconia for good pontic esthetics [40]. In addition, porcelain can be etched interproximally to achieve a stronger bond to the interproximal enamel [41]. It is crucial that the original material is used in this technique as opposed to the newer translucent zirconia products which are not comparable in strength [16, 18].
During fabrication, it is advantageous if the laboratory can complete the countersunk holes and place a 45º bevel around the wing periphery, as chairside preparation is costly and time consuming due to material hardness. A traditional PVS final impression with a bite registration is taken to send to the dental laboratory. With respect to the lingual cingulum stop preparation, this may not be necessary if a deep fossa is present on the lingual surface of the abutment teeth. The purpose of the lingual cingulum stop preparation is to prevent over seating of the bridge during the bonding process. Based on clinical experience, we can anticipate the Pioneer Bridge will be durable in comparison to other types of bonded bridges.
References
- Augusti D, Augusti G, Re D. Prosthetic restoration in the single-tooth gap: patient preferences and analysis of the WTP index. Clin Oral Implants Res. 2014;25:1257-64. PubMed PMID: 24021020.
- Stylianou A, Liu PR, O'Neal SJ, Essig ME. Restoring Congenitally Missing Maxillary Lateral Incisors Using Zirconia-Based Resin Bonded Prostheses. J Esthet Restor Dent. 2016 Jan-Feb;28(1):8-17. PubMed PMID: 26361239.
- Zitzmann NU, Ozcan M, Scherrer SS, Buhler JM, Weiger R, Krastl G. Resin-bonded restorations: a strategy for managing anterior tooth loss in adolescence. J Prosthet Dent. 2015 Apr;113(4):270-6. PubMed PMID: 25702966.
- Sailer I, Balmer M, Husler J, Hammerle CHF, Kanel S, Thoma DS. Comparison of Fixed Dental Prostheses with Zirconia and Metal Frameworks: Five-Year Results of a Randomized Controlled Clinical Trial. Int J Prosthodont. 2017 Sep/Oct;30(5):426–428. PubMed PMID: 28750109.
- Thoma DS, Sailer I, Ioannidis A, Zwahlen M, Makarov N, Pjetursson BE. A systematic review of the survival and complication rates of resin-bonded fixed dental prostheses after a mean observation period of at least 5 years. Clin Oral Implants Res. 2017 Nov;28(11):1421-1432. PubMed PMID: 28191679.
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications in fixed prosthodontics. J Prosthet Dent. 2003 Jul;90(1):31-41. PubMed PMID: 12869972.
- Durey KA, Nixon PJ, Robinson S, Chan MF. Resin bonded bridges: techniques for success. Br Dent J. 2011 Aug 12;211(3):113-8. PubMed PMID: 21836574.
- Heymann HO. The Carolina bridge: a novel interim all-porcelain bonded prosthesis. J Esthet Restor Dent. 2006;18(2):81-92. PubMed PMID: 16519872.
- Berekally TL, Smales RJ. A retrospective clinical evaluation of resin-bonded bridges inserted at the Adelaide Dental Hospital. Aust Dent J. 1993 Apr;38(2):85-96. PubMed PMID: 8494517.
- Smales RJ, Berekally TL. Long-term survival of direct and indirect restorations placed for the treatment of advanced tooth wear. Eur J Prosthodont Restor Dent. 2007 Mar;15(1):2-6. PubMed PMID: 17378451.
- Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J. Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent Mater. 2009 Jan;25(1):94-102. PubMed PMID: 18620749.
- Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent. 2002 Jun;22(3):241-9. PubMed PMID: 12186346.
- Wright JT, Cashion S, Hoover R. The esthetic stainless steel crown bridge: report of two cases. Pediatr Dent. 1999 Mar-Apr;21(2):137-41. PubMed PMID: 10197344.
- Banerji S, Sethi A, Dunne SM, Millar BJ. Clinical performance of Rochette bridges used as immediate provisional restorations for single unit implants in general practice. Br Dent J. 2005 Dec 24;199(12):771-5. PubMed PMID: 16395362.
- Ziada HM, Orr JF, Benington IC. Photoelastic stress analysis in perforated (Rochette) resin bonded bridge design. J Oral Rehabil. 2000 May;27(5):387-93. PubMed PMID: 10887911.
- Christensen G. The future: materials, challenges in dentistry, and education. Interview by Dr. Damon Adams. Dent Today. 2012 Feb;31(2):102,104,106. PubMed PMID: 22413390.
- Christensen GJ. Use of luting or bonding with lithium disilicate and zirconia crowns. J Am Dent Assoc. 2014 Apr;145(4):383-6. PubMed PMID: 24686975.
- Christensen R. Rella Christensen. Discusses the newest in zirconia restorations and how zirconia is changing. Dent Today. 2015;34:14.
- Hamza TA, Sherif RM. In vitro evaluation of marginal discrepancy of monolithic zirconia restorations fabricated with different CAD-CAM systems. J Prosthet Dent. 2017 Jun;117(6):762-766. PubMed PMID: 27836145.
- Polder BJ, Van't Hof MA, Van der Linden FP, Kuijpers-Jagtman AM. A meta-analysis of the prevalence of dental agenesis of permanent teeth. Community Dent Oral Epidemiol. 2004 Jun;32(3):217-26. PubMed PMID: 15151692.
- Gaviria L, Salcido JP, Guda T, Ong JL. Current trends in dental implants. J Korean Assoc Oral Maxillofac Surg. 2014 Apr;40(2):50-60. PubMed PMID: 24868501.
- Vogel R, Smith-Palmer J, Valentine W. Evaluating the health economic implications and cost-effectiveness of dental implants: a literature review. Int J Oral Maxillofac Implants. 2013 Mar-Apr;28(2):343-56. PubMed PMID: 23527335.
- Prathyusha P, Jyoti S, Kaul RB, Sethi N. Maryland Bridge: An Interim Prosthesis for Tooth Replacement in Adolescents. Int J Clin Pediatr Dent. 2011 May-Aug;4(2):135-8. PubMed PMID: 27672253.
- Rosen PS, Bahat O, Froum SJ, Daftary F, Rosenthal H, Feldman S. Use of a Resin-Bonded Bridge to Replace a Congenitally Missing Lateral Incisor: Treatment of "Intrusion" of Teeth. Compend Contin Educ Dent. 2016 Jul;37(7):482-7. PubMed PMID: 27548400.
- Thompson VP. The Maryland bridge. Phillip J Restaur Zahnmed. 1985;2(5):23-6. PubMed PMID: 3006125.
- Maino GB, Maino G, Dalessandri D, Paganelli C. Orthodontic correction of malpositioned teeth before restorative treatment: efficiency improvement using Temporary Anchorage Devices (TADs). Orthod Fr. 2016 Dec;87(4):367-373. PubMed PMID: 27938652.
- Muller C. Agenesis of lateral incisors: A fresh look at our practice. Int Orthod. 2015 Dec 1;13(4):525-38.
- Al-Amleh B, Lyons K, Swain M. Clinical trials in zirconia: a systematic review. J Oral Rehabil. 2010 Aug;37(8):641-52. PubMed PMID: 20406352.
- Bertolini Mde M, Kempen J, Lourenco EJ, Telles Dde M. The use of CAD/CAM technology to fabricate a custom ceramic implant abutment: a clinical report. J Prosthet Dent. 2014 May;111(5):362-6. PubMed PMID: 24433839.
- Sinha N, Gupta N, Reddy KM, Shastry YM. Versatility of PEEK as a fixed partial denture framework. J Indian Prosthodont Soc. 2017 Jan Mar;17(1):80-83. PubMed PMID: 28216850.
- Daou EE. The zirconia ceramic: strengths and weaknesses. Open Dent J. 2014 Apr 18;8:33-42. PubMed PMID: 24851138.
- Baldissara P, Llukacej A, Ciocca L, Valandro FL, Scotti R. Translucency of zirconia copings made with different CAD/CAM systems. J Prosthet Dent. 2010 Jul;104(1):6-12. PubMed PMID: 20620365.
- Inokoshi M, Pongprueksa P, De Munck J, Zhang F, Vanmeensel K, Minakuchi S, et al. Influence of Light Irradiation Through Zirconia on the Degree of Conversion of Composite Cements. J Adhes Dent. 2016;18(2):161-71. PubMed PMID: 27022645.
- Michalakis KX, Hirayama H, Sfolkos J, Sfolkos K. Light transmission ofposts and cores used for the anterior esthetic region. Int J Periodontics Restorative Dent. 2004 Oct;24(5):462-9. PubMed PMID: 15506027.
- Ozkurt Z, Iseri U, Kazazoglu E. Zirconia ceramic post systems: a literature review and a case report. Dent Mater J. 2010 May;29(3):233-45. PubMed PMID: 20467158.
- Parcina I, Amizic, Baraba A. Esthetic Intracanal Posts. Acta Stomatol Croat. 2016 Jun;50(2):143-150. PubMed PMID: 27789912.
- Reich S. Tooth-colored CAD/CAM monolithic restorations. Int J ComputDent. 2015;18(2):131-46. PubMed PMID: 26110926.
- Wang J, Lin J, Seliger A, Gil M, da Silva JD, Ishhikawa-Nagai S. Color effects of gingiva on cervical regions of all-ceramic crowns. J Esthet Restor Dent. 2013 Aug;25(4):254-62. PubMed PMID: 23910182.
- Wiedhahn K, Fritzsche G, Wiedhahn C, Schenk O. Zirconia crowns - the new standard for single-visit dentistry? Int J Comput Dent. 2016;19:9-26. PubMed PMID: 27027100.
- Anand S, Ebenezar AV, Anand N, Rajkumar K, Mahalaxmi S, Srinivasan N. Microshear bond strength evaluation of surface pretreated zirconia ceramics bonded to dentin. Eur J Dent. 2015 Apr-Jun;9(2):224-7. PubMed PMID: 26038654.
- Strassler HE, Nathanson D. Clinical evaluation of etched porcelain veneers over a period of 18 to 42 months. J Esthet Dent. 1989 Jan;1(1):21-8. Pub- Med PMID: 2635950.