Replantation of Avulsed Mature Permanent Teeth: Emergency Management. Report of Two Cases
Gharbi N*, Masmoudi F, Rekik Y, Baaziz A, Ghedira H, Maatouk F, Abid A
Department of Paediatric Dentisry, Dental Faculty, University of Monastir, Tunisia.
*Corresponding Author
Dr. Nesrine Gharbi,
Department of Paediatric Dentisry,
Dental Faculty, University of Monastir, Tunisia
Tel: 00216 98 38 31 46
E-mail: nesrine.gharbi1809@gmail.com
Received: September 11, 2017; Accepted: October 27, 2017; Published: November 15, 2017
Citation:Gharbi N, Masmoudi F, Rekik Y, Baaziz A, Ghedira H, Maatouk F, Abid A. Replantation of Avulsed Mature Permanent Teeth: Emergency Management. Report of Two
Cases. Int J Dentistry Oral Sci. 2017;4(11):541-545. doi: dx.doi.org/10.19070/2377-8075-17000107
Copyright: Gharbi N©2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The dental avulsion due to a trauma is considered as an emergency. Permanent teeth are more lickely affected.
The best treatment is the replantation when the extra alveolar time and the preservation allow it. However it is about a delicate technique whose success is conditioned by the respect of the protocol and the guidelines.
Aim: The aim of this work is to describe the stages of the tooth replantation through two cases of permanent mature teeth with extra alveolar time less than sixty minuts.
2.Introduction
3.Case Reports
3.1 Case no 1
3.2 Case no 2
4.Discussion
5.Conclusion
6.Acknowledgement
7.References
Keywords
Dental Trauma; Permanent Tooth; Avulsion; Replantation; Splint.
Introduction
Dental trauma occures frequently in children and specially in school age, it represents 18% of all injuries [1-3]. It involves mostly the upper central incisors [4, 5].
It affects boys between 7 and 9 years and girls between 5 and 6 years [6, 7].
Crown fractures and luxations are the most common dental injuries [2, 8] but avulsion is the most serious one. It represents between 8.7% and 30% of all the traumatic injuries [9]. It is the most urgent situation that can be seen in paediatric dentistry department, because the examination and the diagnosis have to beas fast as the treatment plan to enhance the prognosis. The immature permanent teeth are more frequently affected because of the short root and the periodental ligament laxity [10, 11].
The best option for an avulsed tooth is the replantation when the extra oral time and the conservation are appropriate. This procedure is indicated only for permanent teeth, primary teeth are rarely replanted because it may affect the developing permanent tooth below.
Even if there is a risk of frequent complications such as root resorption and pulp necrosis, the replantation has to be attempted because it offers aesthetic and functional advantages [9, 12-14]. However, replantation can be contraindicated in some situations such as general pathologies, important alveolar fractures and tooth affection (caries, root fractures…) [9, 15-17].
It is important to promote the first aid instructions for dental traumas to the public and to be ready to give advices to parents or teachers by telephone at the place of the accident [1]. The instructions are mostly about storage medium because many studies found out that the prognosis is conditioned by the extra alveolar conditions, failure is more frequent if the tooth is conserved in dryness [16, 18, 19]. Actually, after two hours of dryness none periodental ligament cell can survive [16, 20]. Milk and saline could be suitable, saliva is not very recommended because of its septicity [16, 17, 21, 22].
Case Reports
The following case reports describe two treatment plans of avulsed teeth of patients who have shown up at the department of Paediatric Dentistry, University Dental Hospital of Monastir, Tunisia.
F.B, an eleven old male, has shown up with the right upper central incisor (tooth 11) avulsed in an accident at school. The patient’s mother called her dentist to ask about advice so they put the expulsed tooth in saline and rushed to the paediatric dentistry department. Thus, the extra-alveolar time was 30 minutes when they arrived.
Medical and dental history of the patient did not reveal any relevant information.
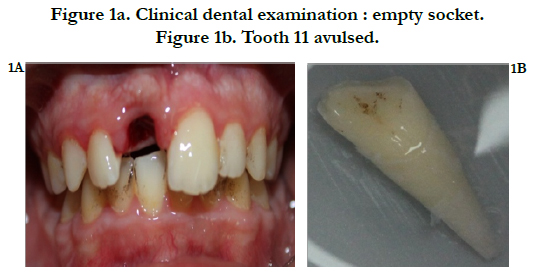
Clinical dental examination showed an upper lip hematoma and a bleeding empty socket (Figure 1a).
The expulsed tooth examination revealed that it is a mature permanent incisor with closed apex with a crown fracture without pulp exposure (Figure1b).
Radiographic examination disclosed an empty upper incisor socket, without any sign of fracture.
The good cooperation and the courage of the patient helped us to start the treatment quickly while the sixty minutes allowing the replantation did not pass by.
The tooth was placed in saline and the alveolar socket was inspected and washed to remove the blood clot.
The adjacent teeth (teeth 12, 21, 22) and the avulsed teeth were prepared with orthophosphoric acid and washed since they will receive the composit to support the splint.
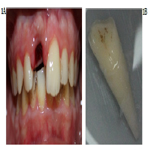
Then the avulsed tooth has been replanted slowly with slight digital pressure, its right position has been verified radiographically (Figure 2a). An orthodontic wire splint has been bonded on the adjacent teeth first and finally on the tooth 11 (Figure 2b).
Figure 2a. X-Ray after replantation.
Figure 2b. The tooth was replanted and stabilized with a flexible wire splint.
We prescribed Antibiotics, anti inflammatories and a mouth rinse and explained the instructions to the patient (soft diet for up to 2 weeks, soft toothbrush use).
We recomended anti-tetnaus vaccine for the patient [24].
Ten days later we recieved the patient again, the gingival healing seemed to be good and the tooth consolidation was satisfying. We proceeded to the root canal treatment with calcium hydroxyde filling.
The splint has been removed 2 weeks later, the crown fracture has been restored with composit and the tooth has been monitored once a week during the first month with frequent calcium hydroxyde renewal, and the root canal filling was done two months later (Figure 3a, b).
Figure 3a. Clinical follow up at 2 months, after replantation and crown restoration.
Figure 3b. Root canal obturation.
The replanted tooth monitoring has been done clinically and radiographically each three months.
A.B, a thirteen years old male, undergoing orthodontic treatment, has shown up after an accident happened in a football game : he fell down and his mate shoelaces hung on the incisors braces. The left upper central incisor (tooth 21) have been dragged out of the tooth socket. The right upper central incisor (tooth 11) have been displaced.
The patient and his coach have shown up at the Paediatric Dentistry department in few minuts so the extra-alveolar time was estimated at 40 minuts, and the avulsed tooth remained in the patient saliva.
Medical history of the patient did not reveal any relevant information, the dental history revealed that the patient is undergoing orthodontic treatment for sixteen months, he has had a root canal treatment on the right upper central incisor three years ago.
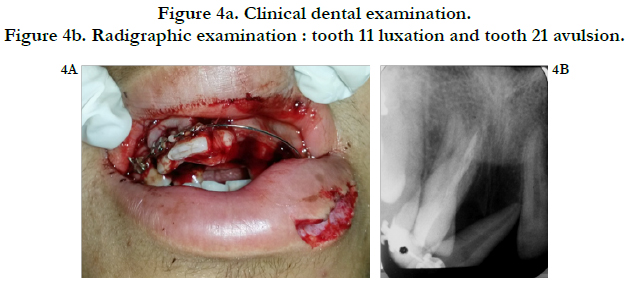
Clinical dental examination showed a lower lip dilaceration, a folded orthodontic wire with the tooth 21 hung on via its bracket, a right upper central incisor displaced in labial direction, a bleeding socket and an upper alveolar mucosa torn (Figure 4a).
Radiographic examination disclosed an empty left upper incisor socket, a right upper diplaced incisor without any sign of fracture (Figure 4b).
Figure 4a. Clinical dental examination.
Figure 4b. Radigraphic examination : tooth 11 luxation and tooth 21 avulsion.
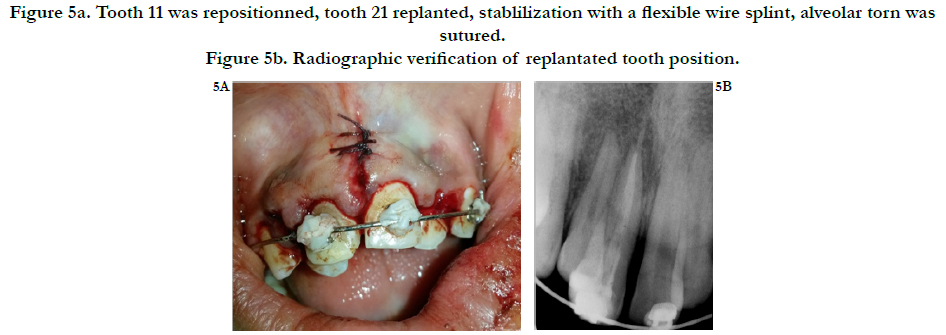
The wire was cut and removed, the avulsed tooth inspected and washed with saline, the displaced tooth (tooth 11) repositioned.
The empty alveolar socket was inspected and washed with saline to remove the blood clot, then the avulsed tooth has been replanted slowly with slight digital pressure, its right position has been verified radiographically (Figure 5 a,b). A new orthodontic wire splint has been bonded on the brackets of the adjacent and the concerned teeth and strenghtned with composit.
Figure 5a. Tooth 11 was repositionned, tooth 21 replanted, stablilization with a flexible wire splint, alveolar torn was
sutured.
Figure 5b. Radiographic verification of replantated tooth position.
The last step was to make sutures on the alveolar mucosa.
We prescripted Antibiotics, anti inflammatories and a mouth rinse and explained the instructions to the patient (soft diet for upto 2 weeks, soft toothbrush use).
Eight days later we saw the patient again, the gingival healing seemed to be good so sutures have been removed, and the teeth consolidation was satisfying. We proceeded to the root canal treatment on the tooth 21 with calcium hydroxyde filling.
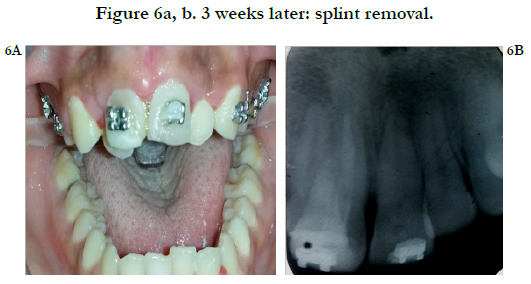
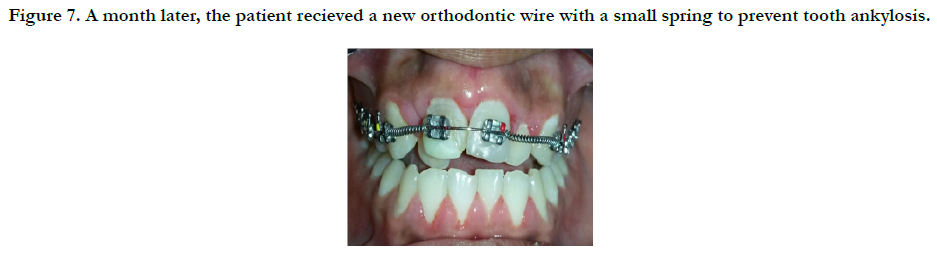
The splint has been removed three weeks later (Figure 6a, b), the tooth was monitored clinically and radiographically once a week during the first month with frequent calcium hydroxyde renewal, then once a month and the patient went back to orthodontics to recieve a new wire (Figure 7).
Figure 7. A month later, the patient recieved a new orthodontic wire with a small spring to prevent tooth ankylosis.
The calcium hydroxyde is renewed when necessary.
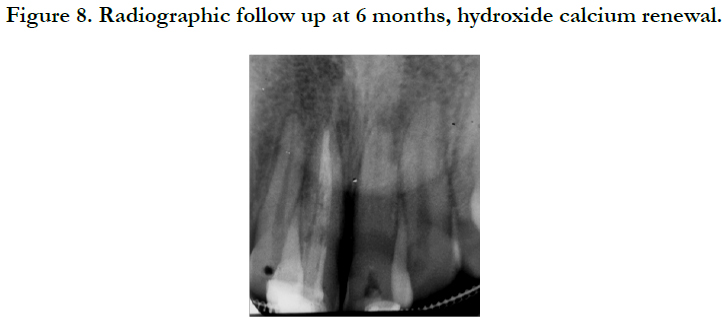
Six months later the radiographic monitoring did not reveal any root or bone resorption (Figure 8).
Discussion
According to IADT guidelines, root canal treatment is recommended for permanent avulsed teeth with closed apex and a root canal filling should be done a month later [1]. The procedure has been a little modified for the second case for important reasons.
The decision was made with orthodontic department agreement, that the root canal will not be filled until the end of the orthodontic treatment and to keep the hydroxyde calcium instead, since the orthodontic forces would increase the risk of root resorption and traumatic teeth are more likely to develop root resorption than untraumatic ones [25, 26]. Indeed, the most frequent reason of replanted teeth loss is the root resorption [27, 28], which is more extensive in children and adolescents due to an extensive bone remodeling during the grow up period [29]. The calcium hydroxyde would decrease the inflammation and stops resorption in 50% of cases [20, 27, 30]. A small spring is also added to prevent tooth ankylosis which is a frequent risk that happens because the surviving periodental cells triggers a repair process through an osteogenesis [25, 31].
In case ankylosis have been diagnosed the unfilled root canal would be helpfull if decoronation is indicated, thus we can avoid a surgical procedure to remove the filling material [26, 32].
Conclusion
Avulsed teeth replantation is a clinical challenge and a delicate procedure that requires a lot of caution. The speed of patient showing up at dental clinic (less than sixty minuts) the storage media and the fast intervention are the prominent factors of the therapeutics success.
The aim of replantation is to keep the tooth on site as long as possible and to postpone the root resoption in order to enjoy its aesthetic and functional characteristics and to preserve the alveolar outline.
Acknowledgement
We would like to thank Pr.Jemmali.B and Pr. Abid.A for their precious advices during the preparation of his work.
References
- Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F, et al. Guidelines for the management of traumatic dental injuries.II. Avulsion of permanent teeth. Dental traumatol. 2007 Jun ;23(3):130-136. PubMed PMID: 17511833.
- Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Oxford : Blackwell Munksgaard ; 2007.
- Petersson EE, Andersson L, Sorensen S. Traumatic oral vs non-oral injuries. Swed Dent J. 1997;21(1-2):55-68. PubMed PMID: 9178450.
- Andreasen JO, Andreasen FM. Text and colourful Atlas of dental trauma. 3rd ed. Porto Alegre: Artmed; 2001.
- Simões FG, Leonardi DP, Baratto FF, Ferreira EL, Fariniuk LF, Sayão SMA. Etiologic factors related to alveoli-dental trauma of patients seen in the dental emergency room of the University Hospital Cajuru1. RSBO. 2004;1(1):50-5.
- Martens L, Rajasekharan S, Cauwels R. Endodontic treatment of traumainduced necrotic immature teeth using a tricalcium silicate-based bioactive cement. A report of three cases with 24-month follow –up. Eur J Paediatr Dent. 2016 Mar;17(1):24-28. PubMed PMID: 26949335.
- Andersson.L, Epidemiology of traumatic dental injuries. J Endod. 2013 Mar;39(3 Suppl):S2-5. PubMed PMID: 23439040.
- Glendor U, Halling A, Andersson L, Eilert-Petersson E. Incidence of traumatic tooth injuries, in children and adolescents in county of Vastmanland, Sweden. Swed Dent J. 1996;20(1-2) :15-28. PubMed PMID: 8738905.
- Skhiri ZS, Abdelmoumen E, Jemaa M, Douki N, Oueslati A, Zokkar N, et al. Traumatic avulsions of permanent teeth. AOS. 2013;266:4-13.
- Naulin-IFI C. Polytrauma of the teeth and the periodontium. Encycl Med chir Odontol. 1998;12.
- Naulin-IFI C. Dental trauma from diagnosis to treatment. Groupe Liaisons; 2005.
- Mc Tigue DJ. Managing traumatic injuries in the yong permanent dentition. In: Pinkham JR, editor. Pediatric Dentistry. Pinkham JR(ed), Saunders, Philadelpia; 1988. 417-418.
- Obry F, Sommerrater J. Dental expulsions. Réalités cliniques. 1992;3:471- 479.
- Andreasen JO. Exarticulations. In: Traumatic injuries of the teeth. 2nd ed. Munksgaard, Copenhagen & Saunders. Philadelphie;1981:203-242.
- Andreasen JO, Andreasen FM. Textbook and color atlas of traumatic injuries to the teeth. Copenhagen, Munsgaard,1994.
- Beslot-Neveu A, David-Béal T, Villette F. Traumatic avulsion of permanent teeth: Management of emergency consultation. Clinic. 2009;30:253-259.
- Trope M. Clinical management of the avulsed tooth. Dent Clin North Am. 1995 Jan;39(1):93-112. PubMed PMID: 7890110.
- Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors. Endod Dent Traumatol. 1995 Apr;11(2):51-89. PubMed PMID: 7641622. PubMed PMID: 7641622.
- Trope M, Hupp JG, Mesaros SV. The role of the socket in the periodontal healing of replanted dog’s teeth stored in Viaspan for extended periods. Endod Dent Traumatol. 1997 Aug;13(4):171-175. PubMed PMID: 9550042.
- Martins WD, Portela V, Westphalen D, Westphalen FH. Tooth replantation after traumatic avulsion: a 27-year follow-up. Dent Traumatol. 2004 Apr;20(2):101-105. PubMed PMID: 15025692.
- Doyle DL, Dumsha TC, Sydiskis RJ. Effect of soaking in Hank’s balanced salt solution or milk on PDL cell viability of dry stored human teeth. Endod Dent Traumatol 1998 Oct;14(5):221-224. PubMed PMID: 9855801.
- Ram D, Cohenca N. Therapeutic protocols for avulsed permanent teeth: review and clinical update. Pediatr Dent. 2004 Jun;26(3):251-255. PubMed PMID: 15185807.
- Martin MP, Pileggi R. A quantitative analysis of Propolis : a promising new storage media following avulsion. Dent Traumatol. 2004 Apr;20(2):85-89. PubMed PMID: 15025690.
- Charland R. Trauma of the permanent anterior teeth. Treizième partie : avulsion. J Ordre des dentistes du Québec. 2008;45:63-69.
- Rocha SR, Moro A, Moresca RC, Sydney G, Fraiz F, Filho FB. Orthodontic treatment in patients with reimplanted teeth after traumatic avulsion: A case report. Dental Press J Orthod. 2010 Aug;15(4):40.e1-10.
- Malmgren O, Malmgren B, Goldson L. Orthodontic approach to traumatized dentition. In: Andreasen JO, Andreasen FM, editors. Text and colourful Atlas of Dental trauma. 3ª ed. Porto Alegre: Artmed; 2001.
- Beslot-Neveu A, David-Béal T, Villette F. Traumatic avulsion of permanent teeth: Management of emergency consultation. Clinic. 2009;30:253-259. [28]. Barrett EJ, Kenny DJ. Survival of avulsed permanent maxillary incisors in children following delayed replantation. Endod Dent Traumatol. 1997 Dec;13(6):269-275. PubMed PMID: 9558508.
- Barrett EJ, Kenny DJ. Avulsed permanent teeth: A review of the literature and treatment guidelines. Endod Dent Traumatol. 1997 Aug;13(4):153–63. PubMED PMID: 9550040.
- Majorana A, Bardellini E, Conti G, Keller E, Pasini S. Root resorption in dental trauma: 45 cases followed for 5 years. Dent Traumatol. 2003 Oct;19(5):262-265. PubMed PMID: 14708650.
- Andreasen JO. Relationship between cell damage in the periodontal ligament after replantation and subsequent development of root resorption. Acta Odontol Scand. 1981;39(1):15-25. PubMed PMID: 6943905.
- Malmgren B, Cvek M, Lundberg M, Frykholm A. Surgical treatment of ankylosed and infrapositioned reimplanted incisors in adolescents. Scand J Dent Res. 1984 Oct;92(5):391-9. PubMed PMID: 6593804.