Difference in Grading of Coronary Stenosis Between Coronary CT Angiography and Invasive Coronary Angiography: Our Experience in an Egyptian Population
Saad Z1*, Donkol RH2, El-Rawy M1, Boughattas S3
1 Cardiology Department, Zagazig University, Egypt.
2 Radiology Department, Cairo University, Egypt.
3 Radiology Department, Aseer Central Hospital, Saudi Arabia.
*Corresponding Author
Zizi Saad, MD,
Professor, Cardiology Department,
Zagazig University, Egypt.
E-mail: zizi5000@hotmail.com
Received: June 08, 2018; Accepted: June 25, 2018; Published: June 27, 2018
Citation: Saad Z, Donkol RH, El-Rawy M, Boughattas S. Difference in Grading of Coronary Stenosis Between Coronary CT Angiography and Invasive Coronary Angiography: Our Experience in an Egyptian Population. Int J Cardiol Res. 2018;5(2):109-115. doi: http://dx.doi.org/10.19070/2470-4563-1800019
Copyright: Saad Z© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: There is some disagreement on grading of coronary artery stenosis (CAS) between CT coronary angiography (CTA) and Invasive Coronary Angiography (ICA). However, there is paucity of data about the factors causing inaccuracy of CTA in grading of CAS. The aim of this study is to identify coronary arterial segment characteristics associated with inaccurate stenosis grading by CTA as defined by Invasive Coronary Angiography (ICA) in an Egyptian population.
Methods: The study was a retrospective single center clinical investigation including 84 patients who were referred for CTA and ICA for various appropriate reasons. We have analyzed the concordance of the stenosis grades on ICA and CTA and their correlation. The difference of grades (DG) between ICA and CTA has been compared across the following variables: involved coronary artery ( left main (LM), left anterior descending (LAD), left circumflex (CX) and right coronary artery (RCA)), anatomical stenosis level (proximal, mid and distal), plaque type (Non-calcified, calcified and mixed) and the ICA stenosis grades (1, 2, 3, 4 and 5).
Results: The linear weighted kappa was к = 0.65 (Confidence Interval: 0.59-0.71) and Spearman’s rs = 0.80 (p < 0.001; Confidence Interval: 0.75-0.85). No association was noted between difference of grades (DG) and involved coronary artery (p = 0.092). A significant association was found between the DG and the affected anatomical segment (p = 0.005) with a significant difference between stenosis of the distal segments versus proximal and middle segments. There was a significant association between DG and plaque type (p = 0.021) with a significant difference between calcified and non-calcified plaques. A significant association between DG and stenosis grade (p < 0.001) was noted but it was considered as clinically irrelevant.
Conclusion: Distal segments stenosis and calcified plaques are associated with higher risk of CTA stenosis grade overestimation.
2.Abbreviations
3.Introduction
4.Material and Methods
4.1 CTA Procedure
4.2 CTA Interpretation
4.3 ICA
4.4 Statistical Analysis
5.Results
5.1 Baseline Demographics
5.2 Sites and characteristics of the stenotic segments
5.3 Concordance of ICA and CTA stenosis grades
5.4 Association between the DG and involved coronary artery
5.5 Association between the DG and the level of CAS
5.6 Association between the DG and plaque type
5.7 Association between the DG and ICA CAS grade
6.Discussion
7.Study Limitations
8.Conclusions
9.References
Keywords
Computed Tomography Coronary Angiography; Coronary Artery Stenosis; Invasive Coronary Angiography.
Abbreviations
CAS: Coronary Artery Stenosis; CTA: CT Coronary Angiography; ICA: Invasive Coronary Angiography; DG: Difference of Grades; LM: Left Main; LAD: Left Anterior Descending; CX: Circumflex; RCA: Right Coronary Artery; CAD: Coronary Artery Disease; NPV: Negative Predictive Value; ECG: Electrocardiographic; MPR: Multiplanar Reformations; cMMR: Curved Multiplanar Reformations; MIP: Maximum Intensity Projections; UE: Underestimation; OE: Overestimation; FP: False Positive; FN: False Negative; OR: Odd Ratios; PPV: Positive Predictive Value; SCCT: Society of Cardiovascular Computed Tomography.
Introduction
Coronary artery disease (CAD) is one of the major causes of mortality and morbidity in the 21st century [1-3]. Reliable and accurate diagnosis of CAD is a crucial part in management and prevention of major cardiac events. While invasive coronary angiography (ICA) is still the "gold standard" imaging test for the anatomical assessment of CAD, Coronary CT angiography (CTA) has increasingly become a reliable noninvasive alternative and has proven clinically useful for excluding obstructive CAD due to its high sensitivity and negative predictive value (NPV) [4-8]. In comparison to conventional functional testing, CTA has been shown to have a higher diagnostic accuracy and results in better cardiovascular outcomes [9]. While disagreement on grading of individual coronary arterial stenosis (CAS) severity is common between CTA and ICA [10], there is paucity of data on factors associated with CTA inaccuracy [11]. The aim of this study is to identify coronary arterial segment characteristics associated with inaccurate CTA stenosis grading as defined by ICA in an Egyptian population.
Material and Methods
This study was a single centre retrospective and the protocol was approved by institutional review board, with written informed consent from all patients. From mid- March 2016 until February 2017 we included 84 patients who were referred to our hospital for CTA and ICA for various appropriate reasons. Inclusion criteria were negative or equivocal stress tests, intermediate pretest probability for CAD (9-15 points) according to the scoring method of Morise et al., [12]. Exclusion criteria were renal insufficiency, known allergy to iodinated contrast material, unstable clinical condition. CTA scans with technical errors or artifacts were excluded from the study. All ICA were performed within a maximum delay of 14 days after CTA.
All patients were examined using a 128 multi-detector CT system (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany). Image acquisition techniques included either traditional retrospective electrocardiographic (ECG)-gating with default use of ECG-dependent tube current modulation or prospectively ECG-triggered high- pitch spiral acquisitions. Tube potential was either 100 or 125 kV according to body mass index (125 kV if body mass index > 25 kg/m2, and100 kV if body mass index < 25 kg/m2).
In the absence of contraindications, patients received 0.5 mg of sublingual nitroglycerin (Nitroquick; Ethex KV Pharmaceuticals, Bridgeton, Mo) immediately before the study for coronary vasodilatation.
In patients undergoing prospectively ECG-triggered highpitch spiral acquisitions, beta-blockers (5-20 mg intravenous metoprolol tartrate [Lopressor, Novartis, East Hanover, NJ]) were administered intravenously for heart rates higher than 65 beats per minute. Contrast timing was tested by an initial bolus-timing scan using 15 cc of iodinated contrast material iohexol [Omnipaque; GE Healthcare, Chalfont St Giles, England], 350 mg of iodine per milliliter, followed by a 30 cc saline chaser. The scan time was adjusted by adding 3 seconds after the peak of time-enhancement curve of the ascending aorta to ensure maximum opacification of the coronary arteries. The contrast-enhanced scan was obtained using a volume of 60 to 100 cc of contrast individually adapted to the selected table feed and scan range followed by a 50 cc saline chaser. Both contrast and saline were injected at a rate of 6 mL/sec by using a dual-syringe injector (Stellant D; Medrad, Indianola, Pa).
Images of the non-contrast-enhanced scan and enhanced CTA data sets were transferred to an image processing workstation (Syngo MMWP VE 36A, Siemens) to be analyzed for coronary calcium scoring and angiography. The images were jointly interpreted by two experienced readers (cardiologist and radiologist) Level III with board certification. If severe calcification or imaging artifacts made a valid assessment impossible, the examination was excluded from the study. Images were reconstructed in mid-diastole with individually optimized the reconstruction window level and width. Additional image reconstructions were performed in endsystole if required. The coronary artery tree was evaluated on a segmental basis in accordance with the guidelines of the society of cardiovascular computed tomography 18-segment model [13], by inspection of the axial images, multiplanar reformations (MPR), curved multiplanar reformations (cMMR) along the vessel centerline, 3 perpendicular sets of thin-slab maximum intensity projections (MIP) orientated along the heart axis. Grading of CAS was based mainly on visual estimation. Each segment was interpreted visually and the severity of lumen narrowing was scored, then rated semi-quantitatively into 5 groups: normal (Absence of plaque/no luminal stenosis) Minimal (Plaque with < 25% stenosis), Mild (25% - 49% stenosis), Moderate (50 - 69% stenosis), Severe (70% - 99% stenosis) and occluded [13].
ICA was performed by interventional cardiologist in the cardiac cath lab using the Judkins approach via the femoral artery acquiring standardized projections [14]. Coronary stenosis were analyzed using a well validated commercially available software package (Xcelera , Phillips Xper FD, Phillips Medical Systems Nederland B.V The Netherlands). ICA images where analyzed using a dedicated software ( Xcelera Cardiology information management system). Visual estimation was applied and the qualitative analysis was based on the angiographic projection showing the most severe narrowing. A coronary stenosis was defined as significant based on visual inspection when the degree of stenosis was more than 50%. Analysis of coronary artery lesions was performed by interventional cardiologist who was unaware of CT results, except for the information that would have an immediate effect on the interventional procedure (e.g. presence of coronary artery anomalies). Each coronary artery was visualized by multiple projections and assessed for diameter reduction.
A statistical analysis was performed by using the NCSS statistical software (Version 11). P < 0.05 was considered as statistically significant.
If the individual CAS had the same grade on ICA and CTA, the result was classified as concordant. The concordance of ICA and CTA for grading of CAS was evaluated using linear weighted kappa (к) statistics and their correlation assessed by the Spearman’s rank correlations coefficient rs. The difference of grades (DG) between ICA and CTA (DG=ICA grade-CTA grade for the same segment) has been compared across the following variables: involved coronary artery (LM, LAD, LCx and RCA), anatomical stenosis level (proximal, mid and distal), plaque type (Non-calcified, calcified and mixed) and the ICA stenosis grade (1, 2, 3, 4 and 5) using Kruskal-Wallis H test with correction for tied ranks; post-hoc analysis has been performed with Dunn’s test. While we used Kruskal-Wallis H test to compare mean ranks, the mean DG is also presented herein for each factor level for illustrative purpose.
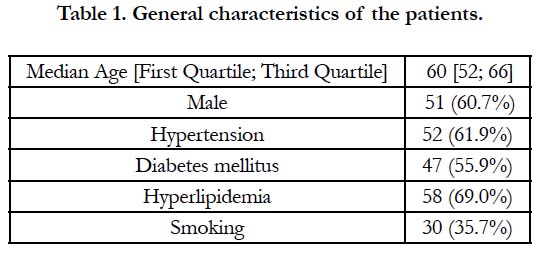
Baseline patients characteristics are shown in Table 1. The median age was 60 years (IQR, 52-66 years). The patients were 51 men, 33 women, 52 had hypertension (62%), 47 diabetes mellitus (56%), 58 hyperlipidemia (69%) and 30 are smokers (36%).
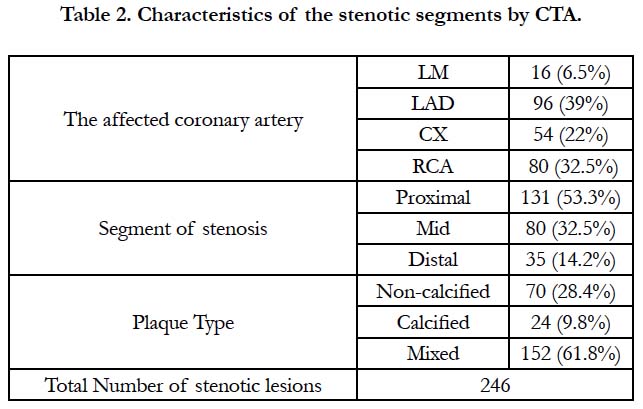
Table 2 presents the CTA findings of the whole 246 stenotic segments regarding the involved coronary artery, the anatomical stenotic segment and the plaque type. Numbers of CAS segments in left main (LM), left anterior descending (LAD), left circumflex (CX) and right coronary artery (RCA) were respectively 16 (6.5%), 96 (39%), 54 (22%) and 80 (32.5%).
Levels of CAS were: 131 proximal (53.3%), 80 mid (32.5%) and 35 distal segments (14.2%). The most frequent type of plaque was mixed 152 (61.8%), followed by non- calcified 70 (28.4%) and calcified (9.8%).
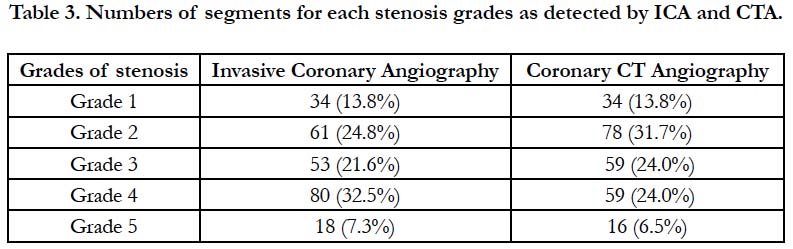
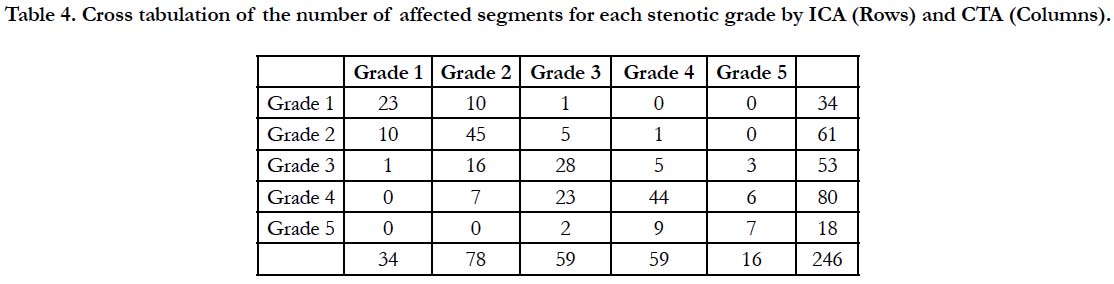
A comparison between numbers of affected segments for each stenosis grades between CTA and ICA is presented in Table 3. The gross tabulation of the number of the affected segments for each stenotic grade by ICA and CTA is presented in Table 4 for the total 246 stenotic segments.
Table 4. Cross tabulation of the number of affected segments for each stenotic grade by ICA (Rows) and CTA (Columns).
The concordance of CTA and ICA in CAS grading was fair with a linear weighted kappa к = 0.65 (Confidence Interval: 0.59-0.71). A significant positive correlation was observed between CTA and ICA CAS grades: Spearman’s rs = 0.80 (p < 0.001; Confidence Interval: 0.75-0.85).
Concordance of grades was noted in 147 segments (59.8 %); CTA underestimation was noted more frequently than overestimation, respectively 68 (27.6%) and 31 segments (12.6%). In 231 segments (94%) the DG was within the range [-1 +1], and in no case the DG was superior to 2.
False positive and false negative results by CTA, in comparison with ICA (significant lesion defined by grade ≥ 3), were noted in, respectively, 7 (2.8%) and 24 segments (9.8%).
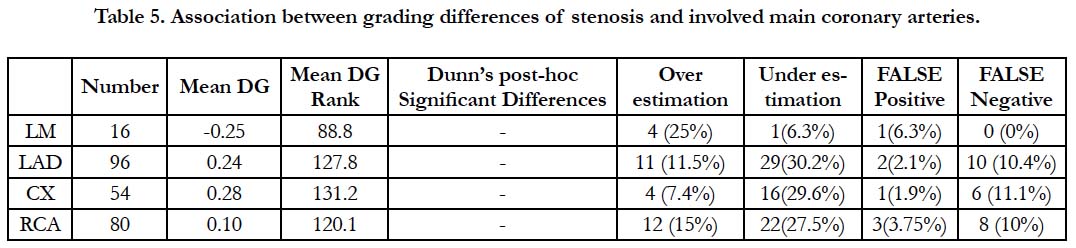
Table 5 shows that there is no association between DG and involved coronary artery (H = 6.44, df = 3, p = 0.092). Percentages ranging among the four arteries (LM, LAD, LCX and RCA) for overestimation, underestimation, false positive and false negative were respectively [7.4%-25%], [6.3%-30.2%], [1.9%-6.3%] and [0%-11.1%].
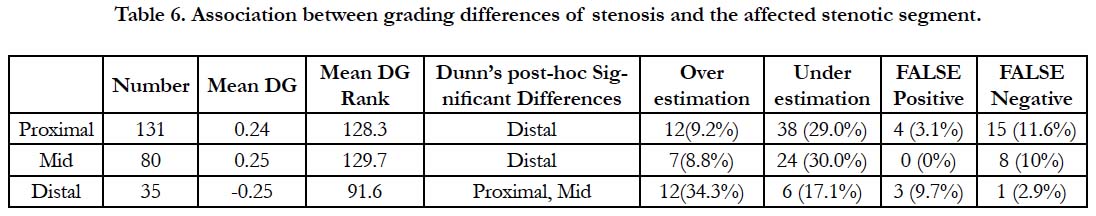
A significant association was found between the DG and the affected anatomical segment (H = 10.65, df = 2, p = 0.005). Posthoc analysis revealed significant difference between stenoses of the distal segments versus proximal and middle segments (Table 6). The percentages of overestimation, underestimation, false positive and false negative were 9%, 29.4%, 1.9% and 10.9% respectively in the proximal/mid group, and 34.3%, 17.1%,9.7% and 2.9% in the distal group.
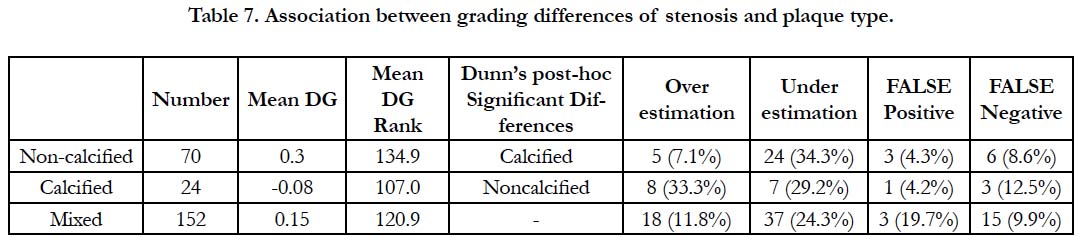
There was a significant association between DG and plaque type (H = 7.68, df = 2, p = 0.021). Post-hoc analysis showed significant difference between calcified and non-calcified plaques (Table 7). The percentages of overestimation, underestimation, false positive and false negative were 7.1%, 34.3%, 4.3% and 8.6% respectively in the non- calcified plaques group, and 33.3%, 29.2%, 4.2% and 12.5% in the calcified plaques group.
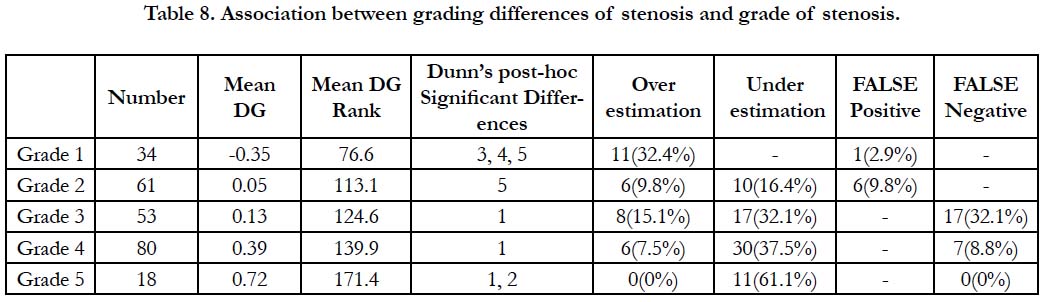
Table 8 shows that there was a significant association between DG and stenosis grade (H=36.96, df=4, p < 0.001). Post-hoc Dunn’s analysis revealed significant differences only in pairs involving at least one of extreme grades 1 and 5; no significant difference was noted between the intermediate grades 3, 4 and 5.
Discussion
Although the diagnostic capability of CTA for determining the degree of CAS has been largely established by several prospective trials [15], few data are available on predicting factors of CTA inaccuracy [11]. Our aim was to identify the angiographic characteristics of the stenotic segments that are predictive of CTA grading differences with ICA, in an Egyptian population. Considering the high predictive value of negative CTA to exclude coronary artery obstruction and the difficulties to characterize all negative segments, we included in this study only the positive results of CTA. While we considered ICA grading of CAS as reference, it is worthy to note that ICA is inherently limited by the number of projections and foreshortening of vessels with imperfections in displaying coronary anatomy accurately especially for noncircular lesions geometries [10].
We have studied the association of the variable DG with four characteristics of the stenotic segment, i.e. the involved coronary artery (LM, LAD, CX and RCA), the anatomical stenosis level (Proximal, Mid and Distal), the plaque characteristics (Noncalcified, Calcified and Mixed) and the ICA stenosis grade (Grades 1,2,3,4 and 5). In our site reading departments, grading was based on visual estimation which is the most commonly performed coronary lumen assessment in clinical practice, both for coronary CTA as well as for ICA because of its easiness and speed [10].
Global results of the current study showed fair kappa concordance and a good significant positive correlation between CTA and ICA in CAS scores.
In this study, underestimation (UE) was more frequent than the overestimation (OE ) and false positive (FP) was more frequent than false negative (FN). This seems to be in opposition to the results of most of previous studies [16-19]. Nevertheless some series reported either that CTA did not overestimate stenosis for the CorE-64 study [20] or even CTA more frequently underestimate stenosis [21]. In the series of Hong [21], who has evaluated the ability of CTA (on a per-patient basis) to aid in the therapeutic decision making process in symptomatic patients, revascularization was performed in 285 (29%) of the 969 patients not indicated for revascularization by CTA, among them 80 because of stenosis underestimation (8.3%). Of the 877 patients indicated for revascularization by CTA (> 70% luminal narrowing of at least one segment), 277 patients (32%) did not undergo revascularization among them 44 because of stenosis overestimation (5%). Observations from this study demonstrate that DG was not associated with the involved coronary artery. In the series of Yan the segment location per major vessel categories was not independently associated with segment-level CTA inaccuracies; taking the LM as reference, the odd ratios (OR) for LCX, RCA and LAD were all inferior to 1 for FN diagnosis and superior to 1 for FP without reaching the level of significant difference. The present findings indicate that distal stenoses confer an increased risk for CTA overestimation in comparison to proximal and mid level stenoses with more OE and FP and less UE and FN. This result is concordant with the results of Hong [21] who reported that disagreement between CTA and ICA is accentuated when examining small-sized vessels (i.e., sidebranch/ distal segments of coronary arteries), manifesting as lower positive predictive value (PPV) with minimal effect on the NPV. Indeed, when CTA angiography indicates revascularization, disagreement was noted in 54%, 53% and 72% for, respectively, proximal, mid and distal segments. When CCTA indicates no need for revascularization, disagreements were seen in only 4%, 9% and 2%. Similar results have been reported by Cademartiri [22], but the difference between proximal and distal segments was strongly dependant on the level of intra-coronary enhancement. For low enhancement (defined as vascular attenuation less than the median attenuation of 326 HU), the PPV was 77% for proximal segments and 55% for distal segments while the PPVs were closer for high enhancement (89% and 85% respectively). At the difference of these results, in the series of Yan [11], smaller luminal caliber conferred increased odds for both CTA false positive (OR: 0.49/mm increment) and false negative (OR: 0.40/ mm increment).
Interpretation of CTA in the presence of coronary artery calcification is hampered by blooming and beam hardening artifacts, which make it difficult to accurately assess the degree of luminal narrowing by coronary CTA [19, 23]. Approximately 50-70% of all coronary artery plaques are calcified in patients with asymptomatic or suspected CAD [23]. Comparison between series is complicated by differences in the definition of plaque groups and several series reported same or better performance in patients with high calcium scores compared to patients with less calcification while others found poorer performance in the former [24]. Some series define the groups based on the Agatston calcium score [24], while others use a per-segment based analysis: partition according to the percentage of the stenotic segment diameter occupied by the calcification [23] or cross-sectional arc [19], dichotomous partition calcified/non-calcified [11]. Another difficulty arises from the fact that the PPV and NPV are influenced by the prevalence of disease which itself depends on the degree of plaque calcification [19, 25].
In the current study, we followed the society of cardiovascular computed tomography (SCCT) guideline recommending that plaque type should be described as calcified, non-calcified, or mixed [13]. We found a significant difference only between the calcified and non-calcified plaques groups. While calcified plaques presented comparable risks for both OE (33.3%) and UE (29.2%), the non-calcified plaques presented mainly a risk for UE (34.3%) and less risk for OE (7.1%). The DG between these two groups was related essentially to a more than fourfold higher risk of OE in the calcified plaques group (33.3% vs 7.1%). In the series of Vavere (non-calcified, mild/moderate/severe according to the diameter occupied by the plaque), OE and UE were, respectively, 1% and 3% in absence of calcification, 5% and 6% for mild calcification, 12% and 8% for moderate calcification, and 17% and 8% for severe calcification [19]; if we consider that the last group is comparable to the "calcified plaque group" in our series, these results corroborate ours in the sense that OE and UE both occur for the severe calcification/calcified plaque. Palumbo [26] reported that a high calcium score leads to a mild reduction in sensitivity and a more obvious decrease in specificity on a per-segment basis and we fully share his conclusion: "this finding has not been extensively investigated and confirmed with 64-slice CTA". However, in the series of Zhang [23], for severe calcification, only OE has been seen in the severely calcified plaque. OE and UE were, respectively, 3% and 2% for small plaque, 9% and 0% for moderate plaque, and 33% and 0% for large plaque. Similarly, in the study of Yan [11] the presence of calcification independently increased the odds for FP diagnosis (OR: 10.16) and conferred reduced odds for FN diagnosis (OR: 0.50); on the contrary, obstructive disease in a segment without calcification is more likely to be missed (OR: 2.01). While we have found a significant association between DG and ICA grade, we are not considering this result as clinically relevant. Indeed, posthoc analysis revealed differences only in pairs involving at least one of the extreme grades 1 and 5 and no significant difference was noted between the intermediate grades 3, 4 and 5. This is likely related to the unidirectional nature of CTA discordances with ICA grades 1 and 5: only OE are possible for CTA grade 1 and only UE are possible for CTA grade 5. This conclusion is corroborated by the results of Raff [17] who noted the absence of significant correlation between the difference in the percentage of stenosis and the stenosis severity.
To the best our knowledge, this is the first study focusing specifically on the identification of predictive factors for DG in an Egyptian population, while previous studies dealt with predictors for inaccuracy of CTA [11, 27, 28]; this has the potential benefit of reduction of the bias related to variations in CAD prevalence. Another important strength of our study resides in its reliance on visual estimation which is the common quantification of CAS method in the "real world" of imaging practice of radiologists and cardiologists in site readings [10, 23].
Study Limitations
Our study had several limitations. First this is a single tertiary cardiac center retrospective study. Second, the study didn’t look at patient characteristics and other angiographic findings, like vein crossing, motion artifact or segment tortuosity that might interfere with image quality and therefore may make CTA grading inaccurate. Third, the sample size of the study group was relatively small with possibly limited statistical power. A larger sample size study could especially reveal some important characteristics of the mixed plaque group which the not only the most prevalent group is but also the most associated one with greater levels of stenosis severity [25].
Conclusions
This study has identified that in an Egyptian population the anatomical segment of stenosis and the plaque type are the main imaging predictors for differences of grading between CTA and ICA. Distal segments stenosis and calcified plaques are associated with higher risk of stenosis overestimation on CTA. These differences should be taken in account when interpreting the results of CTA in patients suspected of CAD.
References
- Laslett LJ, Alagona Jr P, Clark III BA, Drozda Jr JP, Saldivar F, Wilson SR, et al. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the American College of Cardiology. J Am Coll Cardiol. 2012 Dec 25;60(25 Suppl):S1-49. doi: 10.1016/j.jacc.2012.11.002. PubMed PMID: 23257320.
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014 Jan 21;129(3):e28-e292. doi: 10.1161/01.cir.0000441139.02102.80. PubMed PMID: 24352519.
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017 Mar 7;135(10):e146-e603. doi: 10.1161/CIR.0000000000000485. PubMed PMID: 28122885.
- Doh JH, Koo BK, Nam CW, Kim JH, Min JK, Nakazato R, et al. Diagnostic value of coronary CT angiography in comparison with invasive coronary angiography and intravascular ultrasound in patients with intermediate coronary artery stenosis: results from the prospective multicentre FIGURE-OUT (Functional Imaging criteria for GUiding REview of invasive coronary angiOgraphy, intravascular Ultrasound, and coronary computed Tomographic angiography) study. Eur Heart J Cardiovasc Imaging. 2014 Aug;15(8):870-7. doi: 10.1093/ehjci/jeu009. PubMed PMID: 24513881.
- Gorenoi V, Schönermark MP, Hagen A. CT coronary angiography vs. invasive coronary angiography in CHD. GMS Health Technol Assess. 2012;8:Doc02. doi: 10.3205/hta000100. PubMed PMID: 22536300.
- Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008 Nov 18;52(21):1724-32. doi: 10.1016/j. jacc.2008.07.031. PubMed PMID: 19007693.
- Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, et al. ACCF/ ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed topographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol. 2010 Jun 8;55(23):2663-99. doi: 10.1016/j.jacc.2009.11.013. PubMed PMID: 20513611.
- von Ballmoos MW, Haring B, Juillerat P, Alkadhi H. Meta-analysis: diagnostic performance of low-radiation-dose coronary computed tomography angiography. Ann Intern Med. 2011 Mar 15;154(6):413-20. doi: 10.7326/0003-4819-154-6-201103150-00007. PubMed PMID: 21403076.
- Nielsen LH, Ortner N, Nørgaard BL, Achenbach S, Leipsic J, Abdulla J. The diagnostic accuracy and outcomes after coronary computed tomography angiography vs. conventional functional testing in patients with stable angina pectoris: a systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging. 2014 Sep;15(9):961-71. doi: 10.1093/ehjci/jeu027. PubMed PMID: 24618659.
- Arbab-Zadeh A, Hoe J. Quantification of coronary arterial stenoses by multidetector CT angiography in comparison with conventional angiography: methods, caveats, and implications. JACC Cardiovasc Imaging. 2011 Feb;4(2):191-202. doi: 10.1016/j.jcmg.2010.10.011. PubMed PMID: 21329905.
- Yan RT, Miller JM, Rochitte CE, Dewey M, Niinuma H, Clouse ME, et al. Predictors of inaccurate coronary arterial stenosis assessment by CT angiography. JACC Cardiovasc Imaging. 2013 Sep;6(9):963-72. doi: 10.1016/j. jcmg.2013.02.011. PubMed PMID: 23932641.
- Morise A, Evans M, Jalisi F, Shetty R, Stauffer M. A pretest prognostic score to assess patients undergoing exercise or pharmacological stress testing. Heart. 2007 Feb 1;93(2):200-4. PubMed PMID: 17228070.
- Wu FZ, Wu MT. 2014 SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2015 Mar-Apr;9(2):e3. doi: 10.1016/j.jcct.2015.01.003. PubMed PMID: 25708015.
- Judkins MP. Selective coronary arteriography: part I: a percutaneous transfemoral technic. Radiology. 1967 Nov;89(5):815-24. PubMed PMID: 6048074.
- Janjua SA, Hoffmann U. New insights from major prospective cohort studies with cardiac CT. Curr Cardiol Rep. 2015;17(4):19. doi: 10.1007/ s11886-015-0571-2. PubMed PMID: 25725603.
- Madhok R, Aggarwal A. Comparison of 128-slice dual source CT coronary angiography with invasive coronary angiography. J Clin Diagn Res. 2014 Jun;8(6):RC08-11. doi: 10.7860/JCDR/2014/9568.4514. PubMed PMID: 25121042.
- Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005 Aug 2;46(3):552-7. PubMed PMID: 16053973.
- Ong TK, Chin SP, Liew CK, Chan WL, Seyfarth MT, Liew HB, et al. Accuracy of 64-row multidetector computed tomography in detecting coronary artery disease in 134 symptomatic patients: influence of calcification. Am Heart J. 2006 Jun;151(6):1323.e1-6. PubMed PMID: 16781246.
- Vavere AL, Arbab-Zadeh A, Miller JM, Rochitte CE, Dewey M, Niinuma H, et al. Accuracy of 64-slice computed tomography in assessing coronary artery stenoses in segments with mild, moderate, or extensive calcification: a subanalysis of the CORE-64 trial. J Am Coll Cardiol 2009;53 Suppl:1036-248.
- Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008 Nov 27;359(22):2324-36. doi: 10.1056/NEJMoa0806576. PubMed PMID: 19038879.
- Hong SJ, Her AY, Suh Y, Won H, Cho DK, Cho YH, et al. Coronary Computed Tomographic Angiography Does Not Accurately Predict the Need of Coronary Revascularization in Patients with Stable Angina. Yonsei Med J. 2016 Sep;57(5):1079-86. doi: 10.3349/ymj.2016.57.5.1079. PubMed PMID: 27401637.
- Cademartiri F, Maffei E, Palumbo AA, Malagò R, La Grutta L, Meiijboom WB, et al. Influence of intra-coronary enhancement on diagnostic accuracy with 64-slice CT coronary angiography. Eur Radiol. 2008 Mar;18(3):576-83. PubMed PMID: 17934740.
- Zhang S, Levin DC, Halpern EJ, Fischman D, Savage M, Walinsky P. Accuracy of MDCT in assessing the degree of stenosis caused by calcified coronary artery plaques. AJR Am J Roentgenol. 2008 Dec;191(6):1676-83. doi: 10.2214/AJR.07.4026. PubMed PMID: 19020235.
- Arbab-Zadeh A, Miller JM, Rochitte CE, Dewey M, Niinuma H, Gottlieb I, et al. Diagnostic accuracy of computed tomography coronary angiography according to pre-test probability of coronary artery disease and severity of coronary arterial calcification: the CORE-64 (Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography) international multicenter study. J Am Coll Cardiol. 2012 Jan 24;59(4):379-87. doi: 10.1016/j.jacc.2011.06.079. PubMed PMID: 22261160.
- Min JK, Edwardes M, Lin FY, Labounty T, Weinsaft JW, Choi JH, et al. Relationship of coronary artery plaque composition to coronary artery stenosis severity: results from the prospective multicenter ACCURACY trial. Atherosclerosis. 2011 Dec;219(2):573-8. doi: 10.1016/j.atherosclerosis. 2011.05.032. PubMed PMID: 21696739.
- Palumbo AA, Maffei E, Martini C, Tarantini G, Di Tanna GL, Berti E, et al. Coronary calcium score as gatekeeper for 64-slice computed tomography coronary angiography in patients with chest pain: per-segment and per-patient analysis. Eur Radiol. 2009 Sep;19(9):2127-35. doi: 10.1007/s00330- 009-1398-2. PubMed PMID: 19387651.
- Dewey M, Vavere AL, Arbab-Zadeh A, Miller JM, Sara L, Cox C, et al. Patient characteristics as predictors of image quality and diagnostic accuracy of MDCT compared with conventional coronary angiography for detecting coronary artery stenoses: CORE-64 Multicenter International Trial. AJR Am J Roentgenol. 2010 Jan;194(1):93-102. doi: 10.2214/AJR.09.2833. PubMed PMID: 20028910.
- Meijboom WB, Meijs MF, Schuijf JD, Cramer MJ, Mollet NR, van Mieghem CA, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008 Dec 16;52(25):2135-44. doi: 10.1016/j.jacc.2008.08.058. PubMed PMID: 19095130.