Evaluation of Fever Management Practices in Rural India
Jalpa B Manjariya1, Rima Shah2*, Ankita M Miruliya3
1 Medical Officer at primary health centre, Botad, Gujarat, India.
2 Assistant Professor, Department of Pharmacology, GMERS Medical College and General Hospital, Gandhinagar, Gujarat, India.
3 Junior Resident, GMERS Medical College and General Hospital, Gandhinagar, Gujarat, India.
*Corresponding Author
Dr. Rima Shah,
Assistant Professor, Department of Pharmacology, GMERS Medical College and General Hospital, Gandhinagar, Gujarat, India.
Tel: +919913175808
E-mail: rimashah142@gmail.com
Received: May 15, 2020; Accepted: July 29, 2020; Published: July 31, 2020
Citation: Jalpa B Manjariya, Rima Shah, Ankita M Miruliya. Evaluation of Fever Management Practices in Rural India. Int J Clin Pharmacol Toxicol. 2020;9(1):323-330. doi: dx.doi.org/10.19070/2167-910X-2000051
Copyright: Rima Shah© 2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Precision regarding treatment of fever is reportedly low among the rural regions of India, leading to its irrational
management. This study evaluates fever management practices followed by physicians at primary health centre and
correlate this with standard fever management guidelines.
Methods: One hundred and forty patients admitted to hospital with fever were enrolled in the study. Patient’s demographic
profile and presenting symptoms were precisely studied along with their vital parameters. Patients were divided into two
groups (A&B), with and without treated as per standard guidelines. Duration of illness, treatment with various drugs and
clinical investigation of patients with fever were analysed statistically as outcome analysis.
Results: Majority of patients (47.86 %) belonged to age of 18-30 years. Symptoms related to Upper respiratory tract infection
(URTI), such as cough and rhinorrhoea, were the most common symptoms (104 patients, 74.28%). Most common clinical
diagnosis was viral URTI in both the groups followed by enteric fever, acute gastroenteritis etc. No statistical significance
observed in duration of illness in both groups. All the patients of group A were advised laboratory investigations to confirm
the diagnosis as per the standard management protocol. Most frequently ordered investigations were complete blood count
and peripheral smear for malarial parasite. Average number of drugs prescribed was 2.94 and 4.03 in group A and B (p value
0.001). 8.33% and 18.75% were belonged to category of more than 5 drugs per prescription (polypharmacy) in group A and
B respectively. Amoxicillin and Azithromycin were the most preferentially prescribed antibiotics. 90% and 20% of antibiotics
were prescribed appropriately (P=0.01) as per guidelines in group A and B respectively. Co-prescription of famotidine, pantoprazole
etc was significantly high in group B (p<0.05).
Conclusion: A large number of patients were prescribed with antibiotics without accurate confirmation of bacterial infections
which was contradictory to standard guidelines of fever management practice. Hence increased awareness for rational
fever management is desirable among clinical practitioners in rural India.
2.Introduction
3.Methodology
4.Results
5.Discussion
6.Conclusion
7.References
Keywords
Fever; Management Principles; Symptomatology; Clinical Examination; Laboratory Investigations for Fever; Antibiotics Usage.
Introduction
Fever is considered as one of the most common clinical reasons
for physicians, accounting for about one-third of all presenting
conditions in adult population [1, 2]. Fever, an elevation in core
body temperature above the daily range (98.6ºf) for an individual,
is a characteristic feature of most infections but is also found in a
number of non-infectious diseases such as autoimmune and carcinoma.
Fever is a physiological mechanism with beneficial effects in fighting
infection and it is usually not associated with long-term neurologic
complications. The only purpose for treating fever must be
to relieve the discomfort [3]. Concerns of patients about serious
causes of fever (ie, severe bacterial infections) and misconceptions
about fever as a sufficient trigger of brain damage have led
to the spreading of ‘fever-phobia’. Several studies have reported a
high percentage of adult population consuming antipyretics and
antibiotics even when there is minimal or no fever, with wrong
dosages or with insufficient intervals between the doses [3, 4].
The inappropriate management of fever with irrational use of
antipyretics or antibiotics may delay the diagnosis and increase the
risk of overdose or significantly contributing to antibiotic resistance.
Moreover, other factors may increase drug toxicity such as
the alternate/combined use of two antipyretics or combination
of antibiotics, the use of other formulations with other medicaments,
and the administration of these drugs in the presence of
contraindicated underlying diseases. Finally, overtreatment may
have a significant economic impact in low-middle income and
high income countries. Antipyretics and antibiotics are most preferred
self-method of managing fever and there has been an increase
in this preference over the past two decades from 67% to
more than 90% (91% to 95%) [4].
Fever can pose diagnostic and therapeutic challenge to the health
workers, particularly in limited resource settings. A number of
viruses, bacteria, protozoa and rickettsia can cause fever [5, 6].
The non-specificity of symptoms and signs and lack of availability
of accurate diagnostics not only test the clinical mettle of even
astute physicians but often leads to irrational use of antibiotics
and antimalarials. Some fever syndromes have a more clear localization
to skin and soft tissue (abscess or cellulitis), meninges or
neural tissue (headache, neck-stiffness, altered sensorium with or
without focal neurological signs), respiratory tract (cough, breathlessness),
or urinary tract (dysuria, haematuria). These syndromes
have better developed guidelines for their management. On the
other hand, acute unidentified fever syndromes (suchas feverrash,
fever-myalgia, fever-arthralgia, fever-hemorrhageand fever
jaundice) haveoverlapping etiologies, which makes their diagnosis
and management even more challenging [7, 8].
In order to rationalise and standardise the symptomatic management
of fever in adult population, national health agencies,
WHO and scientific societies have produced and disseminated
clinical guidelines. It has been demonstrated that patients do not
fully comply with these recommendations of use of prescription
drugs, as they used to employ traditional physical means and
administer antipyretics and antibiotics with inappropriate indications
and posology. Moreover, important discrepancies have been
reported between the practices of healthcare professionals and
the recommendations of guidelines [4]. Considering the abovementioned
parameters in treatment of fever, this study has been
designed with aim of evaluating management practices for fever
in rural India.
Methodology
This was a cross sectional observational study conducted in two
primary health care centres of the western India to know the
management principles of fever being followed at rural level. The
study protocol was approved by the institutional ethics committee
and written informed consent was obtained from all patients
before enrolling them for the study.
All the patients presented to the primary health care centre of ≥
18 years and of any gender, having chief compliant of fever for
at least one day with any other associated symptoms were enrolled
for the study. Patients with delirium, serious patients requiring referral
to higher centrefacility immediately and those requiring intensive care unit admissions were excluded from the study.
Considering the prevalence of fever of unidentified origin in Indian
populations around 80% [9, 10], sample size is 126 at 7%
precision and 95% confidence interval for this study. Few patients
may drop out or lost to follow up (10%) in the entire duration of
the study, so 140 patients were enrolled for the study. Considering
the dropout total 140 patients were enrolled for the defined time
duration of 6 months (November-April 2019).
All the patients fulfilling inclusion-exclusion criteria were interviewed
by the principle investigator. Demographic details, clinical
examination, history of past and family illnesses, drug therapy
and any complications were recorded in a structured case record
form using case papers of the patients and interview. All the
laboratory investigations carried out for the patients and change
in drug therapy after investigations was also recorded. Disease
related details like temperature measurement method and physical
treatment, patient characteristics (age, gender and main symptoms,
including maximal temperature), medication taken with or
without prescription, antibiotics consumed or not and medication
advice followed or not. Physicians were also asked to give information
about temperature measurement during the consultation
and the final diagnosis (like upper/lower respiratory infection, enteric
fever, malaria, sore throat, isolated fever, gastroenteritis, rash,
influenza or other).
All the patients’ treatment protocol was compared with the standard
treatment guidelines issued by the WHO for fever management
and local standard treatment guidelines of the state.
As per all the guidelines for management of fever following steps
are important:
o Take detail history of fever (temp. reading, type of fever, shivering/
perspiration present or not) and associated symptoms.
o With help of symptoms of the system involved each to clinical
diagnosis like respiratory tract illness, GI infection, Urinary tract
infection, malaria etc (provision/clinical diagnosis).
o Confirm the diagnosis with relevant laboratory tests (like CBC,
S. widal test, blood smear examination, stool or urine examination
etc) – confirmed diagnosis.
o Give treatment both definitive and symptomatic as per the confirmed
diagnosis.
o If started with the empirical treatment, before laboratory investigations,
change to definitive treatment.
All case sheets were reviewed for following of these steps and
divided in to two groups (A & B). Group A included the patients
who were treated as per the guidelines and group B included the
patients who were not treated as per the standard guidelines. For
ease of data analysis, those patients advised any laboratory investigations
for confirmation of diagnosis and treatment were
grouped as A and those who were not advised laboratory investigations
were grouped as B.
Use of antipyretics, antibiotics and other supportive medicines
as well as outcome of fever was compared of the patients given
treatment as per standard guidelines with those not treated as per
guidelines.
The study protocol was approved by the institutional ethics committee
and written informed consent was obtained from all patients
before enrolling them for the study. Participants did not
receive compensation for their participation in this study. All the
patients were given assurance about protecting data confidentiality
and anonymity. Copies of the consent forms were given to
participants and they had the right to refuse participation or withdraw
from the study at any stage without hampering their medical
treatment.
Data analysis was done using Microsoft excel 2010. All the data
are presented as actual frequencies, percentages, mean and standard
deviation. Chi square test was used for comparison of qualitative
data and students’t test was used for quantitative data. P value
less than 0.05 was considered significant.
Results
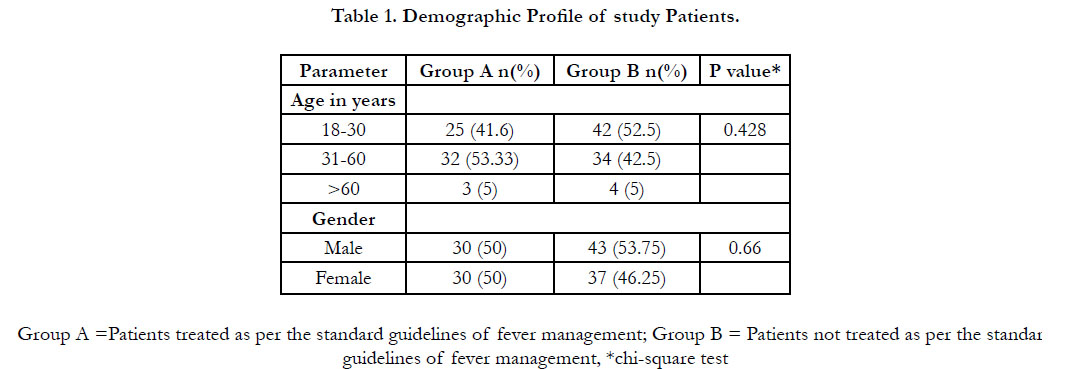
Total 140 patients having fever were enrolled for the study and
their fever management protocol were evaluated. Out of these
140 patients, 60 patients were managed as per standard treatment
guidelines (group A) and 80 patients were not managed as per the
guidelines (group B). Age and gender wise distribution of patients
of both groups is shown in table 1. Majority of patients (47.86 %)
belonged to age of 18-30 years and 30-60 years (47.14 %) while
only 5% patients belonged to > 60 years of age. 52.14 % patient
were male and 47.86 % were females. No statistically significant
difference was found among demographic parameters (p>0.05)
in both groups.
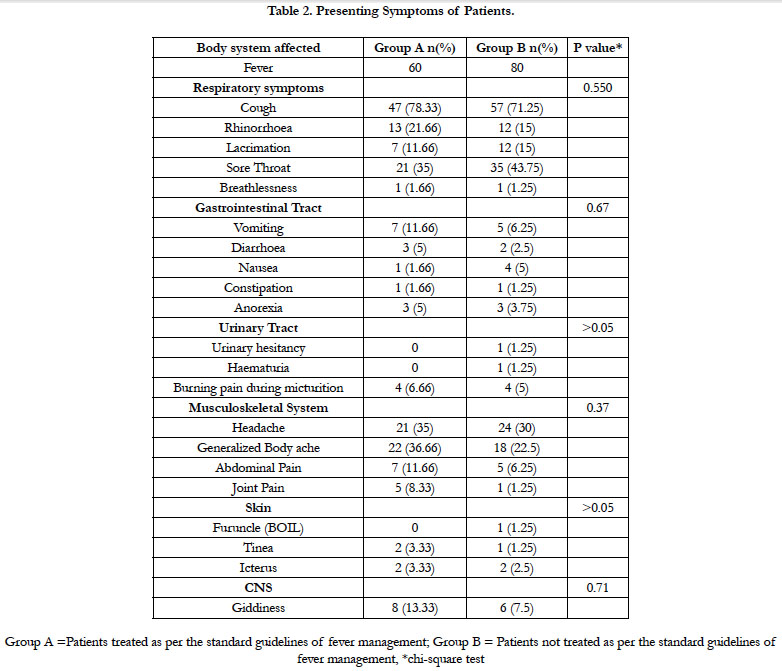
Presenting symptoms of the patients and their body system wise distribution is shown in table 2. Symptoms related to Upper respiratory tract infection (URTS), such as cough and rhinorrhoea, were the most common symptoms (104 patients, 74.28%) as per body system wise distribution. Symptoms related to gastrointestinal system and urinary system were less frequently observed. There was no significant difference between presenting symptoms among both the groups (p>0.05).
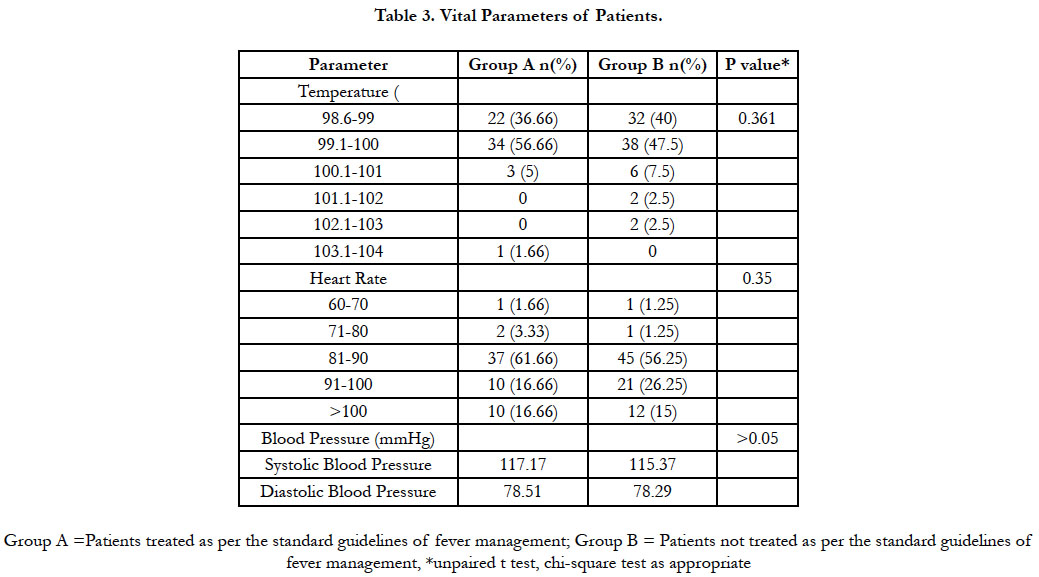
All the patients were subjected to detailed history and clinical examination. Patient’s vital parameters are shown in table 3. Mean temperature of patients was 99.45 and 99.42 in group A and group B respectively. Mean heart rate was 87.39 and 87.45 in group A and B respectively. The mean systolic and diastolic blood pressure in group Apatients was found to be 115.37 mmHg and 78.29 mmHg respectively and in group B it was found to be 115.37 mmHg and 78.29 mmHg respectively, with no statistically significant difference among the groups.
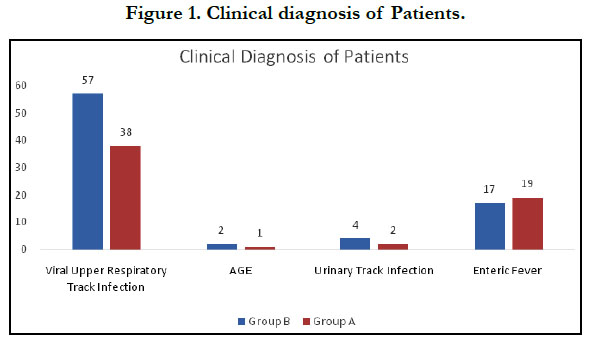
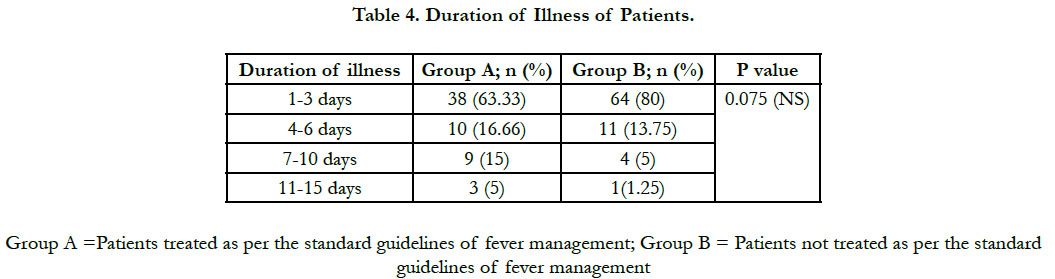
Clinical diagnosis was arrived in all the patients and most common disease was URTI in both the groups followed by enteric fever, acute gastroenteritis and urinary tract infection as shown in figure 1. There was no statistically significant difference was found among provisional diagnosis of the patients (p>0.05). Even there was no statistical significance observed in duration of illness of patients enrolled in both the groups for treatment purpose (table 4).
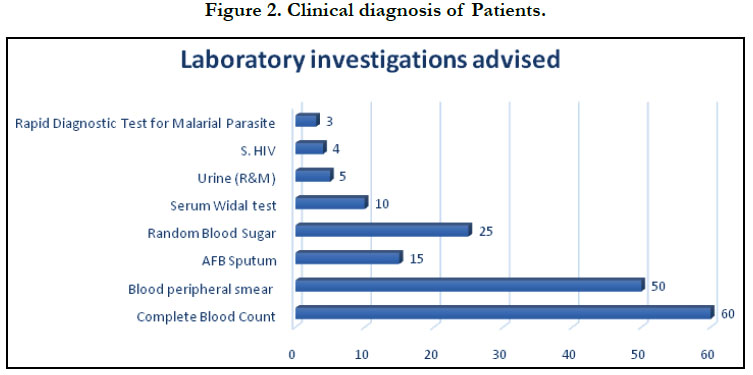
All the patients of group A were advised some or other laboratory investigations to confirm the diagnosis as per the standard management protocol. Most frequently ordered investigations were complete blood count and peripheral smear for malarial parasite. Other laboratory parameters evaluated were liver function test, urine examination, stool examination, blood and sputum culture etc as shown in figure 2. Due to lack of confirmatory tests in group B patients, no definitive diagnosis was reached and thy were treated based on clinical judgement only.
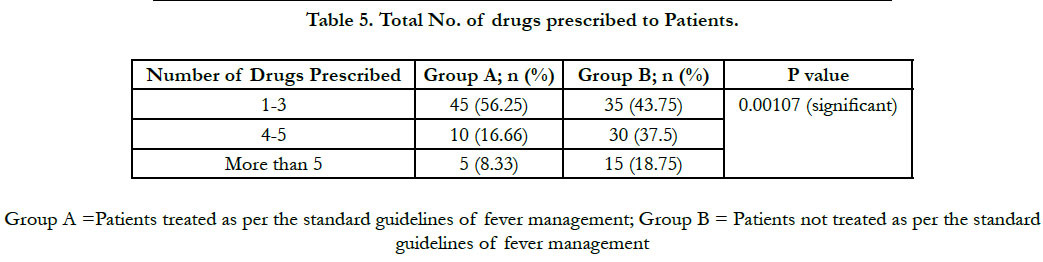
Drug treatment given for the fever patients was compared among both groups. Average number of drugs prescribed was 2.94 and 4.03 in group A and B (p value 0.001). Out of total 140 patients, 56.25% and 43.75% belonged to category of 1-3 drugs prescribed in group Aand Brespectively while 16.66% and 37.5% were belonged to category of 4-5 drugs per prescription and 8.33% and 18.75% were belonged to category of more than 5 drugs per prescription in group A and B respectively (Table 5). There was significantly higher number of drugs prescribed per prescription in group B. (p=0.001).
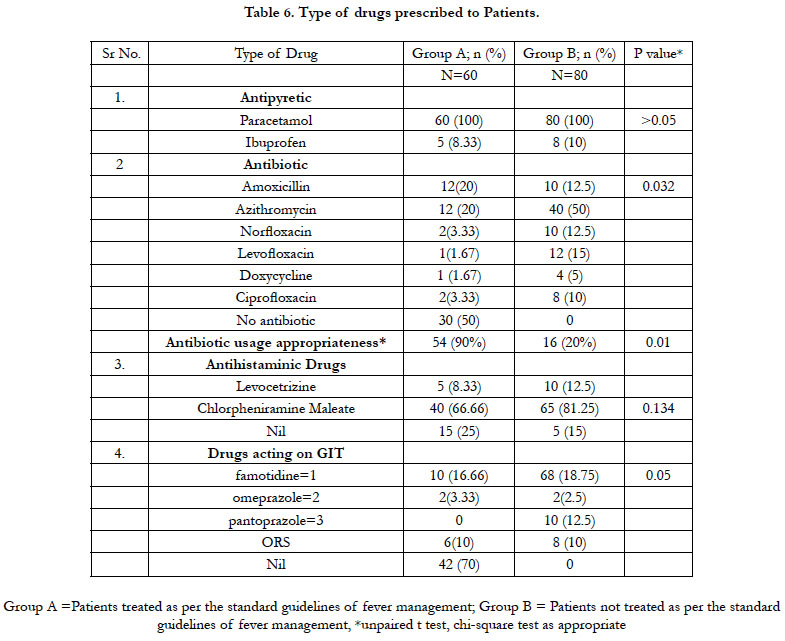
Analysis of drug therapy among both the group patients is shown in table 6. All the patients were prescribed antipyretic, i.e. paracetamol with few patients requiring additional ibuprofen for control of fever. Antibiotics were prescribed to 50% and 100% of patients in group A and B respectively with statistically significant difference (p=0.03). It was found that Amoxicillin and Azithromycin were the most preferentially prescribed antibiotics by the physicians to patients with symptoms of fever.On comparing the use of antimicrobials with the standard treatment guidelines, it was found that 90% and 20% of antibiotics were prescribed appropriately (P=0.01). Prescribing antihistaminic drugs by physicians as an adjuvant therapy to patients suffering from symptoms of fever were reportedly found to be non-significant in both the groups respectively (p>0.05) while drugs acting on GIT like famotidine, pantoprazole etc were prescribed significantly high in group B (p<0.05).
Discussion
This cross-sectional study is the first of its kind investigating the
clinical profile of diverse group of patients suffering from a common
clinical symptom of fever and its management in rural areas
of western India. Our sample was drawn from patients of different
ages came for treatment of fever to primary health care
centres in Gujarat and analysed for its management comparison
with standard treatment guidelines issued by WHO or state government.
Evidences pertaining to Upper respiratory tract infections (URTIs)
are the most commonly encountered diseases for visiting the
doctor, in all groups of patients. URTIs are the major causes of
morbidity and mortality with a worldwide disease burden estimated
at 112 900 000 and 3.5 million deaths, respectively which was
also coinciding with the results of this study that reveals URTIs
as most prevalent cause of fever in majority of patients followed
by Acute gastric enteritis, UTI and enteric fever [11].
Our study found that 28.5% of patients reported using antibiotics
without undergoing laboratory tests to confirm the diagnosis for
bacterial aetiology. Comparatively, a similar study was conducted
by Y. Lui et al., 1999, found a slightly lower prevalence of use
of antibiotics (25.1%) amongst 203 out-patients in Taiwan without
undergoing laboratory examination [1]. Another study conducted in Northern Uganda showed a much higher prevalence
of reported antibiotic use of 62.2% without performing lab tests
contributing a prevalence of 30.4%. This considerable difference
in reported use could likely be as a result of the high prevalence
of non-prescription use of antimicrobials in Northern Uganda
(75.7%) [2]. Again, another study at two hospitals in Ghana found
a higher prevalence of antibiotics in urine (64%) [3].
The significant pervasiveness of prior antibiotic use found in
this study could be attributed to the proliferation of antibiotic
sources, lax drug regulatory legislation and insidious exposure to
antibiotics used in clinical practice and this kind of increased and
inappropriate use of antibiotics has serious implications since it
contributes to selective pressure, favouring the development antibiotic
resistance [4, 12, 13]. Earlier studies reveals that, ceftriaxone
and cefixime seemed to be the first line of antibiotic treatment
for enteric fever however despite of susceptibility, clinical non-response
was seen in around 10 per cent of the patients who needed
combinations of antibiotics with penicillin’s and macrolides as
choice of agents in treatment of fever [14, 15].
Interestingly, more than 25% of patients among the ‘fever symptom
group with no pathological’ were prescribed antibiotics at
primary health care centres. In accordance with treatment guidelines
and recommendations, only patients who have a confirmed
infectious diagnosis are expected to be given an antibiotic prescription [13, 16, 17]. Nonetheless, empirical or presumptive antibiotic
therapy is also accepted when the clinical diagnosis, based
on the presence of a strong clinical suspicion of bacterial infection,
is substantiated by relevant medical history and clinical findings
[13].
According to the WHO and the Indian National Treatment
Guidelines for Antimicrobial Use, presumptive therapy is typically
a one-time treatment given for clinically presumed infection
while waiting for the laboratoryinvestigations [16, 17]. According
to the WHO and the Indian National Treatment Guidelines
for Antimicrobial Use, presumptive therapy is typically a one-time
treatment given for clinically presumed infection while waiting for
the pathological report [18]. It was distinctly observed that the
average duration of treatment was lower in group of patients undergone
pathological examination resulting in lower number of
drugs prescribed which needs to be encouraged. There may be
an increase in compliance, lower cost of therapy and decreased
risk of drug interactions with reduced duration of treatment supported
by earlier studies investigating fever of unknown origin
justified that duration of illness and treatment extends in case of
lack of pathological examination [19, 20].
The practice of prescribing antibiotics to patient groups with no
registered bacterial infection in the absence of laboratory confirmation
could not be considered to be rational. Among the patients
with COPD and RHD, the aetiology of the current episode of
hospitalisation could potentially be expected to be non-bacterial
(e.g, viral infection). However, this could not be confirmed owing
to the absence of laboratory investigations. It is worth mentioning
here that prolonged empirical antibiotic treatment without a
clear evidence of infection is one of the causes of the development
of antibiotic resistance. A higher incidence of prescribing
macrolides, cephalosporinsand fluoroquinolone classes is further
supported by Van Boeckel et al., who observed a significant increase
in the consumption of fluoroquinolones and cephalosporins
globally over the past decade. This increase was mainly attributed
to the increased rates in India and China [21].
In this study both the duration of treatment and the duration
of antibiotic treatment were longer in patients without undergoing
laboratory examination, possibly because of random use of
drug combination without proper justified etiological examination.
This association of longer duration of illness and antibiotic
treatment in patients without laboratory investigations has also
been found in previous studies as well [22, 23].
Irrational use of antibiotics contributes towards difficulties faced
in trying to diagnose specific diseases without the access to diagnostic
tools at health facilities. Various other barriers substantiating
reason for irrational use of antibiotics are the lack of funds
for further diagnostic tests, the shortage of specialists at referral
facilities, deficiencies of the laboratory services (unreliable and
poorly equipped), the limited access to communications and lack
of institutional support and opportunities for training.
A large number of patients were screened over a year period; this
obviates seasonal variations in infectious aetiology, which would
affect antibiotic prescribing strategy with collaboration of pathological
analysis. The same form was used for the data collection
and the process was supervised and monitored by same person at
all hospitals to improve the reliability of the data. The method of collection of data used in the study is robust and reliable. In accordance
with one of the WHO goals of the ‘Global Action Plan’
and in view of limited knowledge of antibiotic use and resistance
patterns, our study suggests that there is a need to conduct similar
long-term surveillance studies globally.
Conclusion
A larger number of patients suffering from fever with their prescribing
occasions were recorded for the study. It was evidently
observed that fever was a factor leading to antibiotic prescription
at health care facility. Large number of patients without any
laboratory investigations and without confirmation of bacterial
infections were prescribed with antibiotics, which could not be
justified. Broad-spectrum antibiotics with irrational combinations
of antibiotics with other adjuvant therapeutics agents were commonly
prescribed in the study for non-indicated conditions may
contribute to elevated duration of treatment. If microbiology reports
could have confirmed the aetiology, some of these might
have been categorised in the non-bacterial group and antibiotic
misuse can be minimised. However, this was not possible to study
in depth owing to the absence of confirmed aetiology and the
nature of the study design (observational). Educational interventions
and continuous learning programs can be implemented for
all practitioners for rational use of drugs specially antimicrobials.
References
- Schmitt BD. Fever phobia: misconceptions of parents about fevers. Am J Dis Child. 1980; 134: 176–181. PMID: 7352443.
- Rkain M, Rkain I, Safi M, Kabiri M, Ahid S, Benjelloun BDS. Knowledge and management of fever among Moroccan parents. East Mediterr Health J. 2014; 20(6): 397–402. PMID: 24960517.
- Thota S, Ladiwala N, Sharma PK, Ganguly E. Fever awareness, management practices and their correlates among parents of under five children in urban India. Int J ContempPediatr. 2018; 5: 1368-1376. PMID: 30035204.
- A Sahib Mehdi El-Radhi. Fever management: Evidence vs current practice. World J Clin Pediatr. 2012 Dec 8; 1(4): 29–33. PMID: 25254165.
- Crump JA. Time for a comprehensive approach to the syndrome of fever in the tropics. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2014; 108(2): 61-2. PMID: 24463580.
- Joshi R, Colford JM, Reingold AL, Kalantri S. Nonmalarial acute undifferentiated fever in a rural hospital in central India: diagnostic uncertainty and overtreatment with antimalarial agents. The American journal of tropical medicine and hygiene. 2008; 78(3): 393-9. PMID: 18337332.
- Phuong HL, de Vries PJ, Nagelkerke N, Giao PT, Hung le Q, Binh TQ, et al. Acute undifferentiated fever in BinhThuan province, Vietnam: imprecise clinical diagnosis and irrational pharmaco-therapy. Tropical medicine & international health. 2006; 11(6): 869-79. PMID: 16772009.
- Susilawati TN, McBride WJ. Acute undifferentiated fever in Asia: a review of the literature. The Southeast Asian journal of tropical medicine and public health. 2014; 45(3):719-26. PMID: 24974656.
- Singhi S, Chaudhary D, George M Varghese, Ashish Bhalla, N Karthi, S Kalantri, et al., Tropical fevers: Management guidelines. Indian J Crit Care Med. 2014; 18(2): 62–69. PMID: 24678147.
- JoshiR, Kalantri SP. Acute Undifferentiated Fever: Management Algorithm. in Update on Tropical Fever. 2015; 1–14.
- Murray C, Lopez A. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997; 349:1436–1442. PMID: 9164317.
- Bertille N, Pons G, Khoshnood B, Fournier-Charrière E, Chalumeau M. Symptomatic Management of Fever in Children: A National Surveyof Healthcare Professionals’ Practices in France. 2015; 10(11):e0143230. PMID: 26599740.
- Liu YC, Huang WK, Huang TS, Kunin CM. Extent of antibiotic use in Taiwan shown by antimicrobial activity in urine. Lancet. 1999; 354(9187): 1360. PMID: 10533872.
- Patil KR, Mali RS, Dhangar BK, Bafna PS, Gagarani MB, Bari SB. Assessment of prescribing trends and quality of handwritten prescriptions from rural India. J PharmaSciTech. 2015; 5: 54– 60.
- Uma B, Prabhakar K, Rajendran S, Lakshmi Sarayu Y. Prevalence of extended spectrum beta lactamases in Salmonella species isolated from patients with acute gastroenteritis. Indian J Gastroenterol. 2010: 29: 201– 204. PMID: 20859716.
- Ocan M, Bwanga F, Bbosa GS, Bagenda D, Waako P, Ogwal-Okeng J, et al. Patterns and predictors of self-medication in northern Uganda. PLoS One. 2014; 9(3):1.
- Lerbech AM, Opintan JA, Bekoe SO, Ahiabu MA, Tersbøl BP, Hansen M, et al. Antibiotic exposure in a low-income country: Screening urine samples for presence of antibiotics and antibiotic resistance in coagulase negative staphylococcal contaminants. PLoS One. 2014; 9(12):1–18. PMID: 25462162.
- Vila J. Update on Antibacterial Resistance in Low-Income Countries: Factors Favoring the Emergence of Resistance. Open Infect Dis J. 2010; 4(2):38–54.
- Murray C, Lopez A. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997; 349:1436–1442. PMID: 9164317.
- Petersdorf RG, Beeson PB. Fever of unexplained origin: report on 100 cases. Medicine (Baltimore) 1961; 40:1–30. PMID: 13734791.
- Dougherty TJ, Pucci MJ. Antibiotic discovery and development. Antibiotic Discovery and Development. 2014; 1–1127.
- Opintan JA, Newman MJ, Arhin RE, Donkor ES, Gyansa-Lutterodt M, Mills-Pappoe W. Laboratory-based nationwide surveillance of antimicrobial resistance in Ghana. Infect Drug Resist. 2015; 8: 379– 89. PMID: 26604806.
- National Centre for Disease Control India. India national treatment guidelines for antimicrobial use in infectious diseases. Version 1.0. New Dehli, 2016: 1–64.
- Bennet JE, Blaser MJ, Dolin R. Principles and practice of infectious diseases. Elsevier Saunders; 2015.
- Davey P, Wilcox M, Irwing W. Antimicrobial chemotherapy. 7th edn. Oxford University Press, 2015.
- Van Boeckel TP, Gandra S, Ashok A, Quentin Caudron, Bryan T Grenfell, Simon A Levin, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. 2014; 14: 742–50. PMID: 25022435.
- World Health Organization. The evolving threat of antimicrobial resistance: options for action. WHO Publications. Geneva, 2014.
- WHO. Promoting rational use of medicines: core components. WHO Policy Perspect Med. 2002.