Solitary Sinonasal Fibrous Tumour: A Rare Presentation And Pathology
A.S. Harugop1, Priti Hajare2, R.S. Mudhol3, Dharmishtha R. Kaku4*, Bijjal Raj4, Vishnu V. Pillai4, Deepika Reddy Ramidi4
1 Professor and Head of Department, Department of ENT and Head and Neck Surgery, Jawaharlal Nehru Medical College , Nehru Nagar, Belagavi, Karnataka, India.
2 Professor, Department of ENT and Head and Neck Surgery, Jawaharlal Nehru Medical College , Nehru Nagar, Belagavi, Karnataka, India.
3 Vice Principal and Medical Superintendent, Professor, Department of ENT and Head and Neck Surgery, Jawaharlal Nehru Medical College, Nehru Nagar, Belagavi, Karnataka, India.
4 Resident, Department of ENT and Head and Neck Surgery, Jawaharlal Nehru Medical College , Nehru Nagar, Belagavi, Karnataka, India.
*Corresponding Author
Dr. Dharmishtha R. Kaku, MBBS,
Resident, Department of ENT and Head and Neck Surgery, Jawaharlal Nehru Medical College , Nehru Nagar, Belagavi-590010, Karnataka, India.
Tel: +919164403312
E-mail: dharmi_11@yahoo.co.in
Received: June 21, 2020; Accepted: August 01, 2020; Published: August 05, 2020
Citation: A.S. Harugop, Priti Hajare, R.S. Mudhol, Dharmishtha R. Kaku, Bijjal Raj, Vishnu V. Pillai, et al.,. Solitary Sinonasal Fibrous Tumour: A Rare Presentation And Pathology. Int J Clin Exp Otolaryngol. 2020;6(2):114-116. doi: dx.doi.org/10.19070/2572-732X-2000021
Copyright: Dharmishtha R. Kaku©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Solitary Fibrous tumour represents a spectrum of mesenchymal tumors, encompassing tumors previously termed as hemangiopericytomas.
They are vascular neoplasms of outer wall pericytes of Zimmermann’s capillaries. These tumors presumed to
be of fibroblastic differentiation, seen most commonly in adults and can occur at any site. We report the case of a young adult
male presenting with a swelling over medial canthus of left eye with a discharging sinus. Wide local excision was done and the
diagnosis was confirmed by biopsy and immunohistochemistry.
2.Introduction
3.Report
4.Discussion
5.Conclusion
6.References
Keywords
Solitary Fibrous Tumor; Haemangiopericytoma; Immunohistochemistry; CD34; Mic-2;bcl-2.
Introduction
Solitary fibrous tumor also known as benign fibrous mesothelioma
or submesothelial fibroma, is sub-classified under existing
mesothelial tumors [1]. Sinonasal hemangiopericytomas are variant
of solitary fibrous tumors. They are rare vascular neoplasms
of the outer wall pericytes of Zimmermann cells that lie external
to the reticulin sheath of capillaries and constitute around 1%
of all angiogenic tumors [2]. Here we report a 21 year old male
with sinonasal hemangiopericytoma. We performed a wide local
excision without the requirement of pre-operative embolization.
To our knowledge this is the first of its kind presentation of the
neoplasm requiring external approach for excision.
Report
A 21 year old male patient came to us with complaints of a swelling
over medial canthus of the left eye extending upto the left
bony dorsum and bridge of the nose since one and a half years.
On examination it was 2x3 cm firm, non fluctuant, non transilluminant and pinkish brown swelling with a discharging sinus over
its surface (Figure 1). The discharge was serosanguinous and nonfoul
smelling. He also gives complaints of blurring of vision in
the left eye with normal eyeball movement, probably due to mass
leison. Other complaints of nasal obstruction, epistaxis, fever and
weight loss were absent.
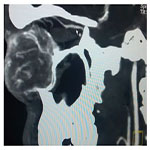
A CT scan was done to know the extent of the swelling and it revealed breach into the left anterior ethmoidal sinus while the left medial orbital wall was intact. Also anterior and posterior ethmoidal arteries were seen as feeding vessels to the tumor (Figure 2).
Figure 2. CT Contrast Showing Extent Of The Swelling with Anterior & Posterior Ethmoidal Arteries Supplying the tumor.
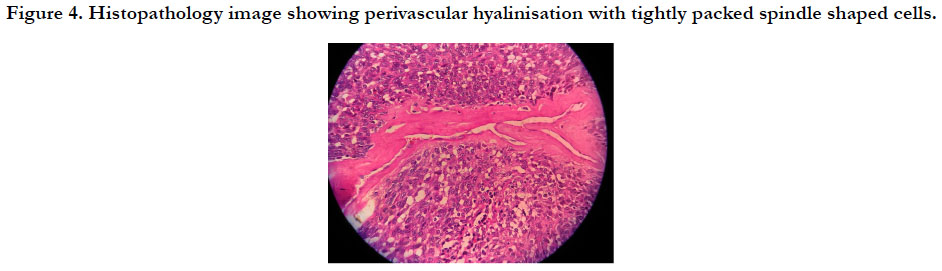
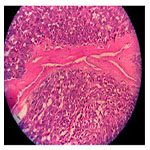
The patient was taken up for surgery and a wide local excision of the lesion was done. A curvilinear incision was taken below the swelling and was dissected from all the sides maintaining hemostasis (Figure 3). The mass was excised completely and the skin was sutured in layers. The mass was sent for histopathological examination. It showed neoplastic cells tightly packed with hyperchromatic nuclei which were situated around endothelial lined vascular spaces. There was presence of perivascular hyalinization in the vascular spaces characteristic of this tumor (Figure 4). The diagnosis was confirmed by immunohistochemistry which was positive for CD34, Mic-2 and bcl-2 and immunonegative for Smooth Muscle Actin (SMA), Desmin, S-100 protein and CD 31.
Figure 4. Histopathology Image Showing Perivascular Hyalinisation with tightly packed Spindle Shaped Cells.
At 6 months post operative follow up, the surgical site was healthy with no evidence of recurrence and good cosmetic outcome. (Figure 5)
Discussion
Solitary fibrous tumors composed of small cells individually separated
by thin bands of collagen fibres. They are categorized as
intermediate biological potential with low risk of metastasis and
an indolent course according to 2002 WHO classification. They
are also called as Benign Fibrous Mesothelioma or Submesothelial
Fibroma [3]. It was first described in the pleura by Klemper & Rabin in 1931 & later referred it as solitary fibrous tumor of pleura
& peritoneum with absence of mesothelial differentiation. Alternate
names are Haemangiopericytoma, Localised fibrous tumor
or Fibrous mesothelioma. Around 27 cases have been reported
in world literature. Various extra pleural sites the liver, eyelids,
orbit, paranasal sinuses, nose, parotid gland, tongue, sublingual
gland, parapharyngeal space, thyroid, and laryngopharynx have
also been reported in literature; but its occurrence in the nose and
paranasal sinuses is very rare and the first case report about its
involvement was from India [1]. They typically present as a soft
to firm, tan, gray, or white, polypoidal mass often confused with
ordinary nasal polyp and most of them arise from lateral wall of
nasal cavity. Nasal obstruction and epistaxis are the most common
symptoms and there is a risk of hemorrhage during biopsy
[4]. Around 23% of pleural tumors have aggressive behaviour as
compared to most nasal and extra-pleural solitary fibrous tumors
which are benign [5].
Haemangiopericytomas can be confused with angiofibroma and
lobular capillary hemangioma. This case had an exceptional presentation
as a swelling near to the left medial canthus extending
to the malar area and on CT scan it was seen extending to the
anterior ethmoids. Lobular capillary haemangioma was one of
the differential diagnosis but it is seen commonly in females and
commonly arises from the nasal septum. Although the role of
angiography is not clearly defined, it is used for preoperative planning
& embolization to reduce the intraoperative haemorrhage [6].
However in the present case, angiography was not done keeping
in mind the affordability of patient.
Haemangiopericytomas are characterized as benign or malignant,
round to spindle cell tumors with numerous “staghorn” branching
vascular channels. The histopathology picture is similar to lobular
capillary hemangioma which also shows lobular arrangement of
capillaries around a large central vessel along with spindled, pericytic
cells which are positive for smooth muscle cell actin which is
also present in hemangiopericytoma [6]. Due to lack of electron
microscopic differentiation properties of pericytes, there is difficulty
in predicting clinical behavior of this tumor. Mc Masteret
al identified three grades of this tumour as benign, borderline and
malignant [7].
The present case histopathology was suggestive of haemangiopericytoma.
Haemangiopericytoma and lobulary capillary haemangioma
often resemble each other and the course and management
of both is entirely different. Immunohistochemistry is
used to differentiate between them [8]. In the present case, the
diagnosis of solitary fibrous tumor was established on immunohistochemistry.
Solitary fibrous tumors are positive for CD34,
bcl2, CD99 and Factor XIIIa. In this case immunohistochemistry
was positive for CD34, Mic-2 and bcl-2 while immunonegative
for SMA, Desmin, S-100 protein and CD31.
Treatment of solitary fibrous tumor involves wide surgical excision,
for that of the nasal cavity involves endoscopic excision as
the preferred surgical approach, although lateral rhinotomy, external
ethmoidectomy, medial maxillectomy and transfacial endoscopic
approaches have been described and majority have excellent
long term prognosis following surgery [1, 9, 10].
The case was successfully managed with wide local excision without
embolization, thus avoiding morbidity and scarring associated
with radical excision. Also on follow up good functional and cosmetic
outcome was achieved.
Conclusion
The facility of immunohiostochemistry should be utilized in cases
of diagnostic dilemma. As solitary fibrous tumors are relatively
radioresistant, their effective management requires wide surgical
excision with clear resection margins. An incomplete primary excision
is the primary factor in recurrent disease and other factors
include osseous invasion, large tumor size (more than 5 cm),
severe nuclear pleomorphism and a high mitotic to proliferation
rate. This case highlights the importance of diagnosing solitary
fibrous tumors of the nasal cavity and paranasal sinuses, as their
management differs from other tumours and stresses the importance
of immuno-histochemical in the diagnosis of solitary fibrous
tumor.
References
- Ashish G, Mathew GA, Tyagi AK, Chandrashekharan R, Paul PR. Solitary Fibrous Tumor of Nasal Cavity: A Case Report. Iranian Journal of Otorhinolaryngology. 2015; 27(4): 307-12. PMID: 26788480.
- Batsakis J. Tumors of Head and Neck: Clinical and pathological considerations (2nd Ed). Baltimore: Williams and Wilkins. 1979; 307-12.
- Demicco1 EG, Park MS, Araujo DM, Fox PX, Bassett RL, Pollock RE et al. Solitary fibrous tumor: a clinicopathological study of 110 cases and proposed risk assessment model. Modern Pathology. 2012; 25: 1298–1306. PMID: 22575866.
- Del Gaudio JM, Garetz SL, Bradford CR, Stenson KM. Haemangiopericytoma of oral cavity. Otolaryngol Head Neck Surg. 1996; 114:339-40. PMID: 8637767.
- Zeitler DM, Kanowitz SJ, Har-El G. Malignant solitary fibrous tumor of the nasal cavity. Skull Base. 2007 Jul; 17(4): 239–46. PMID: 18174924.
- B Kumar, B Pant, D Isser. Nasal Hemangiopericytoma –A Pathological Illusion. The Internet Journal of Pathology. 2013; 13(3):1-5.
- Mc Master MJ, Soule EH, Irins JC. Hemangiopericytoma: a Clinicopathologic study & longterm follow up of 60 patients. Cancer. 1975: 36: 2232- 2244. PMID: 1203874.
- Dabholkar JP, Sathe NU, Patole AD. Nasal Glioma- A Diagnostic Challenge. Indian J Otolaryngol Head Neck Surg. 2004 Jan; 56(1): 27-8. PMID: 23120021.
- Watanabe K, Saito A, Suzuki M, Yamanobe S, Suzuki T. True Hemangiopericytoma of the Nasal Cavity, Immunohistochemical and Electron Microscopic Study of 2 Cases and a Review of the Literature on Sinonasal Hemangiopericytomas. Archives of Pathology and Laboratory Medicine. 2001; 125(5): 686–690.
- Kessler A, Lapinsky J, Berenholz L, Sarfaty S, Segal S. Solitary fibrous tumor of the nasal cavity. Otolaryngol--Head Neck Surg. 1999 Dec; 121(6): 826–8.