Reflux Symptom Index (RSI) and Reflux Finding Score (RFS) in Management of Laryngopharyngeal Reflux in Indian Scenario
Shahul Hameed Poondiyar Sirajuddin1*, Sumathi Veluswamy2, Ramesh Duraisamy3
1 Registrar, Department of Otorhinolaryngology, Sundaram Medical Foundation Dr. Rangarajan Memorial Hospital, Chennai, India.
2 Senior Consultant and Head of the Department, Department of Otorhinolaryngology, Sundaram Medical Foundation Dr. Rangarajan Memorial Hospital, Chennai, India.
3 Senior Consultant, Department of Otorhinolaryngology, Sundaram Medical Foundation Dr. Rangarajan Memorial Hospital, Chennai, India.
*Corresponding Author
Dr.Shahul Hameed Poondiyar Sirajuddin,
Department of ENT, Sundaram Medical Foundation Dr. Rangarajan Memorial Hospital, Chennai, 600040, India.
Tel: (+91) 44 2626 8844, (+91) 44 2614 4100
Fax: 26284257
E-mail: shahulgenius@gmail.com
Received: May 19, 2020; Accepted: June 03, 2020; Published: June 05, 2020
Citation: Shahul Hameed Poondiyar Sirajuddin, Sumathi Veluswamy, Ramesh Duraisamy. Reflux Symptom Index (RSI) and Reflux Finding Score (RFS) in Management of Laryngopharyngeal Reflux in Indian Scenario. Int J Clin Exp Otolaryngol. 2020;6(2):108-113. doi: dx.doi.org/10.19070/2572-732X-2000020
Copyright: Shahul Hameed Poondiyar Sirajuddin©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To study the role of Reflux Symptom Index (RSI) and Reflux Finding Score (RFS) for assessment of severity in Laryngopharyngeal Reflux (LPR) and to assess the improvement of symptoms following treatment with Proton Pump Inhibitors (PPI) using RSI.
Design: Prospective single blinded observational study.
Methods: Patients with symptoms of LPR with RSI and RFS scores more than 7 were included in the study and were treated with PPI for 8 weeks and followed up with RSI.
Results: A total of 107 patients were included over a period of 7 months.There is a positive correlation between RSI and RFS taken before starting treatment (P = 0.016). The mean of RSI score as well as all the 9 individual symptoms showed statistically significant decrease after therapy.
Conclusion: RSI & RFS scores of 7& above can be considered as clinical indicators of LPR and RSI alone can be used to assess its treatment.
2.Introduction
3.Materials and Methods
4.Results and Analysis
5.Discussion
6.Conclusion
7.Ethical Standards
8.Bullet Point Summary
9.References
Keywords
Laryngopharyngeal Reflux; Proton Pump Inhibitors; Prospective; Patients; Questionnaire; Laryngoscop.
Introduction
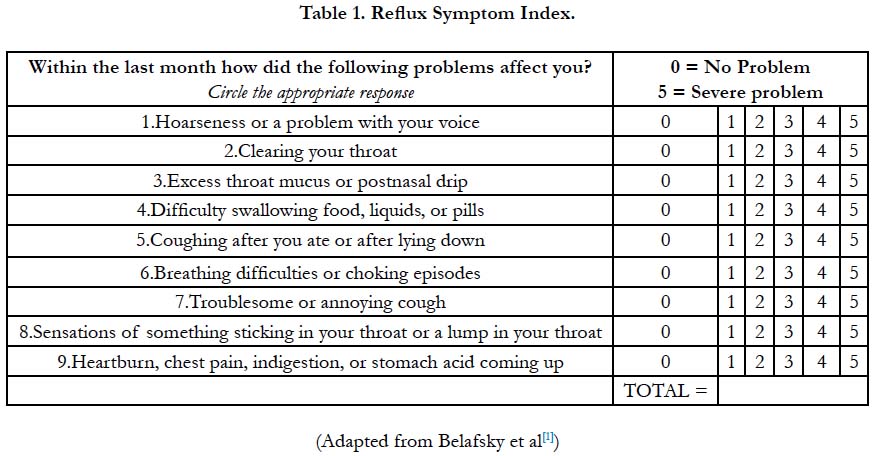
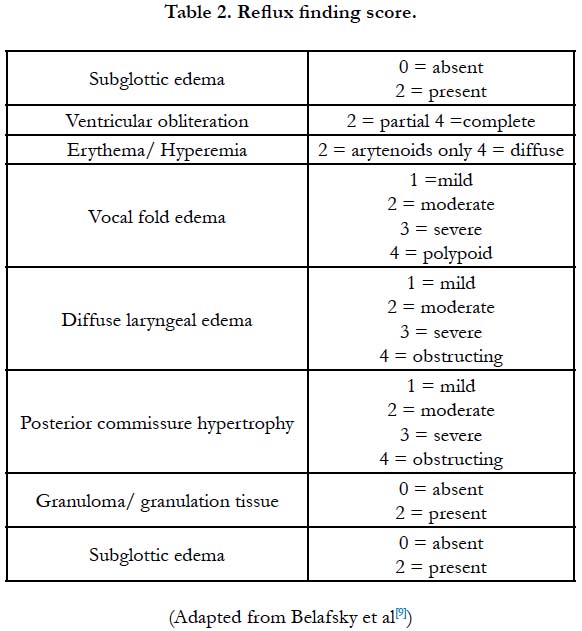
Laryngopharyngeal Reflux (LPR), also known as Reflux laryngitis, is escape of the refluxed gastric contents from esophagus into pharynx and larynx. It has been reported that up to 10% of otolaryngology clinic patients overall and approximately 64% of patients with voice complaints have been diagnosed with Laryngopharyngeal reflux [1, 2]. As there are no pathognomonic symptoms or signs in Laryngopharyngeal reflux, validated assessment tools such as Laryngeal Symptom score (LSS), The Reflux Symptom Index (RSI), laryngopharyngeal reflux health related quality of life (LPR-HRQL) questionnaire, Reflux Finding Score (RFS) scores etc have been introduced and are widely used to assess the severity of LPR [3]. Among them The Reflux Symptom Index (RSI) along with Reflux Finding Score (RFS) introduced by Belafsky et al., (2002) are widely used for initial assessment.
The aim of our study was to study the role of Reflux Symptom Index (RSI) and Reflux Finding Score (RFS) as clinical indicators for assessment of severity in Laryngopharyngeal Reflux (LPR) and to assess the improvement of symptoms following Proton Pump Inhibitors(PPIs) based on the pre and post treatment RSI. A period of 2 to 3 months is necessary to establish benefit from the medication with proton pump inhibitors. Laryngeal reflux symptoms resolve sooner than the findings which may take 6 months or longer to reverse [4]. Hence in our study RSI alone was taken for assessing the outcome after two months of treatment with proton pump inhibitors.
Materials and Methods
Between April 2016 to October 2016, 108 patients attending the Department of Otorhinolaryngology (ENT) in Sundaram Medical Foundation Dr. Rangarajan Memorial Hospital, Chennaifor evaluation of symptoms suggestive of LPR were included in aprospective single blinded observational study which was initiated with Institutional ethics and scientific committee approval. RSI questionnaire was translated into native Tamil language and its credibility was checked by using forward and backward translations. Patients were asked to complete the questionnaire independently and were subjected to Endoscopic laryngeal examination by an examiner who was blinded to the RSI score (Table I & II). In a pilot study done before this study, we found that many patients with significant RFS scores had RSI score as low as 7 and so in order not to miss those patients with high probability of LPR, we included patients with both RSI and RFS scores more than 7 in our study. They were started on treatment with Esomeprazole 40 mg twice daily for total treatment duration of 8 weeks along with advice on dietary and lifestyle modifications. Their compliance to treatment was ensured by phone every fortnightly till the end of treatment period. Patients with RSI & RFS less than 7 were advised dietary and lifestyle modifications and were excluded from the study. Also, patients on Proton Pump Inhibitors (PPIs) or a washout period of less than 6 weeks since initiation of PPI treatment, patients who were noncompliant to treatment, patients with benign and malignant diseases of Larynx, Pharynx and Oesophagus and patients with intolerance to Proton Pump Inhibitors were excluded from study.
At the end of 8 weeks, post treatment Reflux Symptom Index (RSI) was taken and compared with the pre-treatment scores. All data from the questionnaires were collected and fed into the statistical analysis database. All variables of the questionnaires were analysed descriptively. Patients with a reduction of RSI score were regarded as successfully treated and those patients whose symptoms persisted even after 8weeks treatment were referred to gastroenterologist for further assessment.
Data were entered in Microsoft excel 2007 and Descriptive analysis was shown by frequency & proportion charts. SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp. was used for statistical analysis tests to test the level of significance. Pearson correlation and Spearman’s rho correlation were used to correlate RSI with RFS. Wilcoxon signed rank test was done to test the significance of RSI at baseline and follow up. Paired Students’st-test was done to find the significance of mean of RSI at baseline and follow up. P value was considered significant if P≤0.05.
Results and Analysis
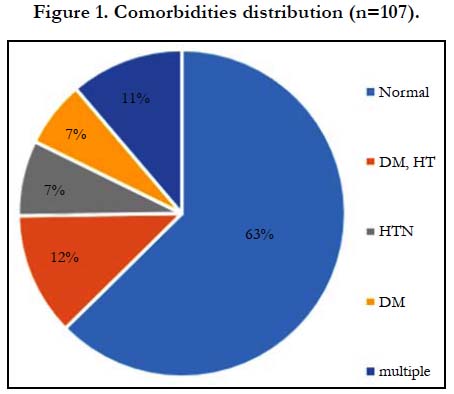
Our study group of 107 had patients between 20 to 70 years of age. Maximum patients were in the age group of 50-60, (29 patients) with male predominance (59%). Only 40 patients had associated co-morbidity (Figure I). Among them Diabetes with Hypertension (14%) was the most common condition. 79% patients were overweight and obese and the mean BMI was 29.17 ± 4.07. All smokers and alcoholics were male constituting 16.8% of our study population. Majority of our study population were Nonvegetarian with 38% having irregular food habits and 47% having history of spicy food intake.
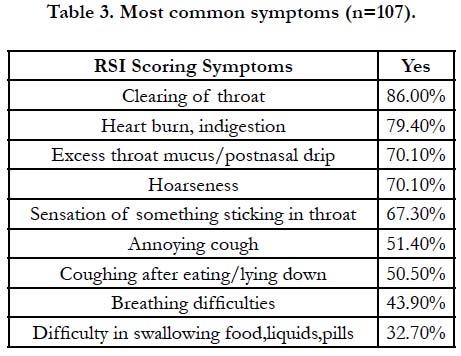
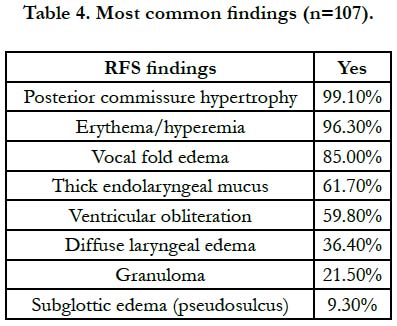
The mean pre-treatment RSI score for 107 patients was 15.45 ± 7.85. Clearing of throat (86%), followed by heart burn (79.4%) and hoarseness (70.1%) were the most common symptoms in our study (Table III). The mean pre-treatment RFS was 9.33 ± 2.44 and Posterior commissure hypertrophy (99.1%) was the most common finding (Table IV).
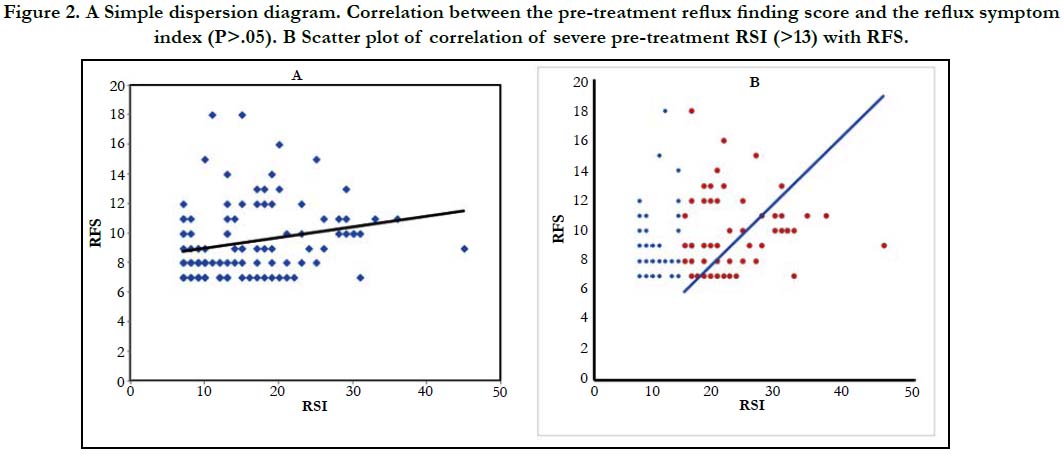
There was a positive correlation between RSI and RFS taken before starting treatment which was statistically significant (P=0.016, P<0.05). We also found that the correlation was stronger with greater RSI scores (RSI >13). (Figure IIA &B).
Figure 2. A Simple dispersion diagram. Correlation between the pre-treatment reflux finding score and the reflux symptom index (P>.05). B Scatter plot of correlation of severe pre-treatment RSI (>13) with RFS.
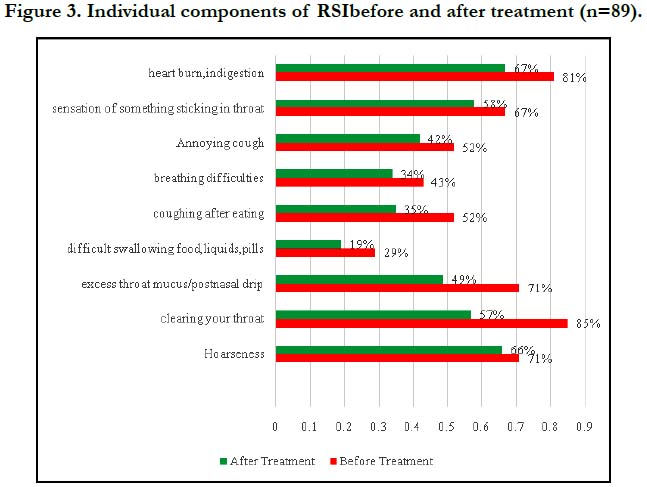
In our study, the mean RSI before therapy was 15.09 ± 7.51 and it decreased at the end of therapy to 3.78 ± 4.94 (P = 0.000). All the 9 individual components of RSI showed statistically significant decrease after therapy in our study. (Figure III)
Discussion
Diagnosis of LPR in the outpatient setting is usually made based on the history, symptoms and laryngeal signs. Our aim was to assess whether the validated assessment tools, Reflux Symptom Index and Reflux Finding Score can be used for assessing and treating LPR, so that they can be used as an outpatient assessment tool in daily otorhinolaryngologic practice in a developing nation such as India.
Our results were comparable to those of earlier studies in most aspects including the demographic profile. In the primary study by Belafsky et al (n=25), the mean age of LPR patients was 57 ± 17 and 56% of the patients were males which was reflected in our study results too1. Moreover,Spandeas et al [5]., who conducted a study on Greek population (n=340), showed that subjects in the age group of 50-64 years had higher prevalence rate of LPR, and there was no statistically significant difference between the two genders. Saruc et al., study on Turkish population (n=90) found that Male gender as one of the risk factors for the occurrence of LPR which was corroborative to our study’s male population [6].
In our study all smokers and alcoholics were male and constituted 16.8% of our study population similar to Haberman et al., where 23% of patients were smokers [7]. Also, according to Spantideas et al., a correlation was found between LPR and smoking and alcohol consumption [5].
Majority of our study population were Non-vegetarians with 38% having irregular food habits and 47% having history of spicy food intake. According to Bhatia et al., study (n=3224) non-vegetarian food was an independent predictor of GERD [8]. Although very few data are available for comparison, none of the food habits found to have any significant impact on symptoms and findings of LPR in our study.
The mean RSI score for 107 patients was 15.45 ± 7.85 in our study which was similar to Belafsky et al., where mean RSI was 19.9 ± 111. Clearing of throat (86%), followed by heart burn (79.4%) and hoarseness (70.1%) were the most common symptoms in our study whereas difficulty in swallowing food, liquids, or pills (32.7%) wasthe least common symptom.
Also, the mean RFS in our study was 9.33 ± 2.44 which was close to Belafsky et al., study where mean RFS was 11.5 ± 5.210. In Nunes et al., study (n=126) mean RFS was 9.53 ± 2.64 which was corresponding to our study [10]. Posterior commissure hypertrophy (99.1%) and Subglottic edema (9.3%) were the most common and least common findings,which were reassuring the findings of Belafsky et al., whose study documented posterior laryngeal hypertrophy in 85% of all patients before the initiation of treatment [9].
We found that there was a positive correlation between RSI and RFS taken before starting treatment which was statistically significant (P=0.016, P<0.05) and the correlation was stronger with severe RSI scores (RSI >13) which was similar to Iglesia et al., study [2], where a statistically significant correlation was found between the RSI and RFS, and the correlation was greater when the RFS score was more than 7.
RSI scores were determining the severity of LPR and in our study the mean RSI before therapy was 15.09 ± 7.51 and decreased at the end of therapy to 3.78 ± 4.94 (p=0.000). In Belafsky et al., study, the mean RSI before therapy was 21.2 ± 10.7 which showed a statistically significant decrease at the end of therapy to 12.8 ± 10.0 (p=0.001) akin to our study1. Also, in Habermann et al., study (n=1044), the median score of the RSI before therapy was 12 and decreased at the end of therapy to 3 which was analogous to our study [7].
The mean of all the 9 individual components of RSI showed statistically significant decrease after therapy in our study. This is in accordance with many studies reported in literature especially by Jasperson and Weber who demonstrated complete (100%) resolution of LPR symptoms after a 4 weeks treatment with 40 mg omeprazole per day as also demonstrated in our study [11]; Kamel and Hanson study showedthat patients had 92% response rate [12]; Our study is in contrast to other studies which demonstrate lack of therapeutic success in treating LPR patients with proton pump inhibitors. These are the studies by Ehrer [13], Wo and Koopman [14]; Steward et al [15]. Overdiagnosis of LPR can be cited as one of the reason for the inadequate response reported in these trials. This scenario of controversy can be avoided by profiling the patients using RSI score as followed in our study.
In addition to this, we found thatthough LPR symptoms are too unspecific to allow for the RSI questionnaire to establish a “diagnosis cut-off point,” we used a cut-off RSI score of 7 for excluding less symptomatic patients and we found that the RSI is better for evaluating treatment with PPIs and monitoring follow up. The response to PPI treatment is basically symptomatic i.e lower RSI scores, since the lesions or laryngealsigns (RFS) may take longer time to return to normal.
We had some limitations to our study. Firstly, this was a singlecentre study and patient population was relatively small. Also, we could not include a separate group of patients who can be subjected to 24hour pH monitoring for validation of RSI and RFS. In addition to this, post- treatment RFS could not be assessed in our study as it required longer follow-up period. However, further research with a longer follow up period of at-least 6 months can be done to determine changes in RFS post-treatment. Also, an amended RSI can be advised as a standard for each institute to decrease the patients’ difficulty in rating symptoms on an ordinal scale.
Conclusion
RSI & RFS scores of 7 & above can be considered as clinical indicators for assessment of severity of LPR which correlates well with RFS score when the RSI score is more than 13. We recommend that by using RSI alone in day to day practice in a developing country like India, the improvement of LPR patients following treatment with twice daily dosage of Proton pump inhibitors can be monitored well which in turn can reduce the cost and time consumed in regular treatment, restrict the injudicious use of PPIs and reserve further investigations for the non-responders.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the Indian national and institutional guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Bullet Point Summary
• Laryngopharyngeal Reflux is a very common yet underdiagnosed or over treated condition.
• 24-hour double probe pH monitoring is the gold standard to diagnose LPR but it is a costly and invasive investigation.
• Reflux Symptom Index and Reflux Finding Score introduced by Belafsky et al., in 2002 are validated tools to assess and treat LPR
• RFS takes longer time of atleast 6 months to come back to normal after treatment of LPR with Proton pump inhibitors.
• We recommend that pre-treatment RSI correlates well with RFS and RSI alone can be usedin an Indian scenario in order to assess patients with LPR symptoms and follow up after treatment.
References
- Belafsky P, Postma G, Koufman J. Validity and Reliability of the Reflux Symptom Index (RSI). J Voice.2002;16(2):274-277.PMID: 12150380.
- Vázquez de la Iglesia F, Fernández González S, de la Cámara Gómez M. Laryngopharyngeal Reflux: Correlation Between Symptoms and Signs by Means of Clinical Assessment Questionnaires and Fibroendoscopy. Is This Sufficient for Diagnosis?.ActaOtorrinolaringol Esp. 2007;58(9):421-425. PMID: 17999907.
- Reimer C, Bytzer P. Management of laryngopharyngeal reflux with proton pump inhibitors. TherClin Risk Manag.2008:4(1) 225–233. PMID: 18728712.
- Altman KW, Koufman JA. Laryngopharyngeal Reflux and Laryngeal Infections and Manifestations of Systemic Disease. Ballenger's Otolaryngology Head and Neck Surgery. 2009;17:893.
- Spantideas N, Drosou E, Bougea A, Assimakopoulos D. Laryngopharyngeal reflux disease in the Greek general population, prevalence and risk factors. BMC Ear, Nose and Throat Disord.2015; 15:7. PMID: 26696776.
- Saruç M, Aksoy E, Vardereli E, Karaaslan M, Çiçek B, İnce Ü, et al. Risk factors for laryngopharyngeal reflux. Eur Arch Otorhinolaryngol. 2012;269(4):1189-1194.
- Habermann W, Schmid C, Neumann K, Devaney T, Hammer HF. Reflux Symptom Index and Reflux Finding Score in Otolaryngologic Practice. J oice2011; 123-127. PMID: 21477986.
- Bhatia S, Reddy D, Ghoshal U, Jayanthi V, Abraham P, Choudhuri G, et al. Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: Report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol.2011;30(3):118-127. PMID: 21792655.
- Belafsky P, Postma G, Koufman J. The Validity and Reliability of the Reflux Finding Score (RFS). Laryngoscope. 2001;111(8):1313-1317.
- Nunes HS, Pinto JA, Zavanela AR, André Freitas Cavallini,Gabriel Santos Freitas,Fabiola Esteves Garcia. Comparison between the Reflux Finding Score and the Reflux Symptom Index in the Practice of Otorhinolaryngology. Int Arch Otorhinolaryngol. 2016;20:218–221. PMID: 27413402.
- Jaspersen, R Weber, C H Hammar, W Draf. Effect of omeprazole on the course of associated esophagitis and laryngitis. J Gastroenterol.1996; 31:765–767. PMID: 9027637.
- L P Leite, B T Johnston, D O Castell. Omeprazole for the treatment of posterior laryngitis. Am J Med.1995 Dec;99(6):694-5. PMID: 7503099.
- A J Eherer, W Habermann, H F Hammer, K Kiesler, G Friedrich, G J Krejs. Effect of pantoprazole on the course of reflux associated laryngitis: a placebo controlled double blind crossover study. Scand J Gastroenterol.2003; 38:462–467. PMID: 12795454.
- John M Wo, Jennifer Koopman, Steven P Harrell, Ken Parker, Welby-Winstead, Eric Lentsch. Double-blind placebo control trial with single dose pantoprazole for laryngopharyngeal reflux. Am J Gastroenterol. 2006;101:1972–1978. PMID: 16968502.
- Steward DL, Wilson KM, Kelly DH, Patil MS, Shwartzbauer HR, Long JD,et al. Proton pump inhibitor therapy for chronic laryngo-pharyngitis: a randomized placebo-control trial. Otolaryngol Head Neck Surg. 2004; 131:342–350. PMID: 15467597.