Isolated Genital Psoriasis - Rare and Disabling Location
Barbach Y*, Baybay H, Chaouche M, Dah Cherif A, Elloudi S, Mernissi FZ
Dermatology Department, University Hospital Hassan II, Morocco.
*Corresponding Author
Younes Barbach,
Dermatology Department,
University Hospital Hassan II, Morocco.
Tel: +212671797158
Fax: 0535613729
E-mail: dr.younes2011@gmail.com
Received: July 31, 2018; Accepted : October 03, 2018; Published: October 04, 2018
Citation: Barbach Y, Baybay H, Chaouche M, Dah Cherif A, Elloudi S, Mernissi FZ. Isolated Genital Psoriasis - Rare and Disabling Location. Int J Clin Dermatol Res. 2018;6(7):185-187. doi: dx.doi.org/10.19070/2332-2977-1800043
Copyright: Barbach Y© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Psoriasis is a chronic skin disease with a high impact on self-esteem and patients’ health-related quality of life. It is well known that the genital skin may be affected by psoriasis. However, little is known about the prevalence and clinical appearance of genital psoriasis, and genital skin is often neglected in the treatment of psoriatic patients. The evaluation of the impact on the quality of life of genital psoriasis is hampered by the difficulty of specifically assessing the severity of the disease. We report a case of exclusively genital psoriasis in a patient consulting mainly for an impairment of quality of life.
2.Abbreviations
3.Introduction
4.Observation
5.Discussion
6.Conclusion
7.References
Keywords
Genital Psoriasis; Isolated; Quality of Life; Rare; Erectile Dysfunction.
Abbreviations
PP: Plaque Psoriasis; GLs: Genital Lesions; PLs: Psoriatic Lesions; STDs: Sexually Transmitted Diseases; QoL: Quality of Life; PASI: Psoriasis Area Severity Index; BSA: Body Surface Area; PGA: Global Assessment Physician; PDI: Psoriasis Disability Index; IIEF: International Index of Erectile Function; SQOL-M: Sexual Quality of Life-Men.
Introduction
Psoriasis is a common chronic inflammatory skin disease affecting 0.5-4.6% of the world population [1]. The most common form of psoriasis is chronic plaque psoriasis (PP), characterized by well-demarcated plaques with a loosely adherent silvery-white scale. The lesions are typically distributed symmetrically on the scalp, elbows, knees, lumbosacral area, and in the body folds [2]. However, psoriasis may involve all sites of the body, most frequently, the genitals. There are limited epidemiological data on genital involvement in psoriasis. In most cases genital involvement is only a part of generalized PP, often of inverse psoriasis, although it may affect only the genitals in 2-5% of the patients. Recently Meeuwis et al., [3, 4] disclosed that frequency of genital involvement was 29-40%; however, in a subsequent study they illustrated that almost 46% of 1,943 patients reported genital lesions (GLs) at some time during the course of their skin disease.
We report a case of exclusively genital psoriasis in a patient consulting mainly for an impairment of quality of life.
Observation
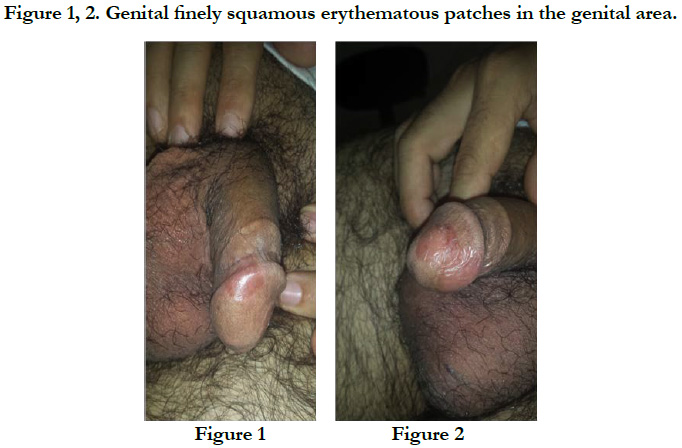
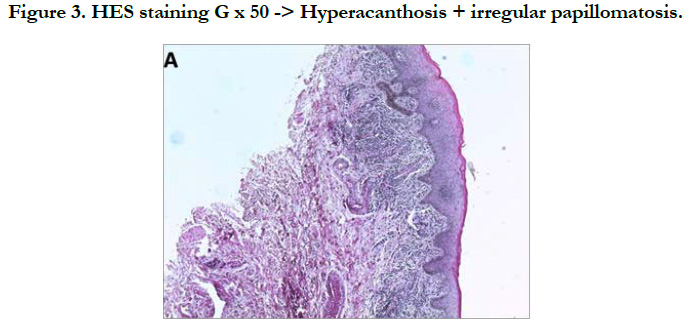
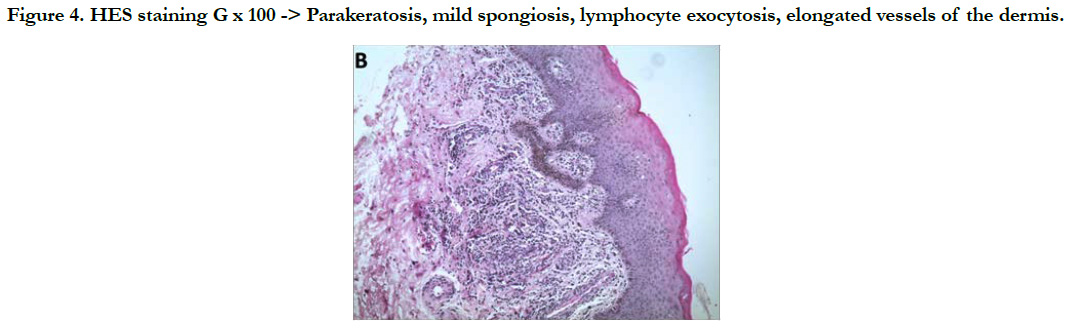
A 38-year-old man with no notable pathological history consulted for erythematous lesions in his newly-acquired glans (15 days) with a burning sensation, altering his life as a couple. The dermatological examination showed the presence of 2 finely squamous erythematous patches sitting respectively at the level of the glans and astride between the glans and the groove balano-preputial which are well limited with irregular edges making respectively 2.2 and 1.4 cm slightly infiltrated, not responding to the application of healing cream [Figure 1, 2]. The rest of the mucocutaneous examination was without particularity. In this symptomatology, Paget's disease, Bowen's disease, lichen planus and genital psoriasis had been mentioned. The latter has been confirmed by pathological examination [Figure 3, 4, 5]. The patient was treated with topical corticosteroids, with good clinical progress.
Figure 4. HES staining G x 100 -> Parakeratosis, mild spongiosis, lymphocyte exocytosis, elongated vessels of the dermis.
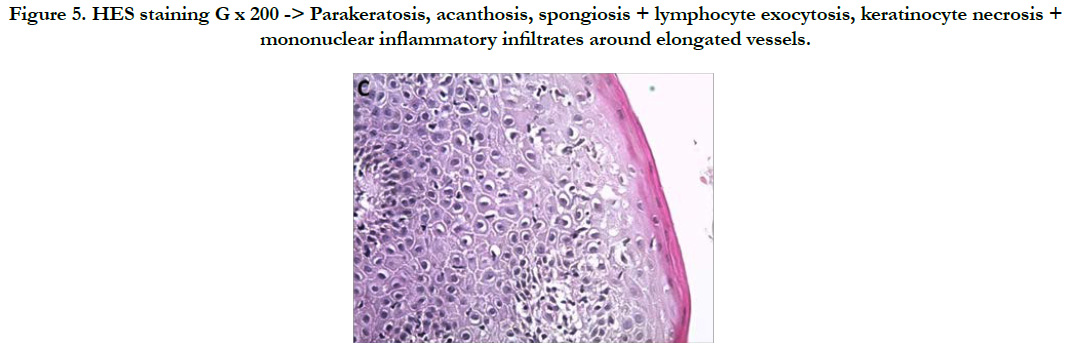
Figure 5. HES staining G x 200 -> Parakeratosis, acanthosis, spongiosis + lymphocyte exocytosis, keratinocyte necrosis + mononuclear inflammatory infiltrates around elongated vessels.
Discussion
The particular structure of the genital skin, which changes from stratified and keratinised squamous cell epithelium to mucosa, makes the psoriatic lesions (PLs) clinically different to the rest of the body. The skin lesions commonly present in the genital area as thin plaques, well demarcated and erythematous. The typical scales are often absent and when present, are minimal [4]. The diagnosis can be, in most cases, based on the clinical appearance of the lesions. However, vulvar and penile lesions frequently have an atypical appearance; in addition, the particular location sometimes makes it difficult to distinguish psoriasis from sexually transmitted diseases (STDs). When the clinical diagnosis of psoriasis may be difficult, a biopsy should be done [3].
Psoriasis involvement of the genital region can be uncomfortable and embarrassing for both men and women. The PLs can cause pain, itching, and burning sensation, furthermore it can determine a significant psychological impact. Patients with recurrent GLs experience significantly worse quality of life (QoL) and more sexual distress, when compared with patients without lesions.
The evaluation of the impact on the quality of life of genital psoriasis is hampered by the difficulty of specifically assessing the severity of the disease. The usual scores based notably on the extent of the lesions, such as the Psoriasis Area Severity Index (PASI), the body surface area (BSA) and the global assessment physician (PGA), are not adapted to the genital location whose surface does not represents one percent of body surface area.
A specific score was proposed in an open-label study to evaluate the efficacy and safety of tacrolimus ointment in the treatment of genital psoriasis in men [5]. The authors thus defined a genital PASI ranging from 0 to 72, defined by the formula (E + S + T) × A where E, S and T respectively correspond to erythema (erythema), desquamation (scaling) and infiltration (thickness) and A varies from 0 to 6 depending on the proportion of the genital area affected (excluding inguinal folds). This specific score, however, was not reused in new studies. The Europso study published in 2006, covering approximately 18,000 patients, showed a more significant decrease in quality of life assessed by an ordinal scale of 1 to 10 Psoriasis Disability Index (PDI) for psoriatic palsy: mean PDI of 5.35, reaching 6.08 in cases of genital involvement in men and women [6].
These results were confirmed by Meeuwis et al., in 2011, who sent a questionnaire to 1579 patients (men and women) members of the Dutch Psoriasis Association, aiming to assess their quality of life measured by the DLQI and the sexual repercussion, measured in men by two specific scores, Sexual Quality of Life Questionnaire for the use of Men (SQLQ-M) and the International Index of Erectile Function (IIEF) [7]. The analysis of the 487 responses (including 278 men) shows an impact on the quality of life more important in case of genital psoriasis (DLQI 8.5 vs 5.5, p < 0.0001). He also observes an impact of genital psoriasis on sexuality; resulting in a DLQI-related sexual dementia score (did your skin problem make your sex life difficult?) Higher in case of genital (p < 0.0001), without any difference in the two sexual disorder assessment questionnaires (SQLQ-M and IIEF).
Two other studies focused on the functional impact of psoriasis, but did not specifically assess the impact of genital psoriasis. The first, published by Chung et al., demonstrates a relationship between psoriasis and erectile dysfunction [8]. Goulding et al., Concluded that erectile dysfunction is more common in psoriatic men than in controls (men with non-psoriasis dermatosis), but psoriasis is not an independent risk factor for erectile dysfunction (unlike psoriasis). At age and at high blood pressure) [9]. More recently, patients have been dissatisfied with the specific management of their genital psoriasis by their doctor. Thus, a second publication on patients from the Dutch Psoriasis Association interviewed by Meeuwis et al., shows that 45% of patients with genital psoriasis did not tell their doctor, only 25% consider the doctor's attention to their genital psoriasis satisfactory and 67% never apply local treatment on their genital psoriasis [10].
Conclusion
Isolated genital psoriasis is a rare entity of psoriasis but with rather significant repercussions on quality of life in general and on sexuality in particular. Therefore, it is imperative that the dermatologist strives to specifically look for the existence of psoriatic genital involvement and to take care of it in a targeted way.
References
- Koo J. Population-based epidemiologic study of psoriasis with emphasis on quality of life assessment. Dermatol Clin. 1996 Jul;14(3):485-96. PubMed PMID: 8818558.
- Griffiths CE, Barker JN. Pathogenesis and clinical features of psoriasis. Lancet. 2007 Jul 21;370(9583):263-271. doi: 10.1016/S0140-6736(07)61128- 3. PubMed PMID: 17658397.
- Meeuwis KA, De Hullu JA, Massuger LF, Van De Kerkhof P, Van Rossum MM. Genital psoriasis: a systematic literature review on this hidden skin disease. Acta Derm Venereol. 2011 Jan;91(1):5-11. doi: 10.2340/00015555-0988. PubMed PMID: 20927490.
- Meeuwis KA, De Hullu JA, De Jager ME, Massuger LF, Van De Kerkhof PC, Van Rossum MM. Genital psoriasis: a questionnaire‐based survey on a concealed skin disease in the Netherlands. J Eur Acad Dermatol Venereol. 2010 Dec;24(12):1425-30. doi: 10.1111/j.1468-3083.2010.03663.x. PubMed PMID: 20384688.
- Bissonnette R, Nigen S, Bolduc C. Efficacy and tolerability of topical tacrolimus ointment for the treatment of male genital psoriasis. J Cutan Med Surg. 2008 Sep-Oct;12(5):230-4. PubMed PMID: 18845092.
- Dubertret L, Mrowietz U, Ranki A, Van De Kerkhof PC, Chimenti S, Lotti T, et al. European patient perspectives on the impact of psoriasis: the EUROPSO patient membership survey. Br J Dermatol. 2006 Oct;155(4):729-36. PubMed PMID: 16965422.
- Meeuwis KA, De Hullu JA, Van de Nieuwenhof HP, Evers AW, Massuger LF, Van de Kerkhof PC, van Rossum MM. Quality of life and sexual health in patients with genital psoriasis. Br J Dermatol. 2011 Jun;164(6):1247-55. doi: 10.1111/j.1365-2133.2011.10249.x. PubMed PMID: 21332459.
- Chung SD, Keller JJ, Chu TW, Lin HC. Psoriasis and the risk of erectile dysfunction: A population‐based case‐control study. J Sex Med. 2012 Jan;9(1):130-5. doi: 10.1111/j.1743-6109.2011.02510.x. PubMed PMID: 22023713.
- Goulding JM, Price CL, Defty CL, Hulangamuwa CS, Bader E, Ahmed I. Erectile dysfunction in patients with psoriasis: increased prevalence, an unmet need, and a chance to intervene. Br J Dermatol. 2011 Jan;164(1):103-9. doi: 10.1111/j.1365-2133.2010.10077.x. PubMed PMID: 20874856.
- Meeuwis KA, Van de Kerkhof PC, Massuger LF, De Hullu JA, Van Rossum MM. Patients’ experience of psoriasis in the genital area. Dermatology. 2012;224(3):271-6. doi: 10.1159/000338858. PubMed PMID: 22677898.