Scarry Tumors: Buschke- Löwenstein Tumor
Nassiri A*, Souhli OA, Tazi MF, Farih MF, Mernissi FZ
1 Department of Dermatology, Hassan II hospital, Fes, Morocco.
2 Urology Department, Hassan II hospital, Fes, Morocco.
*Corresponding Author
A. Nassiri,
Department of Dermatology, Hassan II hospital, Fes, Morocco.
E-mail: aichanassiri6@gmail.com
Received: February 28, 2018; Accepted : May 17, 2018; Published: May 21, 2018
Citation: Nassiri A, Souhli OA, Tazi MF, Farih MF, Mernissi FZ. Scarry Tumors: Buschke- Löwenstein Tumor. Int J Clin Dermatol Res. 2018;6(2):162-164. doi: dx.doi.org/10.19070/2332-2977-1800037
Copyright: Nassiri A© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
2.Material and Methods
2.1 Recurrence Evaluation
2.2 Surgical Management
2.3 Follow-up
3.Results
4.Discussion
5.Conclusion
6.References
Introduction
Buschke-Löwenstein tumor also called giant condyloma acuminatum, is a rare sexually transmitted disease [1]. Men are the most affected, but some cases were described in women [2].
It is usually an exophytic, ulcerative and cauliflower-shaped tumor. It can in filtrate the adjacent tissue.
The treatment is based on surgery, but relapses are very frequent.
Material and Methods
The search strategy employed MeSH terms and keywords designed to optimize the identification of randomized trials, guidelines, and systematic reviews on Buschke Löwenstein disease.
From January 2012 to December 2017, we dermatologists of hassan II hospital in Fez, conducted a prospective trial in collaboration with urologist of the same institution. The trial protocol was approved by the Institutional Ethical Committee of the Hassan II University Hospital. Informed, written consent of all participants was taken prior to enrolment.
We analyzed the result of primary surgery, long term survival, recurrences.
Recurrence was clinically evaluated and defined as the appearance of new condylomatous lesions.
A large resection involving subcutaneous fat was performed. Local treatments were applied with hydrocolloid dressing until complete recovery. All the tumors were excised and send to pathological examination to confirm the diagnosis.
We didn’t perform an HPV research because it’s not available in our laboratory.
Patients were examined 3 months after surgery and underwent a follow-up every 6 months. If the cutaneous defect was very important, the patients were seen monthly until complete recovery.
Pictures were taken for all the patient at the first time and in each follow-up.
All Data was noted on excel.
Results
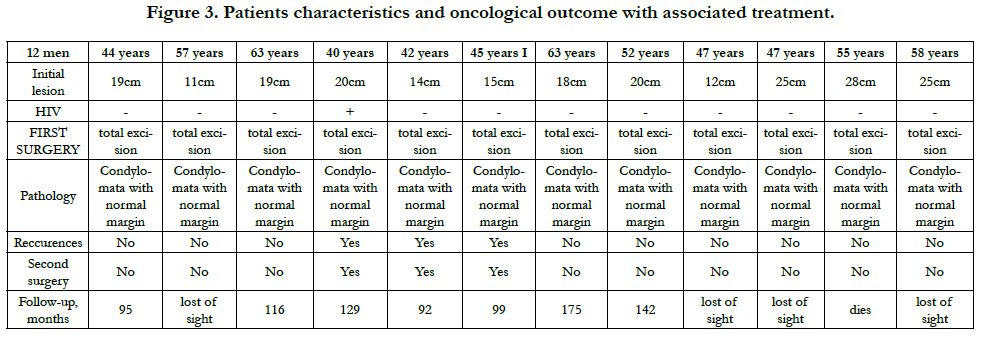
From January 2012 to December 2017, 12 patients were included. All of them were men with a mean age of 51 years (40-63). They all underwent a surgery within the genito-urinary area. All the patients were sexually active. Only two patient had a history of homosexuality. 6 patients were smokers and 4 were cannabis addict.
One patient was HIV seropositive.
In all patients, the tumors were exophytic, ulcerative cauliflower shaped, dotted with super infection sites. All the tumors were large with a minor tumor of 11 cm.
The localisation on genital area was constant. In 4 cases the tumor affected tighs and perianal area, in one case the tumors affected the neck area, and in one another it affected the back.
In pathology anatomy, all tumors were diagnosed to be giant condyloma acuminatum.
All our patient were treated by a large surgery with dressing until full recovery. In 2 patients we conducted a covering in a second time.
The follow-up was allowed in 7 patients. One patient died because of myocardial infarction during his hospital stay.
No surgical complications were noted.
A relapse was noted in 3 patients ,and it was treated by surgical revision.
The 5-year disease-free survival rate was 80%.
Discussion
First described by Abraham Buschke and Ludwig Löwenstein, Buschke-Löwenstein disease (BLD) was classified as a potential malignant condyloma acuminatum [3]. Then in 1979, Mohs and sahl included this disease into verrucous carcinoma category with oral florid papillomatosis and epithelioma cuniculatum [4].
It is a rare sexual transmitted disease that affects 0.1% of the population [5], which explains the limited number of the hospitalized cases in our trial.
Usually it affects men between 40 and 60 years [6] as in our study. A large panel of risk agents were described in literature, as smoking, immune deficiency, anaerobic infections, chronic inflammation [7]. In our trial we could prove that smoking and immune deficiency are closely related to development of Buschke-Löwenstein tumor.
Clinically, BLD, is found on the penis in 81% to 94% of cases and in 10% to 17 % in anorectal area [8]. Uretral area is describes in only 5% [9]. It can invade the cavernous body and urethra by creatinga fistula.
Histological examination of BLD shows a benign appearance as it is a pseudo-epitheliomatous proliferation characterized by exoand endophytic hyper papillomatos is with epithelial hyperplasia, hyperacanthosis and koilocytosis [10].
All the other sexual transmitted diseases hold be looked for, as we did in all our patients.
The prognosis of these tumors is conditioned by the incidence of local recurrence (60–70%) and the risk of malignant transformation [11].
The principal differential diagnosis is epithelioma spinocellular which can lead to dark prognosis [12].
Many treatments are discussed in literature as cryotherapy [13], carbondioxide and ND-YAG laser seems to be satisfying especially in small or lesions or as recurrence treatment [13]. Other topical treatments are used as podophyllin, 5-fluorouracil, bleomycin with cisplatin, acetic acid, imiquimod [13].
Photodynamic therapy using 5-aminolevulinic acid were also reported to allow 40% resolution, but it is not accessible in all centers [14].
But all these forms of treatment are either complementary to surgery or used in patients with limited biological resources.
The surgical treatment is the gold standard therapy. The tumor and the adjacent fat should be excised and margins should be tumors free [13]. CT scan and in sometimes MRI are required in order to evaluate the local disease extension.
The follow-up must be very close because the risk of relapse is very important. As we described it was seen in 3 patients of our trial.
Conclusion
BLD is a rare curable disease. If untreated precociously, it can have dramatic evolution as penectomy. The surgical treatment is the first step to recovery, since dressing and follow-up are necessary to complete recovery and to look for relapses that are very frequent.
References
- Spinu D, Rădulescu A, Bratu O, Checheriţă IA, Ranetti AE, Mischianu D. Giant condyloma acuminatum-Buschke-Lowenstein disease - a literature review. Chirurgia (Bucur). 2014 Jul-Aug;109(4):445-50. PubMed PMID: 25149605.
- Gole GN, Shekhar TY, Gole SG, Prabhala S. Successful treatment of Buschke-Löwenstein tumour by surgical excision alone. J Cutan Aesthet Surg. 2010 Sep;3(3):174-6. PubMed PMID: 21430832.
- Steffen C. The men behind the eponym-Abraham Buschke and Ludwig Lowenstein: giant condyloma (Buschke-Loewenstein). Am J Dermatopathol. 2006 Dec;28(6):526-36. PubMed PMID: 17122499.
- Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995 Jan;32(1):1-21. PubMed PMID: 7822496.
- Qarro A, Ali AA, Choho A, S Alkandry, Borki K. Buschke-Lowenstein tumor with anorectal localization: (About three cases). Ann Chir. 2005 Feb;130(2):96-100. PubMed PMID: 15737321.
- Martin F, Dalac S, Lambert D. Verrucous carcinoma: nosological situation, about four cases. Ann Dermatol Venereol. 1995;122(6-7):399-403. Pub- Med PMID: 8526420.
- Li AL, Walsh S, McKay DR. Surgical management of a giant condyloma of Buschke-Löwenstein in a patient with Netherton syndrome using the pedicled anterolateral thigh flap-a case report. J Plast Reconstr Aesthet Surg. 2011 Nov;64(11):1533-6. PubMed PMID: 21463975.
- Guillou M, Geniaux M, Mugnier C, Ferriere J, TexierL. Urethral location of a Buschke Lowenstein disease and a tumor of the urethra. J Urol Nephr. 1979;85:175-6.
- Dolanc R, Kocher T, Langer I, Marti WR, Pierer G, Harder F. Malignant transformation of perianal Buschke-Löwenstein tumor. Extensive abdominoperineal rectum excision and reconstruction with transpelvic myocutaneous rectus abdominis muscle flap. Chirurg. 2002 Apr;73(4):370-4. PubMed PMID: 12063923.
- Greif C, Bauer A, Wigger-Alberti W, et al. Giant condylomata acuminata (Buschke-Lowensteintumor). Dtsch Med Wochenschr. 1999;124:962-964.
- Fanget F, Pasquer A, Djeudji F, Chabanon J, Barth X. Should the Surgical Management of Buschke-Lowenstein Tumors Be Aggressive? About 10 Cases. Dig Surg. 2017;34(3):247-252. PubMed PMID: 27941342.
- Rivoire J. Malignant evolutionary potential of condylomata acuminata, called "Rooster crest" . J. Lyons. 1981;62:339-42.
- Della Valle A, Heguaburu M, Fresco R, Roldán G, Della Valle M. Buschke- Lowenstein tumor: case report and review with focus on therapeutic and psychological aspects. The Internet J Surg. 2007.
- Paoli J, Bratel AT, Löwhagen GB, Stenquist B, Forslund O, Wennberg AM. Penile intraepithelial neoplasia: results of photodynamic therapy. Acta Derm Venereol. 2006;86(5):418-21. PubMed PMID: 16955186.