Harlequin Ichthyosis: A Rare Case Report
Lahlou A*, Elmahi H, Gallouj S, Mernissi
Department of Dermatology, University Hospital Hassan II, Fez, Morocco.
*Corresponding Author
Asmae LAHLOU,
Department of Dermatology,
University Hospital Hassan II, Fez, Morocco.
E-mail: lahlouasmae@gmail.com
Received: March 02, 2017; Accepted : April 04, 2017; Published: April 29, 2017
Citation: Lahlou A, Elmahi H, Gallouj S, Mernissi FZ (2017) Harlequin Ichthyosis: A Rare Case Report. Int J Clin Dermatol Res. 5(3), 112-113. doi: http://dx.doi.org/10.19070/2332-2977-1700029
Copyright: Lahlou A© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
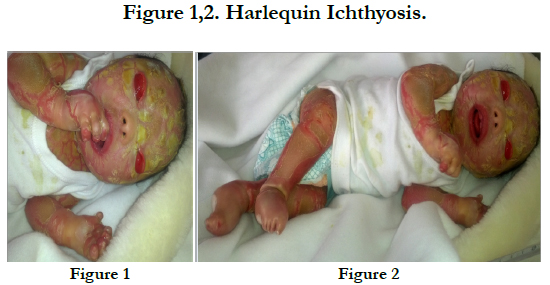
Harlequin fetus is a rare and the most severe genetic form of the congenital ichthyosis with an autosomal recessive inheritance. Incidence of the disease is nearly 1 in 3,00,000 live births. The disease might be lethal at birth and the affected babies are often premature. Harlequin ichthyosis [HI] is marked by severe keratinized and alligator-like horned skin. The present study reports a new case of harlequin fetus born to the consanguineous parents. He had the typical skin manifestations of thick armour like scales with fissures, complete ectropion and eclabium, atrophic and crumpled ears and swollen extremities. Supportive treatment was given but the neonate died on the 7th day. Adds to the collective knowledge of this rare skin disorder. HI has been linked to mutation in the ABCA12 gene; which cause a deficiency of the epidermal lipid transporter, resulting in hyperkeratosis and abnormal barrier function. Therefore, genetic counseling and mutation screening of this gene should be considered.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Harlequin Ichthyosis; Harlequin Fetus; Autosomal Recessive; Skin Abnormalities.
Introduction
Harlequin ichthyosis [HI] is a lethal disease [1, 2], but victims in very rare cases may survive for several months or years [3]. HI appears with severe thickened and scaly skin on the entire body. In addition, ectropion, lack of development of the external parts of the nose and ears, eclabium and open mouth, hypoplastic fingers, anonychia and mobility limitation of the joints are some other clinical features of the HI [2, 4, 5]. Patients are usually born prematurely and do not have any brain or internal organ abnormalities. If patients survive the neonatal period, they continue with a persistent ichthyosis form erythroderma for life. They are at high risk for hypo/hyperthermia, dehydration, respiratory distress, hypoventilation, malnutrition, hypernatremia, seizure, and skin infection [2, 6]. HI is associated with preterm birth and often leads to death due to neonatal complications such as fluid loss and septicemia [3].
We a new case of HI, who was a condidat treatment with isotretinoin but unfortunately died before starting treatment on day 7 of life.
Case Report
We report a new born with harlequin ichtyosis [HI] a product of consanguineous union. The maternal age was 35 years and paternal age was 40 years. Gestational age was 37 weeks of gestation based on both the first day of the last menstrual period and ultrasound. No remarkable complication was noted in the last ultrasound examination at 28 weeks of pregnancy. A female baby with HI was born via normal spontaneous vaginal delivery, This baby born at was weighing 3000 grams at birth. She was a eldest daughter and she died 7 days after birth. Clinical examination showed the typical features of HI with the presence of plaques thick armour like scales with fissures, complete ectropion, atrophic and crumpled ears and swollen extremities. The limbs remained in rigid semi-flexion (Figure 1, 2).
Discussion
HI is an extremely severe congenital form of ichthyosis that characterized by congenital epidermis abnormality [4, 5]. Mutations in the ABCA12 gene (Adenosine-triphosphate-Binding Cassette A12) have been reported in the majority of HI patients [4, 6]. This gene plays a major role in transporting lipids to cells that form the epidermis and the normal development of the skin [2]. HI is a rare disorder with the incidence of 1:300,000 births and more than 100 cases have been reported in the literature [1, 11, 12]. Most cases of HI have been recognized as having autosomal recessive inheritance although a dominant form may exist and sporadic cases occur frequently [12, 13] At birth, infants are covered with hard hyperkeratonic armor, composed of large, thick, yellowish brown, and very sticky plates [6, 7]. After birth, deep red fissures occur on these hard and inflexible plates that extend to the dermis, resulting in a joker-like skin. Infants with HI might have microcephaly, ectropion, and eclabium [4]. External auditory meatus and nostrils appear rudimentary and immature [8]. In addition, patients with HI have respiratory failure as a result of restricted chest expansion and skeletal deformities. Feeding problems may result in low blood sugar, dehydration, and kidney failure. In addition, temperature instability and infection would be common [4, 6]. Almost all these clinical features were observed in the current case he is probably has an autosomal recessive pattern given the fact that his parents showed consanguinity.
Prenatal diagnosis would be the first step for early detection of the disease. Therefore, obtaining the family history, consanguinity between the parents, and the presence of other skin disorders in offspring would be very helpful for early diagnosis of the disease [4]. Microscopic examination of the amniotic fluid cells and ultrasound for assessment of the shape of fetal mouth at 17 weeks of pregnancy might be useful for the early detection [9, 10]. Prenatal diagnosis can also be feasible using skin biopsy at 24 weeks of pregnancy, especially among the families with a history of HI. Although ultrasonography can be useful in some cases but it might not be applicable due to delayed phenotypic expression and the rarity of the disease [3]. Furthermore, sequence analysis of ABCA12 should be done first for the individuals with HI history [4].
Management of the neonate with HI includes the use of a humidified incubator, temperature regulation, nutrition replacement, pain control, and monitoring for infections [2]. Emollients should be applied liberally to the skin and bathing and soaking can reduce the risk of skin infection and promote shedding of the thickened skin. Eye care is critical and at least artificial tears should be initiated. If patients have contractures, surgical treatment may be necessary to prevent necrosis and gangrene formation of the distal fingers [2, 3]. Early systemic retinoid therapy (the majority starting treatment within the first week of life) leads to an increased survival rate (83%) compared to the survival rate without retinoid use [24%] [14] our case was died before starting isotretinoin.
Conclusion
Knowledge of the pathogenetic mechanisms is significant for the precise diagnosis, treatment, genetic counselling and prenatal diagnosis. In addition, genetic counseling and molecular investigation of the ABCA12 gene should be considered, especially in families with a consanguinity marriage.
References
- Arikan II, Harma M, Barut A, Harma MI, Bayar U (2010) Harlequin ichthyosis: A case report and review of literature. Anatolian J Obstet Gynecol. 1: 1–3.
- Hovnanian A (2005) Harlequin ichthyosis unmasked: A defect of lipid transport. J Clin Invest. 115(7): 1708–10.
- Hazuku T, Yamada K, Imaizumi M, Ikebe T, Shinoda K, et al., (2011) Unusual protrusion of conjunctiva in two neonates with Harlequin Ichthyosis. Case Rep Ophthalmol. 2(1): 73–7.
- Richard G, Bale SJ (1993) Autosomal Recessive Congenital Ichthyosis: GeneReviews ™ [Internet] Seattle (WA): University of Washington, Seattle.
- Fischer J (2009) Autosomal recessive congenital ichthyosis. J Invest Dermatol. 129(6): 1319–21.
- Kelsell DP, Norgett EE, Unsworth H, Teh MT, Cullup T, et al., (2005) Mutations in ABCA12 underlie the severe congenital skin disease harlequin ichthyosis. Am J Hum Genet. 76(5): 794–803.
- Hashemzadeh A, Heydarian F (2009) Harlequin Ichthyosis. ActaMedi Iran. 47(1): 81–2.
- Holden S, Ahuja S, Ogilvy-Stuart A, Firth HV, Lees C (2007) Prenatal diagnosis of Harlequin ichthyosis presenting as distal arthrogryposis using threedimensional ultrasound. Prenat Diagn. 27(6): 566–7.
- Shimizu A, Akiyama M, Ishiko A, Yoshiike T, Suzumori K, et al., (2005) Prenatal exclusion of harlequin ichthyosis; potential pitfalls in the timing of the fetal skin biopsy. Br J Dermatol. 153(4): 811–4.
- Zapalowicz K, Wygledowska G, Roszkowski T, Bednarowska A (2006) Harlequin ichthyosis-difficulties in prenatal diagnosis. J Appl Genet. 47(2): 195–7.
- Javed T, FaheemAfzal M, Iqbal Khan H (2005) Harlequin fetus: a case report. J Pak Assoc dermatol. 15: 348–350.
- Martin RJ, Fanaroff AA, Walsh AA (2011) Fanar off and Martin’s neonatal-perinatal medicine. (9th edn), United States, St Louis: Elsevier, Mosby. 1713-1714.
- Subinay M, Sammilani B, Debasish H (2009) Harlequin ichthyosis. The Internet j Pediatrics Neonatol. 9(2).
- Laura M Chang, Melissa Reyes (2014) A case of harlequin ichthyosis treated with isotretinoin. Dermatol Online J. 20(2): 7.