Our Experience of using Caudal Anesthesia in "Small" Surgical Interventions in Newborns
Nasibova EM1*, Polukhov R. Sh2, Ismailov IS3
1 Associate Professor of the Department of Pediatric Surgery, Azerbaijan Medical University, Azerbaijan.
2 Professor, Department of Rheumatology and Internal Diseases, Azerbaijan.
*Corresponding Author
Nasibova Esmira Mirza gizi,
Associate Professor, Department of Pediatric Surgery,
Azerbaijan Medical University, Azerbaijan.
Tel: +9940503366077
E-mail: doc.nasibova.esmira@gmail.com
Received: October 28, 2018; Accepted: November 22, 2018; Published: November 23, 2018
Citation: Nasibova EM, Polukhov R. Sh, Ismailov IS. Our Experience of using Caudal Anesthesia in "Small" Surgical Interventions in Newborns. Int J Anesth Res. 2018;6(8):543-544. doi: dx.doi.org/10.19070/2332-2780-18000109
Copyright: Nasibova EM© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim of the Study: To study the effectiveness of anesthesia with caudal administration of ropivacaine in combination with intravenous administration of propofol in new borns with "small" surgeries.
Material and Methods of the Study: The work was performed in the surgical clinic of the Azerbaijan Medical University. The study included 117 new borns operated on a one-sided or bilateral inguinal hernia, phimosis, paraphimosis and rectal atresia. After the patient completely fell asleep with propofol, a caudal block with ropivacaine was performed. The effectiveness of caudal anesthesia was assessed by hemodynamic indices and by the Robinson index, which was also called the "double product" or RPP (rate pressure product). To assess postoperative pain in newborns, we used the CRIES scale.
Results of the Study: When the caudal block was performed, no serious complications were noted in the newborn. Throughout the period of the surgical intervention (duration averaged from 30 minutes to 1.5 hours), the central hemodynamics index was stable, while the fluctuations of the studied parameters were insignificant in comparison with the initial data. No patient required intravenous administration of fentanyl. Assessment of pain on the scale CRIES showed that the maximum score was 0-4. And this indicates the absence of pain within 6 hours after the operation.
Conclusions:
1. Caudal blockade with ropivacaine provides effective anesthesia in new borns with "small" surgical interventions below the navel.
2. In neonates, a single caudal administration of ropivacaine at a dose of 3 mg/kg does not result in significant changes in hemodynamic parameters of the entire period of effective analgesia.
2.Material and Methods of Research
3.Results of the Study
4.Conclusions
5.References
Introduction
It has now been proven that caudal anesthesia is the safest and most effective way of anesthesia. To date, caudal anesthesia is the most commonly used technique for regional blockades in newborns. It is used alone or in combination with general anesthesia [1-4]. The advantages of the method include reliability (analgesia with an effective caudal block is provided in 98% of cases), safety (puncture of caudal space in children is the easiest access to the epidural space and, when properly performed, the danger of damage to the spinal cord and dura mater is extremely small) simplicity (easily perceived and mastered by trainees) [5-8]. Indications for caudal anesthesia are surgical interventions below the level of the navel (Th10).
Material and Methods of Research
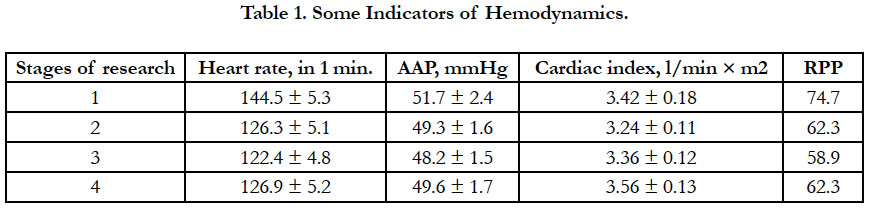
The work was carried out in the surgical clinic AMU. The study included 117 newborns operated on a one-sided or bilateral inguinal hernia, phimosis, paraphimosis and rectal atresia. The duration of operations was from 30 minutes to 1.5 hours. Induction of anesthesia was carried out by intravenous administration of propofol at a rate of 3 mg/kg. After the patient completely fell asleep, the caudal block was performed. The puncture of the caudal space was performed in the position of the patient on the left side with the lower extremities bent at an angle of 90° in the hip and knee joints. After puncturing the sacrococcygeal ligament at an angle of 60◦ to the skin, changing the angle of introduction by 45° advanced the needle into the sacral canal. Further, the presence or absence of blood, or cerebrospinal fluid in the pavilion of the needle, was determined. Only in the absence of the appearance of blood or cerebrospinal fluid from the needle to the latter was connected a plastic syringe with the medicine and an aspiration test was performed. If blood was not received during aspiration, then a test dose of ropivacin (0.5-1ml) was administered, after which the monitored parameters (HR, ECG, BP) were evaluated for 30-40 seconds. In the absence of electrocardiographic changes in the caudal space, the rest of the local anesthetic was injected slowly for 1.5-2 minutes. During anesthesia and surgery, standard monitoring was carried out in the following volumes: ECG, heart rate, blood pressure (non-invasive method), BH, SpO2. The effectiveness of caudal anesthesia was assessed by hemodynamic indices and by the Robinson index (SBP × HRC/100), which was also called the "double product" or RPP (rate pressure product). In 4 stages of the study: 1st stage, before surgery, 2nd stage before skin incision, 3rd stage: end of operation, application of cutaneous sutures, 4th stage: 6 hours after surgery (Table 1). An increase in RPP is a sign of a violation of baroreceptor control, which develops under stress of any origin (in particular pain). To assess postoperative pain in newborns, we used the CRIES scale. The total score on the CRIES scale is calculated as 58.9 the sum of the scores for 5 criteria (crying, oxygen therapy, increasing vital values, facial expression and sleep). The maximum score is 10, the minimum score is 0, the higher the score, the greater the pain.
Results of the Study
When the caudal block was performed, no serious complications were noted in the newborn. Thus, the accidental ingestion of a drug into a blood vessel did not have any consequences, since no further administration was made. Puncture of the dura during the execution of the caudal block occurs usually because of excessive penetration of the needle into the sacral canal, due to improper technique of conducting. In our practice, none of the patients noted this complication. Throughout the period of the surgical intervention (duration averaged from 30 minutes to 1.5 hours), the indices of central hemodynamics were stable, while the fluctuations of the studied parameters were insignificant in comparison with the initial data. No patient required intravenous administration of fentanyl.
At the first stage of the study, the parameters of central hemodynamics corresponded to their mean age values. In the second and third stages of the study (skin incision and end of operation), a decrease in heart rate was observed of 12.6% and 15.3%, of SBP 4.6% and 6.8%, respectively, and SI changes were unreliable (p <0.01). These changes are due to a sympathetic blockade caused by caudal administration of local anesthetics, which did not cause a significant decrease in SI. At the third stage of the study (6 hours after the operation), the hemodynamic parameters remained stable in the patients under study and did not differ significantly from the initial data, which was explained by the prolonged action of the caudal block with naropin. When analyzing the Robinson index in 4 stages of the study, as can be seen from the table, it became clear that the RPP values at the 2nd, 3rd and 4th stages of the study did not differ significantly from the data of the 1st stage. And this confirms the absence of pain at these stages of the study. Every hour for 6 hours after the operation period, the presence or absence of pain was traced. Assessment of pain on the scale CRIES showed that the maximum score was 0-4. And it shows the absence of pain during this period. It was also significant that almost all patients after the operation were switched to enteral nutrition, which is very important for newborns.
Conclusions
1. Caudal blockade with ropivacaine provides effective anesthesia in newborns with "small" surgical interventions below the navel.
2. In neonates, a single caudal administration of ropivacaine at a dose of 3 mg/kg does not result in significant changes in hemodynamic parameters of the entire period of effective analgesia.
References
- Aizenberg VL, Ulrich GE, Tsypin LE, Zabolotsky DV. Regional anesthesia in pediatrics. St. Petersburg: Synthesis of Beech; 2011. p. 304.
- Aizenberg VL, Ulrich GE, Tsypin LE, Zabolotsky DV. Regional anesthesia in pediatric vertebrology. Regionary anesthesia and treatment of acute pain. 2015;9(4):39-47.
- Kulagin AE. Kaudal anesthesia in pediatrics. Health. 2012;4:35-38.
- Sichkar S Yu. Epidural analgesia in newborns in the perioperative and postoperative period. Anesthesiology and resuscitation. 2015;3:65-68.
- Kim EM, Lee JR, Koo BN, Im YJ, Oh HJ, Lee JH. Analgesic efficacy of caudal dexamethasone combined with ropivacaine in children undergoing orchiopexy. Br J Anaesth. 2014 May;112(5):885-91. doi: 10.1093/bja/aet484. PubMed PMID: 24491414.
- Bösenberg AT. Epidural analgesia for major neonatal surgery. Paediatr Anaesth. 1998;8(6):479-83. PubMed PMID: 9836212.
- Locatelli B, Ingelmo P, Sonzogni V, Zanella A, Gatti V, Spotti A, et al. Randomized, double-blind, phase III, controlled trial comparing levobupivacaine 0.25%, ropivacaine 0.25% and bupivacaine 0.25% by the caudal route in children. Br J Anaesth. 2005 Mar;94(3):366-71. PubMed PMID: 15608043.
- O Raux, C Dadure, J Carr, A Rochette, X Capdevila. Pediatric caudal anesthesia. Update in anesthesia. 2010;26:32-36.