Ultrasound-Guided Caudal Block for Anal Canal Surgery: A Prospective Cohort Study
Adriana M Cadavid1*, Sandra M Martínez1, William H Joaqui1,2, Escobar J3, Botero J4, Mavarez-Martinez A5, Bergese SD5,6
Department of Anesthesiology and Reanimation, Intensive Care Department, Karadeniz Technical University, Trabzon, Turkey.
*Corresponding Author
Adriana Cadavid, MD,
Department of Anesthesiology, Universidad de Antioquia,
Hospital Universitario San Vicente Fundación, Medellin, Colombia.
Tel: (+57)310-458-7978
E-mail: adriana.cadavid@udea.edu.co
Received: September 25, 2018; Accepted: October 23, 2018; Published: October 25, 2018
Citation: Adriana M Cadavid, Sandra M Martínez, William H Joaqui, Escobar J, Botero J, Mavarez-Martinez A, et al., Ultrasound-Guided Caudal Block for Anal Canal Surgery: A Prospective Cohort Study. Int J Anesth Res. 2018;6(7):532-536. doi: dx.doi.org/10.19070/2332-2780-18000107
Copyright: Adriana M Cadavid© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Postoperative pain is an important symptom in patients after non-oncological anal canal surgery. A caudal block has shown to be an effective analgesic technique in this type of surgery, and ultrasound facilitates its performance and increases the rate of a successful block. We aimed to determine the effectiveness of ultrasound-guided caudal block (UGCB) in anesthesia and postoperative analgesia in patients scheduled for benign anal surgery.
Methods: This was a prospective interventional cohort study in adult patients who underwent benign anal surgery under UGCB. We evaluated the effectiveness of the intervention based on postoperative pain intensity measured with the numeric rating scale (NRS) at the following postoperative time points: 6, 12 and 24 hours. The following outcomes were included in our analysis: lower limbs motor block, urinary retention, rescue analgesia, and patient’s analgesia satisfaction.
Results: A total of 23 patients were included for data analysis. At least 65% of the study population reported none to mild pain (NRS ≤ 3) during the first 24 hours after surgery. None of the study patients experienced complete motor block in lower extremities or urinary retention. The mean time for patients to request the first rescue analgesia was 6.4 hours. The survey results indicated that 22 patients (95.7%) out of 23 were satisfied with the postoperative pain control.
Conclusions: UGCB is an effective, easy to perform intervention in patients with benign anal canal surgery. This technique offers an alternative multimodal pain control therapy with satisfactory analgesic effect and low rate of adverse events.
2.Abbreviations
3.Introduction
4.Materials and Methods
4.1 Study Population
4.2 Study Procedures
4.3 Statistical Analysis
5.Results
6.Discussion
7.Conclusion
8.Acknowledgment
9.References
Keywords
Caudal Anesthesia; Postoperative Pain; Anal Canal; Ultrasound; Ambulatory Surgery.
Abbreviations
UGCB: Ultrasound-Guided Caudal Block; NRS: Numeric Rating Scale.
Introduction
The prevalence of non-oncological anorectal diseases in adults inthe United States is 4% to 5% of the general population [1]. Of these, the most common diseases are hemorrhoids, anal fissure, anal fistula, and perirectal abscess [2]. Corrective surgery for anorectal diseases is associated with severe postoperative pain. In most cases, these procedures are performed on an ambulatory basis requiring adequate cost-effective anesthetic techniques, minimal adverse effects, and optimal analgesia in the immediate postoperative period [3].
Traditionally, several anesthetic and/or analgesic techniques have been used to perform anal canal surgeries, such as general anesthesia, spinal anesthesia, and perianal regional anesthesia with pudendal nerve block and/or caudal nerve block. Each of these techniques has a variable effect on the postoperative pain. The most commonly used in clinical practice is spinal anesthesia (subarachnoid), due to its anesthetic effectiveness and its analgesic efficacy up to six hours post-surgery [1].
Recent postoperative pain management guidelines for anal canal surgeries (e.g. hemorrhoidectomy) recommend the use of multimodal analgesia including non-steroidal anti-inflammatory drugs, paracetamol, and peripheral nerve blocks [3].
The caudal block used for this type of procedures has a documented increased rate of failure (up to 38%), related to anatomically guided needle insertion with no direct visualization. For this reason, the block it is not the first option when considering the analgesia management [4].
With the introduction of ultrasound-guided regional blocks, the success of these techniques increased significantly [5]. Ultrasound- guided caudal block (UGCB) is recently presented as a potentially effective option to achieve a higher rate of successful blocks, with effective anesthesia and longer postoperative analgesia and reduced side effects [6, 7].
In the surgical setting, the caudal block can be performed under direct ultrasound-guided visualization [8]. In addition, pharmacological development allows the use of adjuvants to the caudal block, such as dexamethasone, with prolonged analgesic effect and optimized postoperative pain control [9, 10].
A systematic search (Pubmed, Chrocrane, Embase, ScienceDirect) of this topic offered no information related to ultrasoundguided analgesic caudal technique for the clinical practice of patients undergoing anal canal surgery. In order to evaluate the effectiveness of UGCB to reduce pain after non-oncological anal canal surgery, we initiated a prospective interventional study in this patient population.
Materials and Methods
This was a prospective interventional study conducted on a cohort of patients undergoing anal canal surgery between November 2015 and May 2016 at Hospital Universitario San Vicente Fundación, Medellin, Colombia. The study protocol was approved by the institutional medical ethics committee and was also registered in ClinicalTrials.gov as NCT03345511. Informed consent was obtained from all study patients.
Patients were included in the study if they were aged between 18 and 70 years, diagnosed with an anal canal disease (hemorrhoids, anal fissure, anal fistula, or perirectal abscess) that required surgical intervention, willing to receive regional anesthesia guided by ultrasound. The exclusion criteria was applied to patients with limitations to understand study procedures (verbal communication impairment or cognitive dysfunction) and patients with a contraindication for neuroaxial nerve block (active infection in the puncture site, receiving anticoagulation or with coagulation disorders).
Preoperatively, inform consent was obtained, patients’ demographic characteristics were collected, and pain diary instructions were provided to participants (to be completed postoperatively).
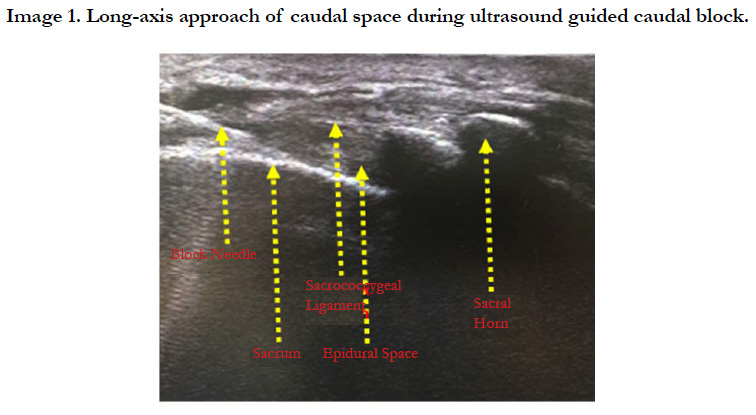
In operating room, patients’ perianal area was aseptically prepared and the skin was infiltrated with lidocaine 2% without epinephrine. Ultrasound Philips® portable scanner with a high frequency linear transducer (7-12MHz) was used to identify caudal epidural space (Image 1). An 18 gauge epidural needle (length 90mm) was used for direct injection with an admixture of bupivacaine 0.25% without epinephrine, lidocaine 1% without epinephrine, and dexamethasone 8 mg. For each patient, the total injected volume was calculated at 10 ml per meter of height [11]. All the UGCBs were erformed by two experienced anesthesiologists.
Intraoperatively, the following variables were measured: latency time to the block, presence of complete or partial lower extremities motor block, and optimal surgical conditions. The latency time was measured from the moment of direct injection administration until decrease of the stimulus sensation at the targeted area (prick test and temperature test with ice). Optimal surgical conditions were determined by the colorectal surgeon according to patient’s anal sphincter relaxation.
Postoperatively, the following variables were measure: pain intensity (at 6, 12, and 24 hours),time to request the first pain rescue medication, pain control satisfaction, and time to spontaneous urination. Pain intensity was measured according to a verbal 11-point numeric rating scale (NRS; 0 - 10). Analgesia efficacy was considered when the patients reported mild pain (NRS ≤3). Analgesia failure was considered when the patients reported moderate (NRS 4 - 6) or severe pain (NRS ≥ 7). Patient’s satisfaction with postoperative analgesia was evaluated with the Likert scale [12]. If patients were discharged sooner than 24 hours, they completed the pain diary at home and the results were collected by phone call at 24 hours.
Variables were summarized as means (standard deviations) for continuous variables and frequencies (percentages) for categorical variables. Results were reported as tables and charts. Normality of variables were performed by means of the Shapiro-Wilk test and homogeneity of variables (homoscedasticity) were performed by means of the Levene test. The database was collected in Microsoft Excel® and the software used to analyze the data was IBM SPSS Statistics, version 23.
Results
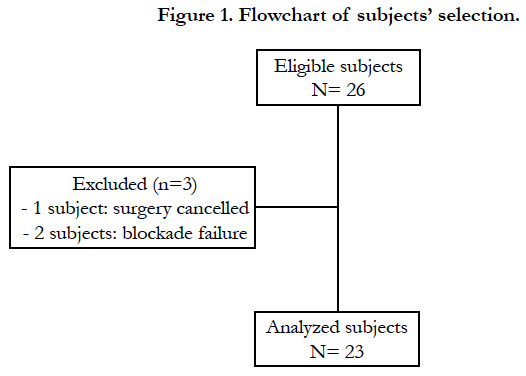
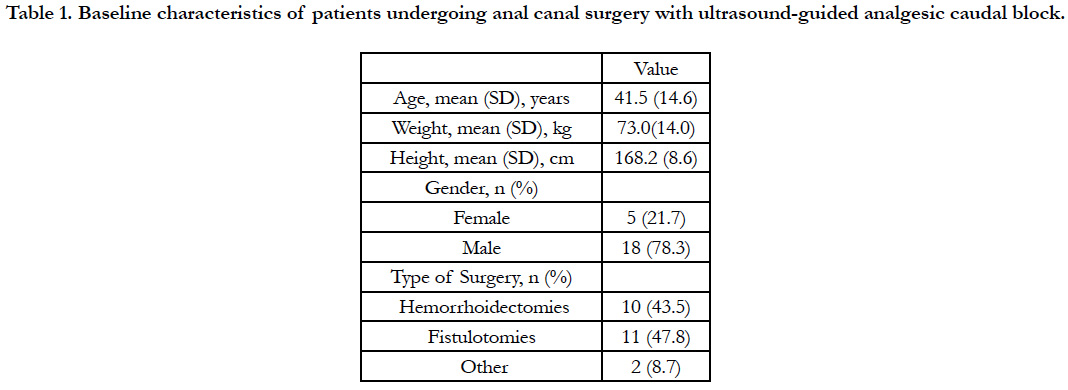
A total of 26 patients who underwent UGCB for anal canal surgeries were included in the study. From the total, 1 surgery was cancelled after blockade and 2 patients were excluded for nerve block failure (Figure 1). The 2/26 patients (7.7%) with unsuccessful nerve block represented the study block failure rate. Out of the 23 patients analyzed, 5 were females (21.7%) and 18 males (78.3%). The mean age was 41.5 ± 14.6years. The types of surgeries performed were: 10 hemorrhoidectomies (43.5 %), 11 fistulotomies (47.8%), and 2 others [1 anal fissurectomy, 1 anal condyloma resection] (8.7 %)(Table 1).
Table 1. Baseline characteristics of patients undergoing anal canal surgery with ultrasound-guided analgesic caudal block.
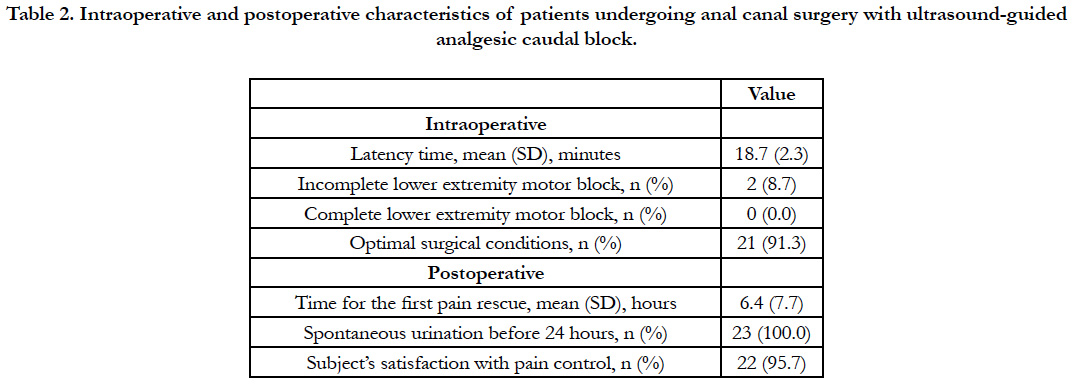
Intraoperatively, the mean latency time to achieve blockade of the pudendal area was 18.7 ± 2.3 minutes, with 22 out of 23 patients achieving blockade in ≤ 20 minutes. Lower incomplete extremity motor block was present in 2 patients(8.7 %) and no complete motor block was reported. Optimal surgical conditions, defined by the complete relaxation of the anal sphincter, were achieved on 22 patients (91.3%)(Table 2).
Table 2. Intraoperative and postoperative characteristics of patients undergoing anal canal surgery with ultrasound-guided analgesic caudal block.
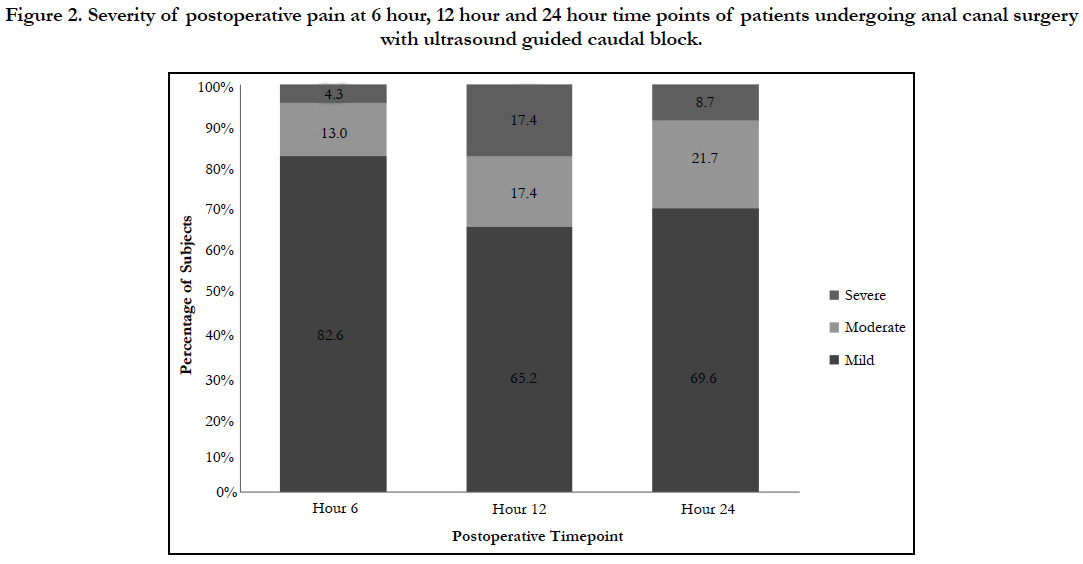
The following postoperative pain intensity scores were reported at the scheduled time points (Figure 2):
• At 6 hours: 19 patients mild (82.6%),3 moderate (13.0%), and 1 severe (4.3%).
• At 12 hours: 15 patients mild (65.2%), 4 moderate (17.4%), and 4 severe (17.4 %)
• At 24 hours:16 patients mild (69.6%), 5 moderate (21.7%), and 2 severe (8.7 %)
The mean time for the first rescue pain medication was 6.4 ± 7.7 hours. All the study patients had spontaneous urination before hour 24 (100.0 %), most of them with the first urination before 12 Hour and no longer than 20 Hour. Out of the 23 patients included in the study, 22 (95.7%) were satisfied with the analgesic technique used (Table 2).
Discussion
Postoperative pain experienced by patients undergoing anal canal surgeries is often severe despite the minor and ambulatory nature of the intervention; multimodal analgesia including a regional or neuroaxial block has been recommended for management. Spinal blockade is frequently used in association with other analgesics for anal canal surgery considering that as a monotherapy the blockade does not provide adequate postoperative analgesia [3].
In adults, regional anesthesia technique guided by anatomic structures has been abandoned due to the high failure rate of up to 38 % [4]. UGCB allows the correct needle positioning in the caudal space with identification of the structures that form and surround the sacral hiatus, significantly increasing the success rate [8]. In our study, the addition of ultrasound showed acaudal block failure rate of only 7.7 %.
To our knowledge, this is the first prospective interventional study where the UGCB is evaluated in a cohort of patients undergoing anal canal surgery, with satisfactory postoperative analgesia results and a low rate of blockade failure. We consider that UGCB facilitates the technique, with an observed latency time of <20 minutes, blocking the pudendal roots from S2 to S4 with sufficient innervation to the anal canal to allow optimal surgical conditions.
The use of dexamethasone as an addition of adjuvants to the local anesthetic for the caudal area is already documented to increase the duration of the blockade [9, 10]. The UGCB has potential benefits not only for the anal canal surgeries described in this study, but also for other types of surgeries of the pelvic territory (genital, prostate, pelvis, etc.) [13, 14].
One of the most frequents consequences of the spinal block technique used for anal canal surgeries is the lower extremities motor block within the first hours after surgery. Based on our study results, UGCB use facilitated patient’s recovery and fasterambulation in the postoperative period with no complete lower limbs motor block [2, 7, 12].
For our study cohort, an oral multimodal analgesic regimen was considered for the management of postoperative pain, including scheduled acetaminophen every 8 hours and tramadol 1mg/kg as needed. The mean time to request tramadol postoperatively was 6.4 hours. Notably, the percentage of patients experiencing severe pain (NRS ≥7) was low in all time points, contradicting the existing published evidence of severe pain when using conventional analgesia for this type of surgeries [3].
The time for first urination after surgery may be influenced by patient’s state of hydration (altered by the intestinal preparation required for surgery) and the preoperative fasting hours. These factors can lead to a fluid deficit, delaying the first postoperative urination [15]. However, no cases of urinary retention were reported in our study and first spontaneous urination occurred within the first 12 hours for the majority of the cohort.
For the two cases of caudal nerve block failure (7.7 %) anesthesia technique had to be converted to spinal. Although ultrasound optimized the success rate, predictors of difficulty have been described, such as the length of the sacrococcygeal ligament <17.6 mm and the depth of the sacral canal at the level of the apex of the sacral hiatus <3.7 mm(4). In our study, we did not perform these measurements.
It has been described that color Doppler during UGCB identifies the correct injection site, avoiding blood vessels [8, 16]. In our study, color Doppler was not used during the caudal injection procedure. Nevertheless, there were no signs of toxicity induced by local anesthetic.
Anecdotally, the hemorrhoidectomy procedure for one of the study patients lasted three hours with no required analgesic reinforcement. The combination of lidocaine 2% with bupivacaine 0.5% at equal proportions could influence the duration of the block. However, we do not recommend to use this technique in longer procedures.
The volume used for the nerve block in this cohort was based on previous studies in which ultrasound was not used for block guidance [11, 17]. Most patients achieved optimal surgical conditions and no complete blockage of the lower limbs was reported. This UGCB study showed high rate of successful block in anal canal surgery and satisfactory analgesia during the first 6, 12 and 24 hours postoperatively.
Our study had some limitations. First, the subject sample was relatively small, which may limit aspects such as the failure rate of the technique. And second, there was no control group to compare and/or to ensure a non-inferiority result of the UGCB. As the UGCB is an innovative technique for anesthesia and analgesia inanal canal surgeries, we consider this first cohort as an important preliminary experience and a base for future research proposals.
Conclusion
The UGCB is a highly effective anesthetic and analgesic option for anal canal surgery, with relatively easy application of ultrasound as a guide for a successful nerve block. With additional advantages over conventional techniques such as longer duration of analgesia, absence of complete motor block, and no urinary retention, UGCB favors a faster recovery after anal canal surgery.
Acknowledgment
These results have been presented as an abstract at the 9th World Congress of The World Institute of Pain (WIP).
References
- Gudaitytė J, Marchertienė I, Pavalkis D. Anesthesia for ambulatory anorectal surgery. Medicina (Kaunas). 2004;40(2):101-11. PubMed PMID: 15007268.
- Castillo E, Margolin DA. Anal fissures: diagnosis and management. Tech Gastrointest Endosc. 2004 Jan 1;6(1):12-6.
- Joshi GP, Neugebauer EA. Evidence‐based management of pain after haemorrhoidectomy surgery. Br J Surg. 2010 Aug;97(8):1155-68. doi: 10.1002/ bjs.7161. PubMed PMID: 20593430.
- Kim YH, Park HJ, Cho S, Moon DE. Assessment of factors affecting the difficulty of caudal epidural injections in adults using ultrasound. Pain Res Manag. 2014 Sep-Oct;19(5):275-9. PubMed PMID: 25111987.
- Nikooseresht M, Hashemi M, Mohajerani SA, Shahandeh F, Agah M. Ultrasound as a screening tool for performing caudal epidural injections. Iran J Radiol. 2014 May;11(2):e13262. doi: 10.5812/iranjradiol.13262. PubMed PMID: 25035698.
- Najman IE, Frederico TN, Segurado AV, Kimachi PP. Caudal epidural anesthesia: an anesthetic technique exclusive for pediatric use? Is it possible to use it in adults? What is the role of the ultrasound in this context?. Rev Bras Anestesiol. 2011 Jan-Feb;61(1):95-109. doi: 10.1016/S0034-7094(11)70011-3. PubMed PMID: 21334512.
- Apan A, Cuvas O. Caudal block in adults: new horizons with ultrasound. Minerva Anestesiol. 2013 Dec;79(12):1332-3. PubMed PMID: 23839326.
- Yoon JS, Sim KH, Kim SJ, Kim WS, Koh SB, Kim BJ. The feasibility of color Doppler ultrasonography for caudal epidural steroid injection. Pain. 2005 Nov;118(1-2):210-4. PubMed PMID: 16213088.
- Thomas S, Beevi S. Epidural dexamethasone reduces postoperative pain and analgesic requirements. Can J Anaesth. 2006 Sep;53(9):899-905. PubMed PMID: 16960268.
- Kim EM, Lee JR, Koo BN, Im YJ, Oh HJ, Lee JH. Analgesic efficacy of caudal dexamethasone combined with ropivacaine in children undergoing orchiopexy. Br J Anaesth. 2014 May;112(5):885-91. doi: 10.1093/bja/aet484. PubMed PMID: 24491414.
- Kiribayashi M, Inagaki Y, Nishimura Y, Yamasaki K, Takahashi S, Ueda K. Caudal blockade shortens the time to walking exercise in elderly patients following low back surgery. J Anesth. 2010 Apr;24(2):192-6. doi: 10.1007/s00540-009-0840-6. PubMed PMID: 20084409.
- Cesur M, Yapanoglu T, Erdem AF, Ozbey I, Alici HA, Aksoy Y. Caudal analgesia for prostate biopsy. Acta Anaesthesiol Scand. 2010 May;54(5):557-61. doi: 10.1111/j.1399-6576.2009.02168.x. PubMed PMID: 19919580.
- Schloss B, Martin D, Tripi J, Klingele K, Tobias JD. Caudal epidural blockade for major orthopedic hip surgery in adolescents. Saudi J Anaesth. 2015 Apr-Jun;9(2):128-31. doi: 10.4103/1658-354X.152832. PubMed PMID: 25829898.
- Wang J, Zhou H, An W, Wang N, Gao Y. Effective concentration of lidocaine plus fentanyl for caudal block in patients undergoing transrectal ultrasound guided prostate biopsy. Pain Res Treat. 2016;2016:5862931. PubMed PMID: 27872761.
- Lee SY, Kang SB, Kim DW, Oh HK, Ihn MH. Risk factors and preventive measures for acute urinary retention after rectal cancer surgery. World J Surg. 2015 Jan;39(1):275-82. doi: 10.1007/s00268-014-2767-9. PubMed PMID: 25189452.
- Tsui B, Leipoldt C, Desai S. Color flow Doppler ultrasonography can distinguish caudal epidural injection from intrathecal injection. Anesth Analg. 2013 Jun;116(6):1376-9. doi: 10.1213/ANE.0b013e31828e5e93. PubMed PMID: 23558836.
- Yokoyama M, Hanazaki M, Fujii H, Mizobuchi S, Nakatsuka H, Takahashi T, et al. Correlation between the distribution of contrast medium and the extent of blockade during epidural anesthesia. Anesthesiology. 2004 Jun;100(6):1504-10. PubMed PMID: 15166571.