Ossification of the Posterior Longitudinal Ligament: A Case Report of Difficult Intubation in a Resource Limited Setting
Baral BK1, Poudel PR1, Regmi S1, Yadav A1, Jense RJ2*
1 Department of Anaesthesiology and Intensive care, National Academy of Medical Sciences, Bir Hospital: Kathmandu, Nepal.
2 Department of Anesthesiology & Pain Medicine, University of Washington: Seattle, USA.
*Corresponding Author
Ryan J. Jense MD,
Department of Anesthesiology & Pain Medicine,
University of Washington: Seattle, USA.
Tel: 206-755-9119
E-mail: rjjense@uw.edu
Received: May 24, 2018; Accepted: June 20, 2018; Published: June 21, 2018
Citation: Baral BK, Poudel PR, Regmi S, Yadav A, Jense RJ. Ossification of the Posterior Longitudinal Ligament: A Case Report of Difficult Intubation in a Resource Limited Setting. Int J Anesth Res. 2018;6(5):523-525. doi: dx.doi.org/10.19070/2332-2780-18000105
Copyright: Ryan J. Jense© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Ossification of the posterior longitudinal ligament (OPLL) is a rare and often unrecognized cause of difficult intubation that is most commonly found in elderly Asian males. This case report will describe the airway management of such a patient with severely limited neck mobility.
A 66-year-old male with diabetes and hypertension presented with ongoing neck pain over three years and new progressive weakness in all extremities over the last two months. Neurological examination revealed mild spastic paresis and hyperreflexia in both upper and lower extremities. Neck movement was severely restricted and radiographic evidence supported the finding of OPLL.
A challenging airway was anticipated and management plans were discussed in advance. A difficult intubation set containing a video laryngoscope and a fiberoptic bronchoscope were prepared for the case. Conventional laryngoscopy was avoided due to severely limited neck mobility and the risk of causing trauma to the spine. The trachea was successfully intubated using video laryngoscopy without manipulation of the cervical spine. The patient underwent a successful posterior decompressive laminectomy with posterior lateral mass screw fixations at C2-C6.
OPLL is a rare cause of difficult intubation that can pose a challenge to anaesthesia providers, especially in resource limited settings. Preoperative evaluation and appropriate airway preparation is essential. Our case demonstrates that video laryngoscopy can be a great choice for the management of difficult airways in such patients.
2.Abbreviations
3.Introduction
4.Case Presentation
5.Discussion
6.Conclusion
7.References
Keywords
Difficult Airway; Video Laryngoscopy; OPLL.
Abbreviations
OPLL: Ossification of the Posterior Longitudinal Ligament.
Introduction
Ossification of the posterior longitudinal ligament (OPLL) results from the process of progressive calcification within the ligament. Although it can occur anywhere along the vertebral column, the most common location is the cervical spine. Such pathology can cause spinal cord compression leading to cervical neuropathy, and it may also severely limit neck mobility [1].
The purpose of this case-report is to highlight an uncommon cause of difficult intubation and describe the airway management techniques that were employed.
Case Presentation
A sixty-six-year-old 64 kg gentleman presented with complaints of neck pain over the past three years. The pain was dull-aching in nature and exacerbated by forward bending of neck. He also reported progressive weakness in all limbs causing difficulty walking over the past two months. He has been treated for hypertension for twelve years and diabetes mellitus for the last five years. He reports no history of trauma.
He was average build, but unable to stand. Strength was 2/5 in the arms and 3/5 in the legs bilaterally. Marked hypertonicity was noted bilaterally in both upper and lower limbs. Sensory examination was unremarkable.
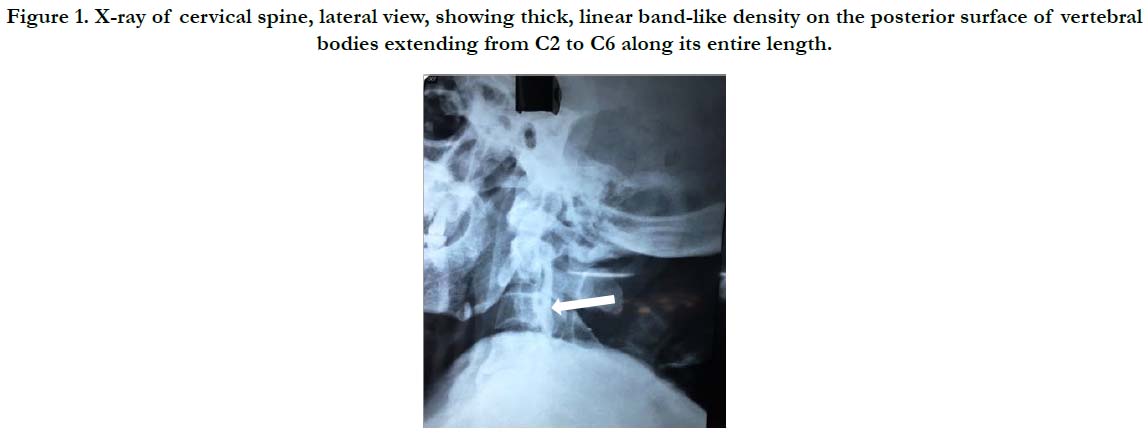
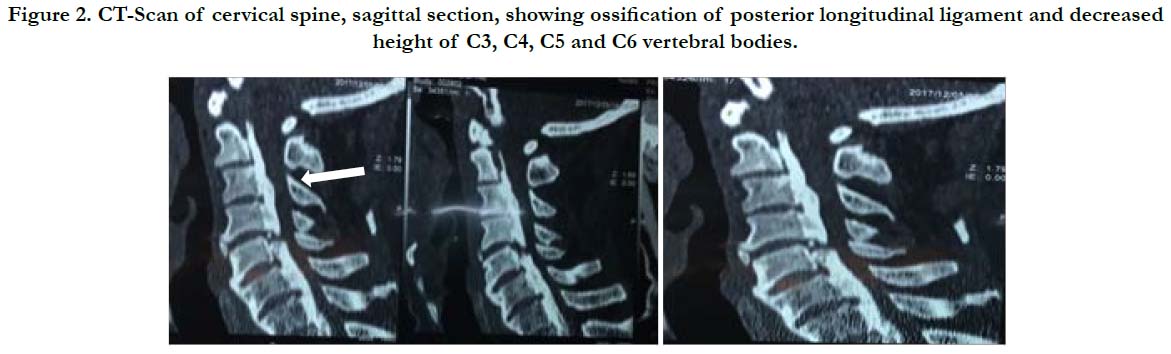
X-rays of the lateral cervical spine revealed a linear band of ossified tissue along the posterior margin of the vertebral bodies extending between C2 and C6 (Figure 1). There was loss of cervical lordosis. CT scan revealed: cervical spondylosis with degenerative disc disease, hypertrophy of PLL at C2-C6 vertebral body causing indentation of anterior thecal sac and spinal cord with narrowing of lateral recesses and spinal canal, and decreased height of C3-C6 vertebral bodies (Figure 2).
Airway evaluation revealed adequate mouth opening, Mallampati Class II, and severely limited neck mobility with an atlanto-occipital angle less than 12 degrees. Laboratory parameters were within normal limits. The patient was considered to be American Society Anesthesiologists physical status II, and was scheduled for C2-C7 laminectomy and C3-C7 lateral screw fixation.
After obtaining written informed consent, standard monitors were applied. An intravenous line was secured, and central venous and arterial lines were inserted for possible hemodynamic instability and vasopressor use.
Anticipating a difficult airway with concerns for cervical neurologic injury, our primary plan was to perform a routine IV induction with muscle relaxation, and then secure the airway with an oral endotracheal tube using video laryngoscopy. Fiberoptic intubation was the backup plan.
A difficult airway cart was secured. The patient was adequately preoxygenated with 100% oxygen, and general anesthesia was induced (Propofol 100 mg, Fentanyl 130 mcg, and Succinylcholine 100 mg). Following induction, video laryngoscopy was performed in the neutral position without manipulation of the cervical spine. The anteriorly located vocal cords were visualized with some difficulty, but the trachea was intubated with a 7.5mm internal diameter cuffed flexometallic endotracheal tube.
The patient was placed in the prone position, and the surgical procedure was performed without incident. Following 120 minutes of operative time, the patient was extubated awake and transferred to the postoperative ward.
Discussion
The incidence of OPLL is low, and is reported to be 2.4% in the Asian population and 0.16% in Caucasians [2, 3]. OPLL is most common in Japanese, Koreans and Chinese populations [4].
This pathology was first described in 1839 by Key, and termed OPLL in 1964 by Terayama et al., [5]. It is most commonly found in males in the 5th to 6th decades of life, and can result in the narrowing of the spinal canal lumen, cord compression, and neurological dysfunction [2, 6].
As neck stiffness is one of the most commonly reported symptoms of OPLL, it can thus present a challenge to the anaesthesiologist regarding airway management using conventional laryngoscopy [7, 8]. As a result of severely limited range-of-motion of the neck, it can be nearly impossible to obtain the alignment of the oral, pharyngeal, and laryngeal axes for conventional laryngoscopy [9], especially in a patient with an atlanto-occipital extension of less than 12 degrees.
Furthermore; our patient had calcification in five contiguous cervical intervertebral spaces, indicating severe disease and thus posed a risk of cervical spine fracture with even minor trauma. We were thus challenged to use an unconventional technique to secure the airway, and were ultimately successful using video laryngoscopy following appropriate anesthetic induction.
We find it worth mentioning that due to the shape of the King Vision laryngoscope, it was difficult to initially insert the video laryngoscope. Thus, the disposable blade had to be disconnected from the reusable display unit and then inserted into the oral cavity. Once in place, it was connected with the display unit and laryngoscopy was performed. This did create the possibility for a bad outcome to occur during intubation, and it does open the possibility for improved designs of such devices so that they can function even better in challenging situations.
Conclusion
Common causes of cervical spine abnormalities are found in patients with rheumatoid arthritis, osteoarthritis, traumatic injury, and other bony abnormalities such as ankylosing spondylitis. OPLL is yet another cause of cervical spine abnormality that can confront anesthesia providers with the potential for difficult intubations.
In any circumstance in which a provider might face a difficult airway, it is important that they are ready to employ secondary techniques when securing the airway. While awake fiberoptic intubation has been considered the primary choice for anticipated difficult airway management [10], newer generations of airway devices such as video laryngoscopes can allow the anaesthesia provider to facilitate endotracheal intubation by indirect visualization of the glottis without the need to align the oral, pharyngeal and laryngeal axes [11].
We would like to ensure that video laryngoscopy is considered when making decisions about difficult airways, and would also like to add that it might be the rescue device of choice. Importantly; this is a less expensive more sustainable option that can be very useful in resource limited settings like Nepal - where fiberoptic bronchoscopes and the accompanying infrastructure are not readily available.
Finally, while management of the airway in patients with cervical OPLL is challenging, gentle atraumatic intubation without manipulation of the neck should be the cornerstone of airway management for all patients.
References
- Nishida N, Kanchiku T, Kato Y, Imajo Y, Yoshida Y, Kawano S, et al. Cervical ossification of the posterior longitudinal ligament: biomechanical analysis of the influence of static and dynamic factors. J Spinal Cord Med. 2015 Sep;38(5):593-8. doi: 10.1179/2045772314Y.0000000221. PubMed PMID: 24964955.
- Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 1984 Apr;(184):71-84. PubMed PMID: 6423334.
- Wang MY, Thambuswamy M. Ossification of the posterior longitudinal ligament in non-Asians: demographic, clinical, and radiographic findings in 43 patients. Neurosurg Focus. 2011 Mar;30(3):E4. PubMed PMID: 21434820.
- Lee T, Chacha PB, Khoo J. Ossification of posterior longitudinal ligament of the cervical spine in non-Japanese Asians. Surg Neurol. 1991 Jan;35(1):40-4. PubMed PMID: 1898499.
- Terayama K, Maruyama S, Myashita R, Minai K, Kirosheta M, Shimizu Y, et al. Ossification of the posterior longitudinal ligament in the cervical spine. Orthop Surg. 1964;15:1083-95.
- Forestier J, Lagier R. Ankylosing hyperostosis of the spine. Clin Orthop Relat Res. 1971 Jan;74:65-83. PubMed PMID: 4993095.
- Mashour GA, Stallmer ML, Kheterpal S, Shanks A. Predictors of difficult intubation in patients with cervical spine limitations. J Neurosurg Anesthesiol. 2008 Apr;20(2):110-5. doi: 10.1097/ANA.0b013e318166dd00. PubMed PMID: 18362772.
- Calder I, Calder J, Crockard HA. Difficult direct laryngoscopy in patients with cervical spine disease. Anaesthesia. 1995 Sep;50(9):756-63. PubMed PMID: 7573863.
- Horton WA, Fahy L, Charters P. Disposition of cervical vertebrae, atlantoaxial joint, hyoid and mandible during x-ray laryngoscopy. Br J Anaesth. 1989 Oct;63(4):435-8. PubMed PMID: 2818921.
- Thompson C, Moga R, Crosby ET. Failed videolaryngoscope intubation in a patient with diffuse idiopathic skeletal hyperostosis and spinal cord injury. Can J Anaesth. 2010 Jul;57(7):679-82. doi: 10.1007/s12630-010-9313-5. PubMed PMID: 20428989.
- Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway, An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013 Feb;118(2):251-70. doi: 10.1097/ALN.0b013e31827773b2. PubMed PMID: 23364566.