An Anesthetic Approach for a Patient with Known Difficult Airway Undergoing an Ommaya Reservoir Placement
Ellwood S1, Amin M2*, Chaudhry F3, Bekker A4
1 Medical Student, Rutgers New Jersey Medical School, Newark, USA.
2 Resident Physician, Department of Anesthesiology & Perioperative Medicine, Rutgers New Jersey Medical School, Newark, USA.
3 Assistant Professor, Cardiothoracic Anesthesia, Department of Anesthesiology & Perioperative Medicine, Rutgers New Jersey Medical School, Newark, USA.
4 Chairman, Professor of Anesthesiology, Department of Anesthesiology & Perioperative Medicine, Rutgers New Jersey Medical School, Newark, USA.
*Corresponding Author
Molly Amin, MD,
Department of Anesthesiology & Perioperative Medicine,
Rutgers New Jersey Medical School, PO Box 1790, MSB-E547,
Newark, NJ 07101-1709, USA.
Tel: 973-972-0470
Fax: 973-972-3835
E-mail: ma1222@njms.rutgers.edu
Received: May 01, 2018; Accepted: May 21, 2018; Published: May 22, 2018
Citation: Ellwood S, Amin M, Chaudhry F, Bekker A. An Anesthetic Approach for a Patient with Known Difficult Airway Undergoing an Ommaya Reservoir Placement. Int J Anesth Res. 2018;6(4):520-522. doi: dx.doi.org/10.19070/2332-2780-18000104
Copyright: Amin M© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
We describe the anesthetic management of a patient with a known difficult airway secondary to a tumor in the oropharynx in need of an Ommaya Reservoir. The surgical team preferred to perform the procedure under monitored anesthesia care to avoid manipulation of the patient’s airway due to the possibility of dislodging friable tissue. We report the successful use of local anesthesia and dexmedetomidine infusion, as the primary sedative agent for intraoperative management of this patient.
2.Abbreviations
3.Introduction
4.Case Report
5.Discussion
6.Conclusion
7.References
Keywords
Dexmedetomidine; Difficult Airway; Monitored Anesthesia Care.
Abbreviations
OR: Ommaya Reservoir; CNS: Central Nervous System; MAC: Monitored Anesthesia Care; TIVA: Total Intra-Venous Anesthesia; LMA: Laryngeal Mask Airway; AC: Awake Craniotomies.
Introduction
The Ommaya reservoir (OR) was initially used for the management of fungal meningitis [1]. Now, the OR is used in the management of a variety of central nervous system (CNS) pathologies, including infections, benign and neoplastic lesions, as well as in the delivery of intrathecal chemotherapy [2, 3].
From an anesthetic perspective, the insertion of an OR can be a relatively minor intracranial procedure with proper patient selection and preparation. The anesthetic techniques used for an OR placement include general endotracheal anesthesia, monitored anesthesia care (MAC) and total intravenous anesthesia (TIVA), all with or without a scalp block. The chosen anesthetic technique is mostly dependent on the preferred location of the OR and the anatomical challenges faced to achieve proper placement. However, it should be noted that an anticipated or known difficult airway is a relative contraindication to performing an OR placement [4].
Currently, there is no consensus on the best anesthetic management for an OR placement with a known difficult airway. Furthermore, the ideal anesthetic management of neurosurgical patient with a relative contraindication, like a difficult airway, remains ambiguous [3, 5]. We are reporting the successful use of both local anesthetic and dexmedetomidine infusion as the primary sedative agents for the insertion of an OR on a patient with a known difficult airway.
Case Report
A 52-year-old male (63 kg) with a history of hypertension, AIDS, hepatitis C, and plasmablastic lymphoma involving the left side of the head/neck in need of intrathecal chemotherapy was scheduled for an insertion of a right frontal OR utilizing the StealthStation™ surgical navigation system due to small ventricle size and difficult anatomy.
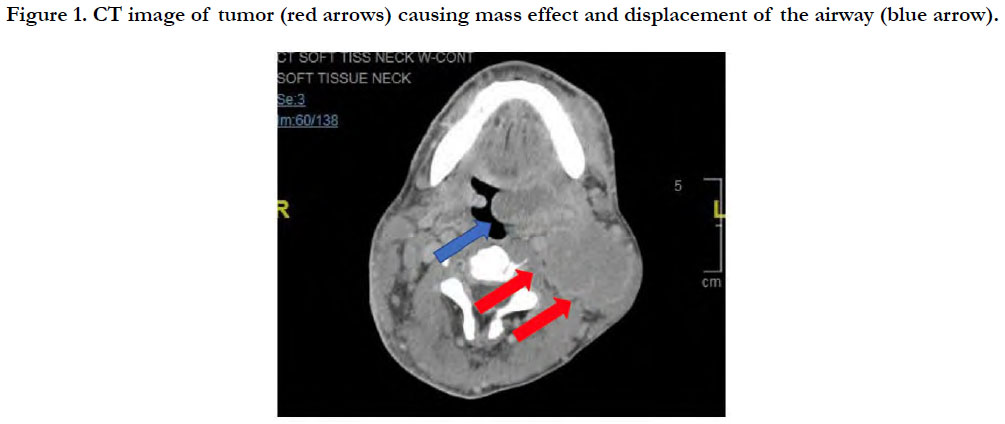
CT imaging showed a large infiltrative mass in the left masticator space with diffuse infiltration of the medial/lateral pterygoid and masseter muscles. Mass extension included the buccal space, nasopharyngeal/oropharyngeal soft tissues, and the left palatine tonsil. The oropharyngeal airway was narrowed due to mass effect at the base of the tongue (Figure 1).
Anesthetic history was significant for a recent difficult fiberoptic intubation for a cervical lymph node biopsy two weeks prior to this procedure. The fiberoptic intubation was challenging due to the large friable mass, which made glottic visualization difficult. Several attempts were required prior to successful intubation.
Airway evaluation demonstrated a Mallampati class IV with a large left-sided ulcerated cheek mass. Examination also demonstrated a thyromental distance 3 fingerbreadths, a two finger breadth mouth opening and a full range of motion of the neck.
A thorough discussion regarding the intraoperative airway management plan was had preoperatively with the patient, and it was decided that if the patient’s airway condition deteriorated rapidly, a surgical airway would be performed by ENT.
Given the history of difficult fiberoptic intubation, a decision was made to proceed under monitored anesthesia care. Standard ASA monitors, a nasal cannula with 4L/min O2 and end tidal carbon dioxide monitoring were applied. ENT surgeons were present in the operating room with their equipment ready if an emergent tracheostomy needed to be performed. 0.4 mg of glycopyrrolate, 4 mg of ondansetron, 2 mg of midazolam, and loading dose of dexmedetomidine at a rate of 1μg/kg over ten minutes were given IV. 15 mL of 0.25% bupivacaine was used for local infiltration by the surgeon. Next, a single 20 mg propofol bolus was given and a light level of sedation with a RASS score of -2 was obtained in order to help facilitate the insertion of the Mayfield skull-pins (Figure 2). The patient continued to maintain spontaneous breathing.
For the remainder of the procedure, a dexmedetomidine infusion was titrated between 0.4 - 0.8 μg/kg/hr to keep the patient comfortable, spontaneously breathing, and at a RASS of 0. The oxygen saturation (SpO2) remained 98% throughout the procedure, which ended uneventfully.
Discussion
Managing a difficult airway in the neurosurgical patient is a challenging endeavor with many complex obstacles that must be addressed by a mindful anesthetic plan. In our case, we had a patient with a recent history of a difficult fiberoptic intubation in need of an OR placement that had to be done utilizing the StealthStation ™ for stereotaxic guidance. Given this history and these neurosurgical requirements, we chose not to employ the traditional route of intubating the patient, as we were concerned that attempting another fiberoptic intubation would place the patient at a substantial risk for a poor outcome secondary due to the friability of the tumor. We were therefore forced to contemplate other options. We thought about using a laryngeal mask airway (LMA)but decided against using any supraglottic airway devices, since we were not certain these devices would sit properly in the larynx given the presence of the oropharyngeal tumor. Furthermore, LMAs carry the risk of inducing unwanted coughing, vomiting, or movement, and these unwelcomed incidents can increase the risk for adverse events including cerebral trauma, swelling, bleeding, or air embolism [5]. The option of a surgical airway was also discussed with the patient prior to the procedure, and after a multi-disciplinary team meeting with our ENT colleagues, it was decided that this would have to be our only secondary option for airway access if the patient’s condition deteriorated while his head was fixed in the frame. Ultimately, our primary option was to use a MAC technique with a dexmedetomidine infusion and allow our patient to breath spontaneously throughout the procedure.
The goal for our case was to keep the patient spontaneously breathing and awake so that he would protect his own airway from potential obstruction that could be caused by the large friable tumor present in his oropharynx. We avoided medications that would potentially cause drastic changes in respiratory effort. We also attempted to evade the intraoperative complication of vomiting and aspiration, by pre-treating our patient with ondansetron and by avoiding the use of medications that cause significant respiratory depression. Additionally we were not concerned for seizures, since the patient had no previous history of seizures as well as the fact that the neurosurgeons also felt that the patient did not require any prophylactic treatment.
Dexmedetomidine has been safely and effectively used for conscious sedation in awake craniotomies (AC) due to its minimal interference with electrocorticography and allowance for neurobehavioral testing required for functional brain mapping [3, 5-9]. Dexmedetomidine’s effectiveness in routine ACs is quite validated [3, 7, 8]. However, very few studies, that focus solely on the anesthetic approach for high-risk patients with difficult airways undergoing neurosurgical procedures, currently exist.
Garavaglia et al., discusses a case series of ten high-risk patients undergoing AC procedures of which only two are known difficult airway cases [5]. Our anesthetic plan for this high-risk OR placement case happens to be very similar to the approach used by Garavaglia et al., for their high-risk AC cases. We both utilized local anesthetics and dexmedetomidine as the primary sedative agent. However, we had a few key differences. In their cases, midazolam was used to reduce the anxiety during pin placements, while we titrated a low dose of propofol in order to assist with the stressful moments of pin placements. Additionally, we avoided the use of opioids, while Garavaglia et al., titrated low doses of opioids in one of their two difficult airway cases [5]. Both techniques maintained a normal respiratory drive and spontaneous ventilation, without any anesthetic complications.
Although dexmedetomidine has many advantageous properties that make it suitable for both an OR and an AC procedure, it should be emphasized that its pharmacological properties are helpful when managing a patient with a difficult airway. Dexmedetomidine is a highly selective α2-adrenergic receptor agonist that decreases anxiety, produces a dose-titrated and unusually cooperative form of sedation, reduces pain, and does not induce ventilatory suppression [5-8]. Dexmedetomidine’s ability to preserve spontaneous ventilation is a vital characteristic needed in managing a patient with difficult airway. Additionally, dexmedetomidine has analgesic properties. Studies have shown that dexmedetomidine can reduce both perioperative and potentially postoperative opioid requirements in neurosurgical cases [9, 10]. Opioid use is associated with respiratory depression and excessive sedation. Opioid use can lead to the undesired events such as airway obstruction, hypoxia, and hypercarbia. Avoidance of respiratory depression and excessive sedation are critical elements of successful anesthesia in patient with a difficult airway. In our case, the technique of MAC with dexmedetomidine offered a clear and distinct advantage over other possible anesthetic techniques [5, 7-9]. We believe that this technique diminishes the complexity and the concerns of having to intubate/control a difficult airway by simply avoiding the need for any airway device altogether.
Conclusion
We demonstrated successful anesthetic management in a difficult airway patient in need of an OR placement. Our goal is to inspire others to explore our approach in order to form a more standardized anesthetic management for high-risk patients with difficult airways in need of neurosurgical procedures.
References
- Ommaya A. Subcutaneous reservoir and pump for sterile access to ventricular cerebrospinal fluid. Lancet. 1963 Nov 9;2(7315):983-4. PubMed PMID: 14059058.
- Pels H, Juergens A, Glasmacher A, Schulz H, Engert A, Linnebank M, et al. Early relapses in primary CNS lymphoma after response to polychemotherapy without intraventricular treatment: results of a phase II study. J Neurooncol. 2009 Feb;91(3):299-305. PubMed PMID: 18931887.
- Stevanovic A, Rossaint R, Veldeman M, Bilotta F, Coburn M. Anaesthesia management for awake craniotomy: systematic review and meta-analysis. PLoS One. 2016 May 26;11(5):e0156448. PubMed PMID: 27228013.
- Srejic U, DeMonte F. (2008) Chapter 3: Stereotactic Brain Biopsy, Ommaya Reservoir, Intracavitary Brain Catheters, Management of Cranial Pressure Monitors/Drains. InNeurecipes: The MD Anderson Cancer Center Guide to Anesthesia for Neurosurgical Cases. AuthorHouse, Bloomington, Indiana. pp.8-13.
- Garavaglia MM, Das S, Cusimano MD, Crescini C, Mazer CD, et al. Anesthetic approach to high-risk patients and prolonged awake craniotomy using dexmedetomidine and scalp block. J Neurosurg Anesthesiol. 2014 Jul;26(3):226-33. PubMed PMID: 24064713.
- Uyar AS, Yagmurdur H, Fidan Y, Topkaya C, Basar H. Dexmedetomidine attenuates the hemodynamic and neuroendocrinal responses to skull-pin head-holder application during craniotomy. J Neurosurg Anesthesiol. 2008 Jul;20(3):174-9. PubMed PMID: 18580347.
- Shen SL, Zheng JY, Zhang J, Wang WY, Jin T, Zhu J, et al. Comparison of dexmedetomidine and propofol for conscious sedation in awake craniotomy: a prospective, double-blind, randomized, and controlled clinical trial. Ann Pharmacother. 2013 Nov;47(11):1391-9. PubMed PMID: 24259599.
- Haroun L, Amin M, Eloy JD, Bekker A. Anesthetic Considerations for awake Craniotomy in Epilepsy Surgery.
- Ard JL, Bekker AY, Doyle WK. Dexmedetomidine in awake craniotomy: a technical note. Surg Neurol. 2005 Feb;63(2):114-6; discussion 116-7. Pub- Med PMID: 15680647.
- Liu Y, Liang F, Liu X, Shao X, Jiang N, Gan X. Dexmedetomidine reduces perioperative opioid consumption and postoperative pain intensity in neurosurgery: a meta-analysis. J Neurosurg Anesthesiol. 2018 Apr;30(2):146-155. PubMed PMID: 28079737.