Postsurgical Chronic Pain: Incidence and Associated Factors in a Latin American Population
Quintero O1, Moyano J2*, Romero D1
1 Departamento de Anestesia, Fundacion Santafe de Bogota, Colombia.
2 Jefe Servicio Clinica de Dolor y Cuidado Paliativo, Deparmento de Anestesia, Hospital Universitario Fundación Santafe de Bogotá, Bogotá, Colombia.
*Corresponding Author
Jairo Moyano, MD, PhD,
Deparmento de Anestesia, Servicio Clinica de Dolory Cuidado Paliativo,
Hospital Universitario Fundación Santafe de Bogotá, Carrera 7 No. 117-15, Bogotá, Colombia.
Tel: 57 1 6199375/57-3123507164
Fax: 57 1 6122362
E-mail: jmoyano@unbosque.edu.co
Received: August 01, 2017; Accepted: September 23, 2017; Published: September 26, 2017
Citation: Quintero O, Moyano J, Romero D. Postsurgical Chronic Pain: Incidence and Associated Factors in a Latin American Population. Int J Anesth Res. 2017;5(8):479-484. doi: dx.doi.org/10.19070/2332-2780-1700097
Copyright: Moyano J© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: It is important to know the incidence of Chronic Post-Surgical Pain (CPSP), to describe the distribution of risk and protective factors associated with its presentation and to measure its impact on the quality of life. Due to the diversity of factors that have been implicated as potentially associated with chronic post-surgical pain, it is important to look for differential characteristics including emotional features to establish whether there are differences in the incidence of this type of pain.
Methods: A prospective analytical observational study was conducted in surgical patients at a University hospital from January 1 2014. Patients were asked to score their pain in the preoperative and immediate postoperative setting, and 3 months after surgery; preoperative, intraoperative, and postoperative risk factors were assessed, and quality of life was assessed in the preoperative setting and 3 months after surgery.
Results: We included 108 patients for a preliminary analysis, the study continued until the target sample size had been reached. The global incidence of CPSP was 16.67% (95%CI 9.63-23.69). Risk factors were the presence of pain prior to surgery and the duration of the surgical procedure. The presence of pain prior to surgery is a risk factor for the transition to CPSP.
2.Introduction
3.Materials and Methods
4.Results
4.1 Comprehensive Assessment
5.Discussion
6.Acknowledgments
7.References
Keywords
Chronic Pain; Quality of Life; Pain; Postoperative; Risk Factor.
Introduction
Chronic post-surgical pain (CPSP) is an adverse outcome in a concerning number of surgical patients [1-5]. Considering that the quantity of surgeries increases steadily, it is expected that the number of people suffering from this type of chronic pain (CP) will increase significantly. CPSP has been defined in different ways but the key elements included in most definitions are persistent pain (continuous or intermittent) for more than 2 or 3 months after surgery when all other causes have been excluded. CPSP predictive or risk factors may be associated with patient characteristics (age, gender, depression, anxiety, lifestyle), specific conditions during the surgical procedure (nerve damage, surgical technique), as well as with treatments for comorbid conditions such as radiotherapy and chemotherapy [6, 7]. Several studies have been conducted to estimate the incidence of CPSP in different population groups and different types of surgeries [8, 9] on average 2-10% of patients undergoing surgical procedures report persistent pain 1 year after surgery [10]. Due to a greater acquaintance of its existence, and the need to control the negative impact on the well-being of the patient, a growing request for health services is expected to treat this modality of CP; however, because of its partially unknown nature, it is possible that the result of the treatments will not always be satisfactory. It is now documented that there is wide variation in the presentation of this type of pain, i.e. only some patients will develop it, while others with similar characteristics will not; therefore, a multifactorial etiology has been postulated. Nerve dysfunction has been reported to be involved in the genesis of chronic post-surgical pain. Some neuropathic features maybe be seen after surgical procedures (i.e. thoracotomy) and maybe related to nerve damage, paroxysmal or spontaneous pain, or autonomic signs, without evidence of ongoing tissue damage [11]. It is estimated that 1-3% of patients undergoing surgical procedures develop acute neuropathic pain and up to 56% of this group show progression from acute to CP at the 1-year follow-up [7, 12, 13].
Among the psychological aspects, the acceptance of pain has emerged as an influential construct in the understanding of its management. Acceptance of CP refers to the ability of the individual to learn how to live a fulfilling life despite CP, which has been measured by the Chronic Pain Acceptance Questionnaire (CPAQ)[14, 15]. On the other hand, pain catastrophizing, which is an emotional and cognitive exaggerated negative trend toward the potential or actual pain, has been recognized as an important factor associated with CP [16]. Some consequences of pain catastrophizing are the increased consumption of analgesics, interference with the activities of everyday life, and a worse prognosis of the painful pathology [18, 19].
While some aspects related to the development of CP are not yet known, including genetic make-up, the surgical procedure allows us to determine the starting point of nociception in advance. It also enables us to identify possible risk and protective factors of the postoperative course of pain [20]. The first step to design interventions that improve the outcome of patients undergoing surgery is to understand the behavior of CPSP and related factors (risk or protective). Currently, there is limited information regarding the epidemiology, clinical course, and impact on the quality of life of CPSP in Latin America. Hence, it is important to know its incidence, describe the distribution of risk and potential protective factors associated with it and measure the potential impact on the quality of life that this disease has on patients undergoing surgery in the Latin American population [21]. The purpose of this study is to find the incidence of chronic post-surgical pain and associated factors in a population of Latin American patients.
Materials and Methods
This prospective analytical observational study was conducted at a 200 bed University Hospital which offers care to most medical and surgical specialties. The Institutional Review Board approved the study protocol. Patients aged 18 years or older scheduled for one of the following procedures were included in the study: hip arthroplasty, knee arthroplasty, shoulder arthroplasty, thoracotomy, mastectomy, sternotomy, limb amputation, cesarean section, laparoscopic hernia repair, laparoscopic cholecystectomy, and craniotomy. Those with mental conditions (psychiatric or neurologic) that prevented them from answering the questionnaire properly and those with communication barriers were excluded.
Patients who fulfilled the admission criteria were invited to participate in the study, and, if they accepted, written informed consent was obtained. Before the surgical procedure, a standard preoperative assessment as well as an evaluation focus on pain were performed; patients were asked to fill out questionnaires evaluating pain at the initial assessment and at 3 months’ post-surgery. The questionnaires were tested for clarity during a pilot phase of the studied. The following information was obtained:
1. General medical history, during first consultation.
2. McGill pain questionnaire: during first consultation, and at 3 months postoperatively.v
3. Assessment of pain intensity through a verbal analogous scale (or numerical rating scale) from 0-10 (0=no pain, 10= worst imaginable pain) preoperatively, immediate postoperativepain in post-anesthetic care unit (PACU), and 3 months postoperatively.
4. SF-36 Quality of Life Questionnaire, registered before surgery and at 3 months postoperatively.
5. Pain Catastrophizing Scale (PCS): Catastrophizing is considered an important prognostic factor in chronic pain (score varies from 0 to 52, being 0 no catastrophizing); registered during the first consultation.
6. Chronic Pain Acceptance Questionnaire (CPAQ) is a 20-item instrument used to measure the acceptance of pain in people in CP, to be completed during the first consultation.
Three months after the surgical procedure, patients were contacted by telephone and asked for the presence of persistent postsurgical pain and its characteristics; the McGill questionnaire and SF-36 Quality of Life were completed. SPSS version 19.0 was used for statistical analysis. A template of the questionnaire was created in Excel. Multivariate model, Nagelkerke R2 and Hosmer- Lemeshow tests were used to evaluate the adjustment and power. A p value of < 0.05 was considered statistically significant, a sample size of 219 patients was calculated using Epi info v3.5.3 Statistical tool, assuming a CPSP prevalence of 15% with a 95% confidence interval and adjusting for 10% of possible losses. This preliminary analysis included 108 patients.
Results
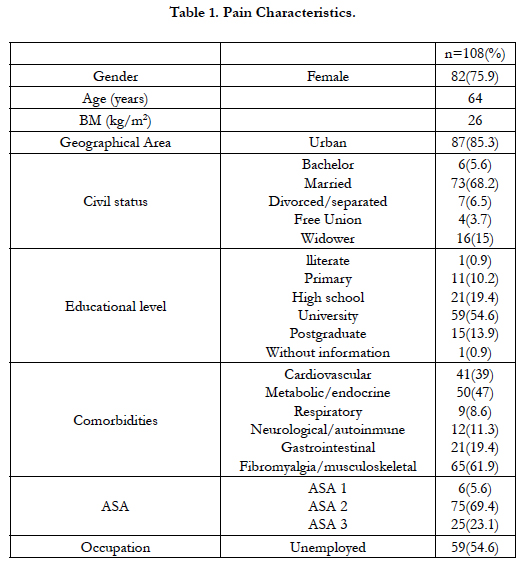
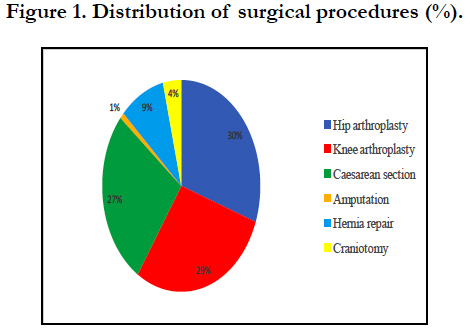
One hundred and eight consecutive patients scheduled for hip arthroplasty, knee arthroplasty, shoulder arthroplasty, thoracotomy, mastectomy, sternotomy, limb amputation, cesarean section, herniorrhaphy and craniotomy were enrolled between January and July 2014. One was excluded from analysis since the patient asked not to participate in the study. One hundred and eight patients (82 women) were included in the analysis. The demographic characteristics are shown in Table 1 and the distribution of surgeries is shown in Figure 1. Most patients underwent orthopedic procedures (60%), followed by caesarean section (28.7%). General anesthesia was used in 52.7% (n=57) of patients, regional anesthesia in 27.7% (n=30), total intravenous anesthesia was used in 11.1% (n=12) and local anesthesia in 8.3% (n=9). The median duration of surgery was 107 minutes. For hip arthroplasty, the median duration was 110 minutes, for knee arthroplasty the median was 139 minutes, for caesarean section it was 45 minutes, for hernia repair it was 91 minutes, and for craniotomy it was 285 minutes.
Pain Catastrophizing Scale median score was 4 (Min: 0, Max: 49, interquartile amplitude was 15). The chronic pain acceptance CPAQ mean overall score was 57.5 (SD 10.2). The components of the questionnaire were distributed as follows: mean CP disposition score was 33.75 (SD 10.8) and the mean acceptance of CP score was 23.7 (SD 7.8).
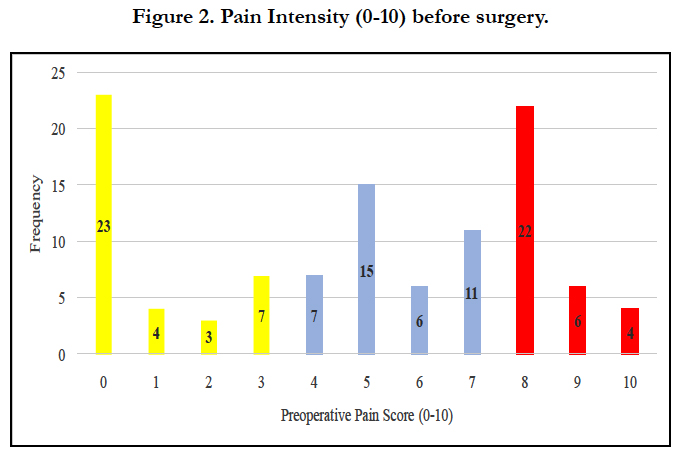
The distribution of pain prior to surgery shows that 79.6% (86 out of 108 patients) had pain related to the cause of surgery. Of those patients in pain before surgery, 39.8% had a pain intensity greater than 7/10 (Figure 2). It was found that the median time from the onset of pain was 715 days. Of those patients in pain at the initial assessment, 58.1% used analgesics.The mean time of usewas 110 days, with a median of 110 days (minimum 8, maximum 5475 days, interquartile range 406).
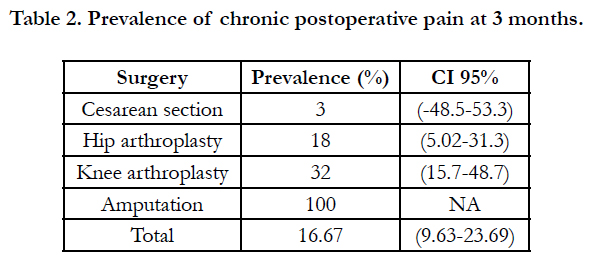
The prevalence of CPSP was evaluated at 3 months (Table 2), being the overall prevalence of 16.67%.
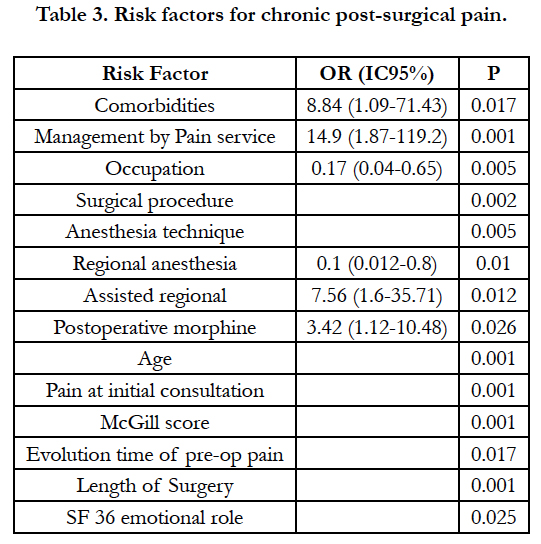
Orthopedic surgery was most frequently related with CPSP. After bivariate analysis using the Chi square test, it was found that having comorbidities, being treated by the pain service in the postoperative period, and occupation were associated with the development of CPSP at 3 months. The Mann-Whitney test found a significant relationship between pain score in the initial consultation (VAS or McGill), duration of pain prior to surgery, and the incidence of CPSP at 3 months after surgery. Only one patient was subjected to amputation, and he developed chronic pain at 3 months.
There was no statistically significant relationship between the SF36 scores and the incidence of CPSP at 3 months, except for the emotional role (p = 0.025). Table 3 summarizes the risk factors for chronic post-surgical pain at 3 months.
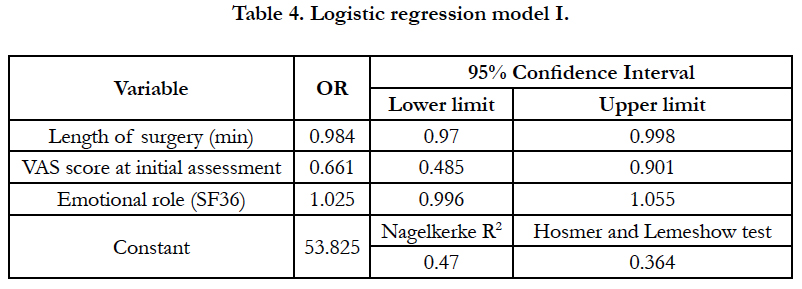
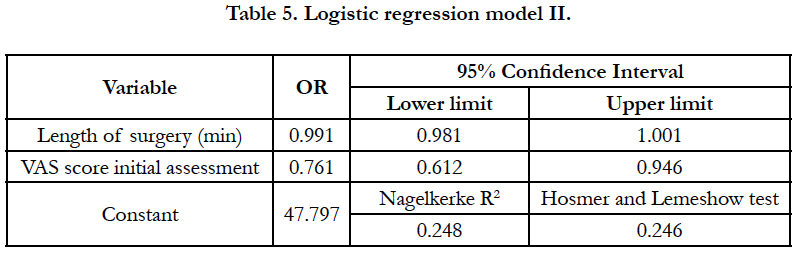
After multivariate analysis using multiple logistic regression, twomodels were proposed. Of those risk factors that reached statistical significance in bivariate analysis, it was found that duration of procedure and pain intensity at the initial assessment had a directly proportional relationship with the incidence of CPSP at 3 months (OR 0.984 and 0.661, respectively) (Table 4). The emotional role item of the SF36 questionnaire did not reach statistical significance in the multivariate model; therefore, a new multivariate analysis was performed without this variable (Table 5).
In the second model, the duration of surgery did not reach statistical significance. However, VAS maintained its statistical significance as a risk factor with an inversely proportional relationship between pain at the initial assessment and the incidence of chronic postoperative pain (OR 0.76; p = 0.014).
Discussion
This research shows that the high prevalence of CPSP remains a challenging condition through different surgical procedures, being more frequent in “high risk surgeries” such as knee and hip joint replacementas previously found [8, 22]. In this research, an identified risk factor to develop CPSP at follow-up was the presence severe acute postoperative pain which indicates the need to develop an efficient control of postoperative pain [23]. Indeed, several researchers have identified the relationship between acute pain intensity and CPSP. Given the huge variety of surgical procedures, and the wide range incidence of CPSP in each procedure, the need to develop specific analgesic treatments by surgical procedure is apparent. In some instances, these treatments could include anti-neuropathic medicines from the preoperative period, such as NMDA channel blockers during the intraoperative period and continued in the postoperative period. Calcium channel blockers have been used when neuropathic pain has been involved [2, 22].
In this research, 16.7% of patients included in the analysis developed CPSP 3 months after the procedure. This prevalence is likethat reported by previous studies [3, 20, 24, 25]. In this research, two variables showed statistical significance as risk factors for CPSP in logistic regression analysis (pain prior to surgery, p = 0.009 and duration of surgery, p = 0.025), these findings were consistent with the previously published data [10]. The first research that identified surgery as a significant risk factor for the development of CP was published in 1998 by Crombie et al. In that study the authors reported that approximately 40% of the 5130 patients with CP at 10 pain clinics from the United Kingdom developed CP after surgery or trauma. A survey carried out in 10 pain clinics in Scotland and North of England found that surgery contributed to approximately 25% of the total number of referrals, positioning itself as the second leading cause of CP.
Our population had low to moderate scores in the CPAQ, and a predominantly low score on the PCS [14, 26], both of which are psychological scores associated with the incidence of CPSP. However, these scores did not show a statistically significant association with the incidence of CPSP, which is consistent with the results described earlier [3]. This lack of significance could be related to the limited sample size used for these partial results.
The SF36 questionnaire measures components of the quality of life, and was used as a tool to determine the impact of CPSP on the quality of life of patients. We explored the relationship between this score and the incidence of CPSP, and found that the emotional role has a statistically significant relationship with CPSP. It is important to emphasize that the average score of the mental and physical component summary (PCS and MCS respectively) for this population were lower than the media of the U.S. population for each of these components.
Both the duration of surgery and the presence of pain in the preoperative period are important risk factors for the incidence of CPSP (Table 4). When a shorter duration of surgery and lower levels of pain intensity were found, there was a lower risk of CPSP (OR 0.98 and 0.66, respectively). It can be inferred that there must be other risk factors that explain the incidence of CPSP, corroborating the multifactorial etiology of this condition.
A higher incidence of CPSP was found in orthopedic procedures. Orthopedic surgeries are frequently associated with the presence of pre-operative CP, so these patients may have active central and/or peripheral sensitization mechanisms that facilitate the persistence of pain after surgery. Neither age nor gender were factors of risk or protection in this sample, which correlates with previous inconsistent findings on these variables. The use of analgesics prior to surgery was not a statistically significant relationship with the occurrence of CPSP, which could explain why the analgesic use was inconsistent and rarely achieved proper pain control given the high prevalence of pre-surgical pain associated with a low rate of analgesic use (58% of all patients who reported pain in the initial consultation). It has been found that effective analgesic control is more important in preventing the incidence of CPSP than the use of analgesics. In contrast to earlier reports, the presence of acute postoperative pain in this research did not show a statistically significant relationship with the occurrence of CPSP (p=0.96). Likewise [3], it has been postulated that the changes in neuroplasticity related to the development of CPSP are more extensive and severe with preoperative CP than those which could be produced for a brief time of acute pain in the postoperative period.
Per institutional policies more than half of the patients received treatment by the pain service (62.4%); however, being treated by a specialized pain service in the postoperative period was not a protective factor for CPSP. This can be explained by the possible presence of the patient's own genetic, biological, social, and environmental factors, some of them cannot be modified or intervened in, even with optimal analgesic treatment in the postoperative period. It has been mentioned that the mechanisms of CP and the central/peripheral sensitization seem to be influenced more by a persistent painful stimulus and established in the longterm rather than due to acute painful stimuli. These results highlight the importance of efficient postoperative pain treatment and the duration of surgery as possible factors that are likely to alter the incidence of CPSP. The strength of this study lies in its prospective character and the inclusion of multiple procedures which allows the analysis of results per the type of surgery performed. Likewise, it allows the influence of anesthetic technique on the development of CPSP to be explored. However, it has certain limitations. First, it is difficult to determine whether CPSP is a new entity or an extension of CP. While the CPSP definition requires that it excludes chronic pain, in practice this task it is not as easybecause of the subjective nature of pain. Another limitation of the study is that it included patients from a single university hospital with a leading pain service, which could modify the incidence of CPSP compared with other centers.
This study shows that the overall incidence found is located towards the lower limit of the range reported in the literature (16.7%). When the analysis is by type of surgical procedure, the incidence of CPSP is lower than that reported by others for the respective procedure, especially in the case of joints replacement. This could relate to the fact that the hospital where the study was conducted developed an institutional pain policy for pain screening and treatment and a specialized acute pain service.
We find that the presence of pain prior to surgery is one major risk factor reported in the literature to date [27]. This finding opens the door to an important point of therapeutic action for the prevention of CPSP and designates an indicator of those patients with a high probability of evolution into a CP entity in the postoperative period. It is important to continue research efforts into the pathophysiology and development of CPSP, as its incidence indicates that a significant proportion of patients will suffer from it.
In general, the findings of this research agree with findings from previous studies. One distinctive feature is that the sample came from a Latin American population, which means that genetic factors may be different although those factors apparently did not influence our results.
Possible improvement measures include an institutional diffusion of the use of anti-neuropathic drugs in patients stratified as highrisk.
Acknowledgments
The editorial assistance of Paola Lecompte MD is gratefully acknowledgemend.
References
- Searle R, Simpson K. Chronic post-surgical pain. Contin Educ Anaesthesia, Crit Care Pain. 2010;10(1):12-4.
- Ravindran D. Chronic Postsurgical Pain: Prevention and Management. J Pain Palliat Care Pharmacother. 28(1):51-3. PubMed PMID: 24552601.
- Hoofwijk DM, Fiddelers AA, Peters ML, Stessel B, Kessels AGH, Joosten EA, et al. Prevalence and Predictive Factors of Chronic Postsurgical Pain and Poor Global Recovery 1 Year after Outpatient Surgery. Clin J Pain. 2015;31(12):1017–25. PubMed PMID: 25565589.
- Bruce J, Quinlan J. Chronic Post Surgical Pain. Rev pain. 2011;5(3):23–9. PubMed Central PMCID: PMC4590073.
- MU Werner, JM Bischoff. Persistent postsurgical pain: Evidence from breast cancer surgery, groin hernia repair, and lung cancer surgery. Curr Top Behav Neurosci. 2014;20:3–29. PubMed PMID: 24523139.
- Buvanendran A. Chronic postsurgical pain: Are we closer to understanding the puzzle? Anesth Analg. 2012 Aug;115(2):231–2. PubMed PMID: 22826522
- Jin J, Peng L, Chen Q, Zhang D, Ren L, Qin P, et al. Prevalence and risk factors for chronic pain following cesarean section: a prospective study. BMC Anesthesiol. 2016 Oct 18;16(1):99. PubMed PMID: 27756207.
- Huang A, Azam A, Segal S, Pivovarov K, Katznelson G, Ladak SS, et al. Chronic postsurgical pain and persistent opioid use following surgery: the need for a transitional pain service. Pain Manag. 2016 Oct;6(5):435–43. PubMed ID: 27381204.
- Gupta A, Gandhi K, Viscusi ER. Persistent postsurgical pain after abdominal surgery. Tech Reg Anesth Pain Manag. 2011 Jul;15(3):140–6.
- Reddi D, Curran N. Chronic pain after surgery: pathophysiology, risk factors and prevention. Postgrad Med J. 2014 Apr;90(1062):222–7. PubMed PMID: 24572639.
- Theunissen M, Peters ML, Schepers J, Maas JWM, Tournois F, van Suijlekom HA, et al. Recovery 3 and 12 months after hysterectomy. Medicine (Baltimore). 2016 Jun;95(26):e3980. PubMed Central PMCID: PMC4937912.
- Gerbershagen HJ, Pogatzki-Zahn E, Aduckathil S, Peelen LM, Kappen TH, van Wijck AJM, et al. Procedure-specific Risk Factor Analysis for the Development of Severe Postoperative Pain. Anesthesiology. 2014 May;120(5):1237–45. PubMed PMID: 24356102.
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 Aug;386(9995):743–800. PubMed PMID: 26063472.
- Rodero B, García-Campayo J, Casanueva B, del Hoyo YL, Serrano-Blanco A, Luciano J V. Validation of the Spanish version of the Chronic Pain Acceptance Questionnaire (CPAQ) for the assessment of acceptance in fibromyalgia. Health Qual Life Outcomes. 2010 Apr 12;8:37. PubMed PMID: 20385016.
- Hinrichs-Rocker A, Schulz K, Järvinen I, Lefering R, Simanski C, Neugebauer EAM. Psychosocial predictors and correlates for chronic post-surgical pain (CPSP) - A systematic review. Eur J Pain. 2009 Aug;13(7):719–30. PubMed PMID: 18952472.
- Greenbaum S, Wasan AD, Sc M, Borsook D, Ph D, Jamison RN, et al. Distraction analgesia in chronic pain patients: the Impact of Catastrophizing. Anesthesiology. 2014 Dec;121(6):1292–301. PubMed PMID: 25264596.
- Saxena AK, Chilkoti GT, Chopra AK, Banerjee BD, Sharma T. Chronic persistent post-surgical pain following staging laparotomy for carcinoma of ovary and its relationship to signal transduction genes. Korean J Pain. 2016 Oct;29(4):239–48. PubMed Central PMCID: PMC5061640.
- Papaioannou M, Skapinakis P, Damigos D, Mavreas V, Broumas G, Palgimesi A. The role of catastrophizing in the prediction of postoperative pain. Pain Med. 2009Nov;10(8):1452–9. PubMed PMID: 19863742.
- Valdes AM, Warner SC, Harvey HL, Fernandes GS, Doherty S, Jenkins W, et al. Use of prescription analgesic medication and pain catastrophizing after total joint replacement surgery. Semin Arthritis Rheum. 2015 Oct;45(2):150–5. PubMed PMID: 26092331.
- Meissner W, Coluzzi F, Fletcher D, Huygen F, Morlion B, Neugebauer E, et al. Improving the management of post-operative acute pain: priorities for change. Curr Med Res Opin. 2015 Nov;31(11):2131–43. PubMed PMID: 26359332.
- Guimaraes-Pereira L, Valdoleiros I, Reis P, Abelha F. Evaluating persistent postoperative pain in one tertiary hospital: Incidence, quality of life, associated factors, and treatment. Anesthesiol Pain Med. 2016Apr;6(2):e36461. PubMed Central PMCID: PMC4886451.
- Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: A combined systematic review and meta-analysis. Anesth Analg. 2012 Aug;115(2):428-42. PubMed PMID: 22415535.
- Nunes BC, Garcia JB, Sakata RK. Morphine as first medication for treatment of cancer pain. Braz J Anesthesiol. 2014 Aug;64(4):236–40. PubMed PMID: 24998106.
- Fletcher D, Stamer UM, Pogatzki-Zahn E, Zaslansky R, Tanase NV, Perruchoud C, et al. Chronic postsurgical pain in Europe: An observational study. Eur J Anaesthesiol. 2015 Oct;32(10):725-34. PubMed PMID: 26241763.
- Martínez-Nicolás I, Ángel-García D, Saturno PJ, López-Soriano F. Cancer pain management: systematic review and critical appraisal of clinical practice guidelines. Rev Calidad Asistencial. 2016 Feb;31(1):55-63.
- García J, Rodero B, Alda M, Sobradiel N. Validation of the Spanish version of the pain catastrophizing scale in fibromyalgia. Med Clin. 2008 Oct;131(13):487–92. http://dx.doi.org/10.1157/13127277
- Laufenberg-Feldmann R, Kappis B, Mauff S, Schmidtmann I, Ferner M. Prevalence of pain 6 months after surgery: a prospective observational study. BMC Anesthesiol. 2016 Oct 10;16(1):91.