Percutaneous Dilatational Tracheostomy: ULTRAperc® Single Stage Dilator Technique Versus Ciaglia Blue Dolphin® Balloon Dilatation Technique for Intubated Unweanable ICU Patients
Abbas MS*, Maher H
Department of Anesthesia, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
*Corresponding Author
Mohamed Sayed Abbas,
Anesthesia Department,
Al Mouwasat Hospital, Dammam, KSA.
Tel: 00966507275885
GSM: 00966138203436
E-mail: mohamed_abasy@hotmail.com
Received: February 02, 2017; Accepted: March 23, 2017; Published: March 28, 2017
Citation: Abbas MS, Maher H (2017) Percutaneous Dilatational Tracheostomy: ULTRAperc® Single Stage Dilator Technique Versus Ciaglia Blue Dolphin® Balloon Dilatation Technique for Intubated Unweanable ICU Patients. Int J Anesth Res. 5(3), 417-421. doi: http://dx.doi.org/10.19070/2332-2780-1700086
Copyright: Abbas MS© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Percutaneous tracheostomy is currently one of the most common procedures performed in ICU. It has demonestrated provide numerous advantages over the classical surgical tracheostomy. The aim of this study is to compare ULTRAperc single stage dilator technique with Ciaglia Blue Dolphin ballon dilatation technique for intubated unweanable ICU patients with respect to procedure difficulties and complications.
Methods: A prospective randomized trial was used to compare two different techniques of percutaneous dilatational tracheostomy performed by ICU physicians in intubated unweanable ICU patients. The study included 60 intubated ICU patients with failure of liberation from mechanical ventilation, underwent bedside dilatational tracheostomy using ULTRAperc tracheostomy set (30 patients) and Ciaglia Blue Dolphin balloonset (30 patients). Both groups were compared as regards procedure technical difficulties such as difficult dilatation and difficult tube insertion and complications such as pneumothorax and subcutaneous emphysema.
Results: Six patients in the Ciaglia Blue Dolphin group were difficult in dilatation and tube insertion and there was over dilatation of the tracheal stoma Compared to zero recorded cases in the ULTRAperc group (P-value = 0.024). Failed tube insertion and false passage was recorded in two cases in the Ciaglia Blue Dolphin group compared with zero recorded cases in the ULTRAperc group (P-value = 0.492). There were zero recorded cases of cardiac arrest or lung atelectasis in either groups. No significant statistical difference was found between groups as regards pneumothorax, pneumomediastinum and subcutaneous emphysema. Seven patients in the Ciaglia Blue Dolphin group experienced minor bleeding from the tracheostomy site compared with zero recorded bleeding complications in the ULTRAperc group (P-value = 0.011).
Conclusions: Percutaneous dilatational tracheostomy for intubated unweanable ICU patients using ULTRAperc single stage dilator technique is easier and associated with fewer complications as compared with Ciaglia Blue Dolphin ballon dilatation technique.
2.Abbreviations
3.Background
4.Methods
5.Statistical Analysis
6.Results
7.Discussion
8.Ethics and Consent
9.Authors’ contributions
10.Conclusions
11.References
Keywords
Percutaneous Tracheostomy; ULTRAperc; Ciaglia Blue Dolphin.
Abbreviations
APACHE: Acute Physiology and Chronic Health Evaluation; ARDS: Adult Respiratory Distress Syndrome; CBD: Ciaglia Blue Dolphin; FiO2: Fraction of Inspired Oxygen; ICU: Intensive Care Unit; PDT: Percutaneous Dilatational Tracheostomy; PEEP: Positive End Expiratory Pressure; SD: Standard Deviation; UP: Ultra-perc; ST: Surgical Tracheostomy
Background
Intubated ICU patients with failure of weaning from mechanical ventilation usually needs replacement of the endotracheal tube with tracheostomy tube for fear of complications associated with prolonged intubation. Once the decision was taken to perform tracheostomy, the next question is which technique to choose percutaneous or surgical.
Surgical tracheostomy (ST) is considered one of the oldest surgical procedures, first described by Chevalier Jackson in 1909. For more than six decades, It was usually done by the surgical team in the operating room requiring the transfer of critically ill patients to be performed (from the intensive care unit (ICU) to the operating room (OR)). The technique of surgical tracheostomy involves dissecting pretracheal tissues and inserting the tracheostomy tube into the trachea under direct vision [1].
Percutaneous dilatational tracheostomy (PDT) was first describedin 1957 [2]. In 1985, Ciaglia et al., [3] described a technique of PDT using a needle guide wire technique and multiple serial dilators to dilate the tracheostomy stoma to fit the tracheostomy tube. In 1989, Schachner et al., [4] developed a single dilation tracheostomy using a flexible metal guide wire, needle and a specially designed tool that slides over the guidewire into the trachea and is used to dilate the tracheal stoma by squeezing its handles facilitating the insertion of a cuffed tracheostomy tube. In 1990, Griggs et al., [5] developed a single stage dilation technique using a specially designed modified forceps named Howard-Kelly forceps as a tracheal dilator by sliding over the guidewire into the airway. In 1998, The Ciaglia Blue Rhino Single stage dilator technique was introduced as a modification of the multiple dilator technique described in 1985. The PortexUltraperc (Smith Medical, Hythe, Kent, UK) offers a similar set to the Ciaglia Blue Rhino PDT with a single-step curved hydrophilic white dilator kit and in addition provides a tapered introducer for the tracheostomy tube. The Ciaglia Blue Dolphin has been introduced as a modification of the Ciaglia Blue Rhino using a balloon-tipped catheter loading dilator assembly system as a tracheal dilator [6].
The aim of this study is to compare ULTRAperc single stage dilator technique with Ciaglia Blue Dolphin ballon dilatation technique for intubated unweanable ICU patients with respect to procedure difficulties and complications.
Methods
The study was registered on www.clinicaltrials.gov, Registration ID: NCT02754921, principal investigator’s name: Mohamed Sayed Mohamed Abbas, Registered 27 April 2016.
We conducted a prospective randomized trial to compare ULTRAperc single stage dilator technique (UP) and Ciaglia Blue Dolphin balloon dilatation technique (CBD) From January 2013 to December 2015. It included sixty critically ill patients older than 20 years in ICU who required tracheostomy as a result of failed weaning from mechanical ventilation. Ethical Committee approval and written informed consent from all the patients or their legal representatives was obtained prior to enrollment.
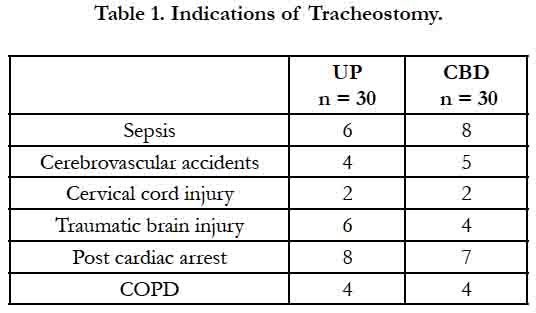
The indications for tracheostomy included sepsis, cerebrovascular accidents, cervical cord injury, traumatic brain injury, post arrest and COPD (Table 1).
Exclusion criteria consisted of patient or family refusal, emergency tracheostomy, distorted abnormal anatomy, bleeding diathesis, morbid obesity, previous tracheostomy, infected surgical site and ARDS patients requiring high PEEP and high FiO2.
These 60 ICU patients were divided into two groups, each one consisted of 30 patients. One group underwent percutaneous dilatational tracheostomy using the ULTRAperc technique and the other group underwent percutaneous dilatational tracheostomy using the Ciaglia Blue Dolphin technique. All patients were already intubated orotracheally and procedure was done under sedation in ICU using midazolam, fentanyl, and cis-atracurium. All patients were connected to mechanical ventilation with FiO2 of 100%. Arterial blood pressure, electrocardiography, pulse oximetry were continuously monitored. Patient is positioned with the neck hyperextended by placing a pillow under his shoulders to optimize the distance between the cricoid cartilage and the jugular notch. Then laryngoscopy was done and the endotracheal tube was withdrawn under direct vision until the cuff is located just under the vocal cords to minimize the risk of cuff puncture.
PDT was done by experienced ICU physicians using the widely accepted Seldinger guide wire technique. The skin and underlying tissues were anesthetized using lidocaine 2% as local anesthetic solution then a horizontal skin incision was madeat the level between the second and third tracheal rings, a curved forceps was used to spread the tissue in the midline, and the trachea is palpated through the wound. A 14 G cannula-over-needle connected to a saline-filled syringe was inserted into the trachea between the second and third tracheal rings with the needle bevel directed caudally. Tracheal entry of the needle was confirmed by aspiration of air into the saline-filled syringe. The needle is then removed leaving the cannula in place. A J-tip guidewire was then introduced through the cannula into the tracheal lumen followed by removal of the cannula leaving the guidewire in situ. A well-lubricated small pre-dilator was passed over the guide wire into the trachea to start the stoma formation and was later removed.
In Portex Ultraperc single stage dilator technique, a guiding catheter was introduced inside the single stage white Rhino (ULTRAperc) dilator until the tip of the dilator is at the safety stop of the guiding catheter then both are advanced over the guide wire until the tip of the guidewire comes out of the guiding catheter then both the guiding catheter and the single stage dilator are advanced together until a specific mark over the dilator has been reached. Next, the single stage dilator is removed leaving both the guidewire and the guiding catheter in place. The tracheostomy tube loaded over a well-lubricated tube introducer was then advanced over the guidewire and the guiding catheter into the tracheal stoma followed by removal of the introducer, guidewire and the guiding catheter leaving the tracheostomy tube in place.
In Ciaglia Blue Dolphin technique, the tracheostomy tube was loaded over a well lubricated balloon-tipped catheter assembly and then introduced over the guidewire remaining in situ. The deflated balloon catheter was advanced into the trachea until the balloon part of the catheter is traversing the skin aperture then the inflation pump was connected to the balloon port of the catheter and filled with saline solution to reach a pressure of 11 atm. The inflated balloon was kept in place for 10 seconds, and then completely deflated causing dilatation of the stoma allowing to advance the tracheostomy tube with the balloon–tipped catheter together as one unit into the trachea then both the balloon catheter and the guide wire were finally removed.
The tracheostomy tube balloon cuff was then inflated, and the ventilator was then connected to the tube and the orotracheal tube was removed. The correct placement of the tracheostomy tube was confirmed by capnography reading, chest auscultation and chest x-ray.
We compared the two groups as regards procedure difficulties including difficult dilatation defined as difficulty in dilating the tracheostomy stoma requiring multiple trials, difficult tube insertion defined as resistance to tracheostomy tube insertion, failed tube insertion, false passage and tracheal stoma over dilatation and Procedure complications including cardiac arrest, pneumothorax, pneumomediastinum, subcutaneous emphysema, minor bleeding defined as bleeding from tracheostomy stoma requiring less than two changes of trachestoma dressing within 4 hours after percutaneous tracheostomy procedure and lung atelectasis.
Statistical Analysis
Data were collected, tabulated, coded, and then analyzed using Minitab® 16.1.0 computer software. Numerical variables were presented as mean ± standard deviation or median (range), and compared using student’s t test or Mann-Whitney u test as appropriate, while categorical variables were presented as frequency and compared using Fisher’s exact test. Any difference with p-value <0.05 was considered statistically significant. Assuming the rate of difficult tube insertion is 28.6% [17], at least 30 patients are needed in each group to detect a reduction in this rate to be at most 5%, with a power of 0.8 and significance level of 0.05.
Results
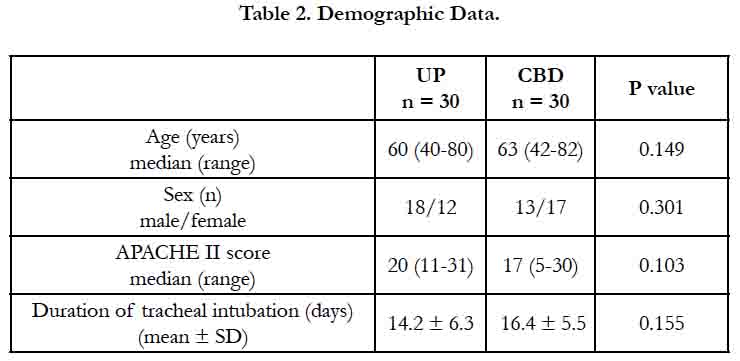
60 patients underwent percutaneous trachesotomy using the ULTRAperc technique and the Ciaglia Blue Dolphin technique divided into two groups 30 patients in each. The two groups were similar in terms of age, sex, APACHE II score and duration of tracheal intubation with no significant statistical difference (Table 2).
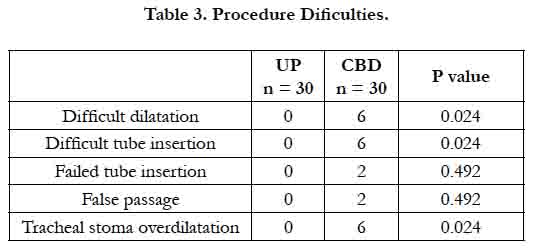
During the tracheostomy procedure, six patients in the Ciaglia Blue Dolphin group were difficult in dilatation and tube insertion and there was over dilatation of the tracheal stoma Compared to zero recorded cases in the ULTRAperc group. Failed tube insertion and false passage were recorded in two cases (out of the previously mentioned six difficult cases) in the Ciaglia Blue Dolphin group compared with zero recorded cases in the ULTRAperc group. There was significant statistical difference between the two groups as regards difficult dilatation, difficult tube insertion and tracheal stoma over dilatation (Table 3).
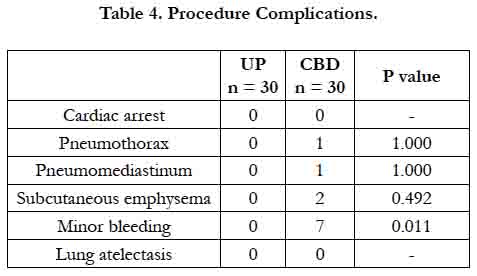
There were zero recorded cases of cardiac arrest or lung atelectasis in both groups. One patient developed pneumothorax and pneumomediastinum and two patients developed subcutaneous emphysema inthe Ciaglia Blue Dolphin group (the previously mentioned two cases with failed tube insertion and false passage) detected in chest X-ray done immediately post procedure with zero recorded such complications in the ULTRAperc group. Seven patients in the Ciaglia Blue Dolphin group experienced minor bleeding from tracheostomy site compared to zero recorded bleeding complications in the ULTRAperc group. Significant statistical difference between both groups was found only in the minor bleeding complication with no significant difference in others (Table 4).
Discussion
Performance of tracheostomy procedure in general offers many advantages when compared to conventional prolonged endotracheal intubation because tracheostomy tube is better tolerated by the patient with avoidance of laryngeal, cricoidal and hightracheal injury [7] decreasing the duration of sedation, allowing earlier weaning from mechanical ventilation and shorter overall length of stay in ICU [8-10]. That is why doing early tracheostomy will have positive impact on patient prognosis. The excellent results of percutaneous tracheostomy may influence the decision to perform a tracheostomy rather early. Additionally, percutaneous tracheostomy done at the bedside offers advantage of minimizing the duration of endotracheal intubation with all its risks and complications when compared with surgical tracheostomy performed in the OR which may be accounted to the ease of scheduling the percutaneous tracheostomy at the bedside, without the need for a surgical consultation or booking in the often busy ORs. Two studies [11, 12] have examined the time taken from the decision to perform a tracheostomy until the procedure has been performed. Both found that percutaneous tracheostomy was associated with a significantly shorter time as compared with surgical tracheostomy.
Unfortunately, there are some indications where percutaneous tracheostomy cannot be done such as emergency tracheostomy, difficult airway anatomy, prior airway problems, coagulopathies and previous tracheostomy. In such cases when it comes for decision to perform tracheostomy, It can be done only by surgical technique as percutaneous technique is contraindicated in such cases. Thus, despite the wide spread use of percutaneous tracheostomy, surgical tracheostomy may still be indicated for selected patients [13].
In 1992, it was recommended that percutaneous tracheostomy be done only by doctors in the surgical field [14], but one of the major advantages of this technique is that nonsurgically trained members of the health care team may perform the tracheotomy using a Seldinger technique, and this physican may be more familiar with the percutaneous technique than the respective surgeon such as intensive care and anesthesia doctors. In our study, all percutaneous tracheostomies were performed by an intensivist trained in performing percutaneous tracheostomies and were carried out at bedside in the intensive care unit.
Two studies were conducted on percutaneous dilatational tracheostomy using the ULTRAperc technique:
The first one was done by Patel et al., [15] on porcine model and mannequins comparing the ULTRA perc technique with the Blue Rhino technique and concluded that the ULTRAperc set is more easier, quicker and causes less anterior–posterior tracheal compression during tracheostomy tube insertion compared to the Blue Rhino set in both mannequin and porcine airway models. This advantage may be attributed to the presence of tracheostomy tube introducer.
The second study was done by Kumar et al., [16] comparing the ULTRAperc technique versus the Griggs guidewire dilating forceps technique and found that both techniques were comparable and equally reliable in performing percutaneous tracheostomy at bedside in ICU.
Two studies compared percutaneous tracheosotomy using the Ciaglia Blue Dolphin technique with the Ciaglia Blue Rhino technique in ICU patients. One study was done in 2010 and concluded that Ciaglia Blue Rhino technique was associated with shorter procedure time, less bleeding complications and less resistance to tracheal tube passage as compared to the Ciaglia Blue Dolphin technique [17]. The other study was done in 2014 and concluded that both techniques were comparable in processing time and processing difficulties with no patients in the two groups developing any complications such as pneumothorax, subcutaneous emphysema or mortality [18].
In our present study, we compared the ULTRA perc technique with the Ciaglia Blue Dolphin technique for percutaneous dilatational tracheostomy performed in ICU patients and we found that six cases in the Ciaglia Blue Dolphin exhibited difficulty in dilatation and tube insertion with subsequent tracheal stoma overdilation and bleeding. Two cases out of these six were associated with failed tracheostomy tube insertion and subsequent reintubation. While in the ULTRAperc group, there were no recorded cases with associated technical difficulties or complications.
Ethics and Consent
The study protocol was approved by Al Mouwasat hospital review board, and all the patients, or their legal representatives, provided a written informed consent before enrollment. The trial was registered on Clinicaltrials.gov (NCT02754921).
Authors’ contributions
MA and HM contributed equally to the design of the study, data collection, interpretation and statistical analysis. The final manuscript was revised and approved by both authors.
Conclusions
Percutaneous dilatational tracheostomy for intubated unweanable ICU patients using the ULTRAperc single stage dilator technique is easier and associated with fewer complications as compared to the Ciaglia Blue Dolphin balloon dilatation technique.
References
- McWhorter AJ (2003) Tracheotomy: timing and techniques. Curr Opin Otolaryngol Head Neck Surg. 11(6): 473-479.
- Shelden C, Pudenz R (1957) Percutaneous tracheotomy. J Am Med Assoc. 165(16): 2068-2070.
- Ciaglia P, Firsching R, Syniec C (1985) Elective percutaneous dilatational tracheostomy. A new simple bedside procedure; preliminary report. Chest. 87(6): 715-719.
- Schachner A, Ovil Y, Sidi J, Rogev M, Heilbronn Y, et al., (1989) Percutaneous tracheostomy-A new method. Critical care medicine. 17(10): 1052-6.
- Griggs WM, Worthley LI, Gilligan JE, Thomas PD, Myburg JA (1990) A simple percutaneous tracheostomy technique. Surg gynecol obstet. 170(6): 543-5.
- Gromann TW, Birkelbach O, Hetzer R (2009) Balloon dilatational tracheostomy: initial experience with the Ciaglia Blue Dolphin method. AnesthAnalg. 108(6): 1862–6.
- Frova G (2002) Improvements in percutaneous tracheostomy: the singlestep rotational dilation. Anaesthesia, Pain, Intensive Care and Emergency Medicine-APICE. 305-313.
- Griffiths J, Barber VS, Morgan L, Young JD (2005) Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 330(7502): 1243.
- Arabi Y, Haddad S, Shirawi N, Al Shimemeri A (2004) Early tracheostomy in intensive care trauma patients improves resource utilization: a cohort study and literature review. Crit Care. 8(5): R347-352.
- Shirawi N, Arabi Y (2005) Bench-to-bedside review: Early tracheostomyin critically ill trauma patients. Crit Care. 10(1): 201.
- Friedman Y, Fildes J, Mizock B, Samuel J, Patel S, et al., (1996) Comparison of percutaneous and surgical tracheostomies. Chest. 110(2): 480-485.
- Silvester W, Goldsmith D, Uchino S, Bellomo R, Knight S, et al., (2006) Percutaneous versus surgical tracheostomy: A randomized controlled study with long-term follow-up*. Crit care med. 34(8): 2145-52.
- Ben Nun A, Altman E, Best LA (2005) Extended indications for percutaneous tracheostomy. Ann Thorac Surg. 80(4): 1276-1279.
- Leinhardt DJ, Mughal M, Bowles B, Glew R, Kishen R, et al., (1992) Appraisal of percutaneous tracheostomy. Br J Surg. 79(3): 255-8.
- Patel PB, Ferguson C, Patel A (2006) A comparison of two single dilator percutaneous tracheostomy sets: The Blue Rhino and the Ultraperc. Anaesthesia. 61(2): 182-6.
- Kumar M, Trikha A (2012) Percutaneous dilatational tracheostomy: Griggs guide wire dilating forceps technique versus ULTRA-perc single-stage dilator-A prospective randomized study. Indian J Crit Care Med. 16(2): 87-92.
- Cianchi G, Zagli G, Bonizzoli M, Batacchi S, Cammelli R, et al., (2010) Comparison between single-step and balloon dilatational tracheostomy in intensive care unit: a single-centre, randomized controlled study. Br j anaesth. 104(6): 728-32.
- Cinar D, Kahveci K, Ozcan U, Guler L, Kabalak AA, et al., (2014) A comparision between blue rhino and balloon-assisted tracheostomy in intensive care units. Acta medica mediterranea. 30(2): 371-4.