Comparative Study between Intrathecal Hyperbaric and Isobaric Ropivacaine in Geriatric Patients, Undergoing Lower Limb Plastic Surgical Procedures
Ahmad Langoo S1, Jan S2, Ahmad T3*
1 Senior Resident, Department of Anaesthesiology, Sher-I-Kashmir Institute of Medical Sciences, Srinagar, India.
2 Post Graduate, Department of Anaesthesiology, Sher-I-Kashmir Institute of Medical Sciences, Srinagar, India.
3 Post Doctorate, Department of Plastic surgery, Sher-I-Kashmir Institute of Medical Sciences, Srinagar, India.
*Corresponding Author
Tawheed Ahmad,
Post doctorate, Department of Plastic surgery,
Sher-I-Kashmir Institute of Medical Sciences,
Srinagar, 190012, India.
Tel: +918491865492
E-mail: drtawheedahmad@yahoo.com
Received: December 04, 2016; Accepted: January 16, 2017; Published: January 19, 2017
Citation: Ahmad Langoo S, Jan S, Ahmad T (2017) Comparative Study between Intrathecal Hyperbaric and Isobaric Ropivacaine in Geriatric Patients, Undergoing Lower Limb Plastic Surgical Procedures. Int J Anesth Res. 5(1), 393-396. doi: http://dx.doi.org/10.19070/2332-2780-1600081
Copyright: Ahmad T© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Ropivacaine is one of the commonest drugs used for spinal anaesthesia. We conducted a study comparing characteristics of spinal anesthesia using isobaric and hyperbaric ropivacaine (0.75%), in geriatric patients who underwent plastic surgical procedures in lower limbs.
Study Design: Randomised double blind study.
Methods: Sixty Geriatric patients were randomly assigned into two groups (I & H group). Group I patients were given spinal anaesthesia using 15mg of isobaric ropivacaine (0.75%), whereas group H patients were given hyperbaric ropivacaine (0.75%). The characteristics of intrathecal anesthesia, hemodynamic parameters, quality of anesthesia and muscle relaxation as well as duration of post-operative analgesia were compared.
Results: In group H there was early onset of sensory block at T6 (group H 4.5 ± 2.3 vs. group I 6.4 ± 3.5 minutes; p = 0.015) and also earlyonset of grade 3 motor blockade (group H 5.10 ± 2.5 vs. group I 7.2 ± 4.4 minutes; p = 0.026); in addition as compared to group I, group H had shorter total duration of motor blockade (group H 127.3 ± 29.5 vs. group I 164.3 ± 35.2min; p < 0.0001), sensory blockade (group H 171.5 ± 28.1 vs. group I 207 ± 27.30 min., p < 0.0001) and duration of post-operative analgesia. Median maximum extent levels achieved, muscle relaxation and Quality of anesthesia were comparable in both groups.
Conclusion: 15mg of (0.75%) hyperbaric ropivacaine provides similar, reliable and effective quality of spinal anesthesia with early onset and early recovery from sensory and motor blockade, when compared to 15mg of (0.75%) isobaric ropivacaine.
2.Introduction
3.Materials and Methods
4.Statistical Analysis [4-7]
5.Results
5.1 Motor and Sensory Block Characteristics
5.2 Hemodynamic Characteristics
5.3 Intra Operative Analgesia and Muscle Relaxation
5.4 Side Effects
6.Discussion
7.Conclusion
8.References
Keywords
Hyperbaric vs. Isobaric Ropivacaine Solution; Spinal Anaesthesia, Lower Limb Surgeries.
Introduction
Anesthesia in geriatric patients is always challenging for anaesthetists, because of diminished cardiac reserve in these patients may lead to exaggerated drop in blood pressure during induction of anesthesia, in addition many elderly patients may experience post operatively varying degrees of confusional state, delirium or cognitive dysfunction. Ease of administration, rapidity of onset and reliability makes spinal anaesthesia more popular as compared to epidural anaesthesia. Various anaesthetic drugs like bupivacaine, lignocaine, levobupivacaine and ropivacaine are used for spinal anesthesia. The preferred drug in spinal anaesthesia is one which provides longer duration of analgesia with minimal side effects and toxicity; ropivacaine seems to have this profile, and hence ropivacaine is gaining increasing popularity. With ropivacaine there is less risk of central nervous system and cardiac toxicity, patient can be ambulated early and in addition it provides good quality of post-operative analgesia.
Ropivacaine has been used for administering spinal anaesthesia in both obstetric and non-obstetric patients [1]. Changing baricity of ropivacaine using glucose, changes its clinical characteristics when used in subarachnoid block [2]. Fentanyl enhances analgesic effect of local anaesthetic drug without intensifying motor and sympathetic block in spinal anesthesia, thus leading to lower incidences of hypotension, early recovery and mobilization, with additional benefit of decreasing total dose of local anesthetic drug needed [3].
The present study was conducted to compare the efficacy intrathecal hyperbaric ropivacaine and isobaric ropivacaine in geriatric patients undergoingc lower limb plastic surgical procedures. The two groups were compared in onset and duration of sensory and motor blockade, hemodynamic effects, quality of anesthesia and muscle relaxation, duration of post-operative analgesia and for side-effects.
Materials and Methods
This was prospective randomized double blind study, conducted on 60 elderly patient of ASA class 1&2, between the age group of 60-75 years and having height between 150-175cms undergoing plastic surgical procedures in lower limbs. Double blinding was done by not revealing the assessing person the group to which patient belonged and drug was prepared by anaesthesiologist who was not involved in subsequent assessment. Written informed consent was taken from patients after explaining procedure to them and to their relatives. All Patients with contraindication to spinal anaesthesia were excluded from the study. All patients were pre-loaded with ringer lactate intra-venous solution (15mg/kg). Patients were randomly and equally divided into 2 groups using computer generated randomisation chart:
1) Group H (Hyperbaric ropivacaine): Ropivacaine (0.75%) 15 mg (2ml) + 25mcg fentanyl (0.5ml) + 5% (50mg/ml) of dextrose 0.5ml = 3ml (total volume).
2) Group I (isobaric ropivacaine): Ropivacaine (0.75%) 15 mg (2ml) + 25mcg fentanyl (0.5ml) + normal saline 0.5ml=3ml (total volume).
On operation table blood pressure, ECG monitor and pulse oximeter were applied to record baseline pulse rate, blood pressure (BP), Respiratory rate (RR) and SPO2. Under all aseptic precautions intrathecal anesthesia was given in L3-L4 space using 25 gauge spinal needle in sitting position. Immediately after giving spinal anesthesia patient was turned into supine position. The sensory blockade was assessed by pin prick and motor blockade by using modified Bromage Scale (0: No block, 1: Inability to raise the extended leg, 2: Inability to flex the knee, and 3: Inability to flex the ankle and foot), every 2 minutes till highest sensory and motor levels were achieved. Then at the interval of every five minutes, till patient completely recovered. The variables recorded were: Time taken to achieve sensory block at T6; Highest level of sensory block achieved; Time taken to achieve maximum level of block; Time taken for 2 segment regression of sensory block from maximum block; Time taken for complete sensory regression; Maximum motor block achieved and Time taken for the onset of maximum motor block. Duration of motor block was recorded from the time of highest scale of motor block till complete recovery; ECG and SPO2 were monitored continuously while BP and pulse rate was monitored at every 2 minutes interval for 1st 10 minutes, every 5 minutes in intra-operative period and then every 10 minutes interval for rest of study period. For judging the quality of anaesthesia, patients were assessed for feeling of sensation during the operation and graded as:
A. No sensation throughout the operation.
B. Mild pain during operation but no need of additional analgesia.
C. Pain & need of additional analgesia.
Grade A considered as excellent analgesia, Grade B as good analgesia and Grade C as poor analgesia. Grade C patients were given Inj. Ketamine 10mg i.v and repeated after 5min on request. If after giving two doses of ketamine, patient still complained of pain, general anesthesia (GA) was given and considered as a failed case. If in any patient sensory blockade of T6 was not achieved, that case was excluded from study. During recovery phase patients were monitored at the interval of 15 minutes, for regression of motor and sensory effects. Duration of analgesia was assessed from time of intrathecal injection till the first analgesic request. Side effect like Hypotension (systolic BP < 80 mmHg) was treated by giving IV ringer lactate (RL) with Inj. ephedrine 6mg IV. Bradycardia (pulse rate <50 / min) was managed with Inj. Atropine 0.5mg i.v, Nausea, vomiting, pruritus were treated symptomatically. Quality of muscle relaxation was assessed by surgeon and classified as Excellent, Satisfactory and Unsatisfactory. At the end of surgery, patients were asked for satisfaction level which was graded as Poor, Good and Excellent. On post-operative day 1 & 5 patients were followed for side effects like headache and Back pain.
Statistical Analysis [4-7]
The data was assessed by using statistical product and service solutions (SPSS) software version 22.0. For intergroup comparison unpaired t-test was used. Probability values (P-value) of <0.05 were considered significant. All data was presented as mean (SD) except highest sensory blockade level achieved, for which Chisquare test was used. For patients Satisfaction level and for quality of intra-operative muscle relaxation ‘Z’ test was applied.
Results
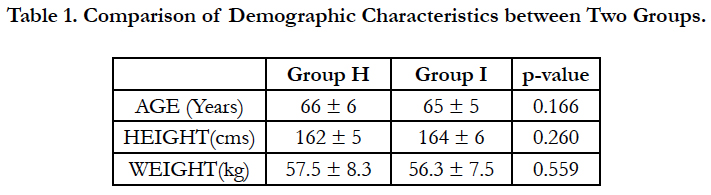
Both groups were comparable with respect to age, weight and height [Table 1].
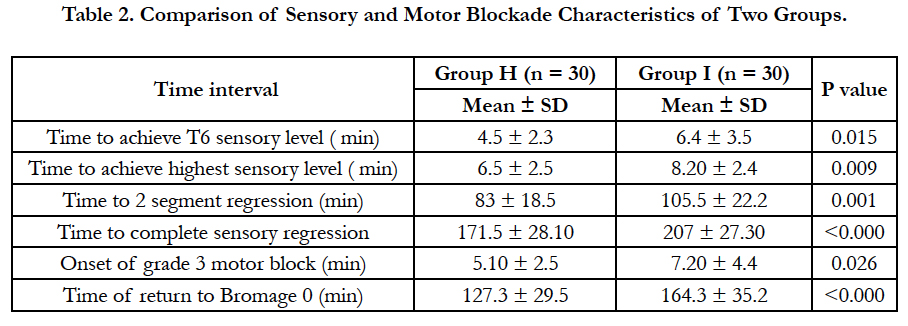
Mean time taken for achieving T6 sensory analgesia and mean time taken for attaining maximum sensory level was shorter in group H than group I (P < 0.05). The median maximum sensory level achieved was similar in both groups. Two patients in hyperbaric ropivacaine Group and one patient of isobaric group had sensory level of T3 but no patient had sensory level above T3. This variation in degree of spread of sensory block may be attributed to baricity (2). The mean time for regression of sensory blockade level by 2 segments and mean time to complete sensory blockade regression were shorter in Group H as compared to Group I. Mean total duration of sensory analgesia was also shorter in group H. Total duration of motor blockage was significantly shorter in group H than Group I (p < 0.0001) [Table 2].
The baseline mean pulse rate and blood pressure was comparable between the two groups. There was no significant difference in change of mean pulse rate between the two groups. Both groups had fall in systolic and diastolic blood pressure and the difference in mean fall of BP was not statistically significant.
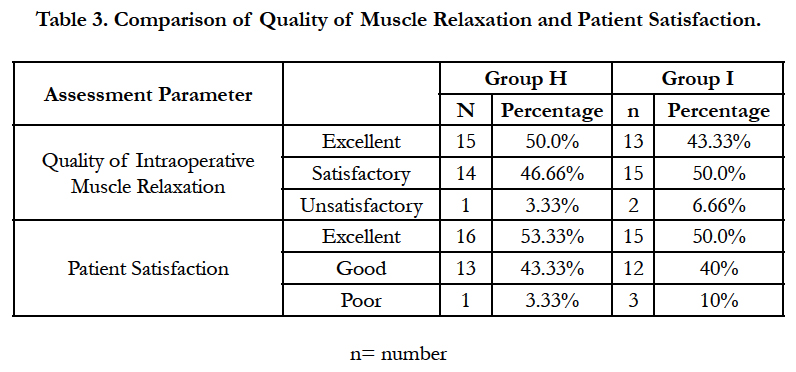
Most patients in either group (96.66% patients in group H and 90.0% patients in group I) had satisfactory analgesia but one patient in Group H and three patients from group I experienced pain during intraoperative period. Out of this, the patient from group H and two patients of group I had visual analogue score (VAS) > 3 and required rescue analgesia in the form of ketamine 10mg IV. In one patient of group I, discomfort was relieved by just assurance. Most patients in Group H 29(96.66%) and 28 (93.33%) in Group I had satisfactory or excellent muscle relaxation [Table 3].
Hypotension was observed in seven patients (23.33%) of group H and in six patients (20.0%) of group I. Three (10.0%) patients in the group H and two (6.66%) patients of group I had nausea or vomiting, which was managed by inj. Ondansetron 4mg IV. Incidences of pruritus were lesser in Group H compared to Group I (6.66% vs 13.33%) but the difference was not statistically significant. Shivering was observed in one patient (3.33%) in Group H and in two patients (6.66%) of Group I. None of the patient had respiratory depression or block higher than T3 level from either of groups [Table 4].
Discussion
We found that the rate of onset and maximum level achieved of sensory and motor blockade was shorter in group H as compared to group I. The mean time taken for regression of sensory level by 2 segments from highest sensory level attained and the mean time taken for complete sensory regression was significantly shorter in group H as compared to group I (p < 0.001). We had chosen T6 level of sensory blockade as an arbitrary study parameter to represent sufficient block level.
Khaw KS et al., [2] compared the cephalic spread and reliability between hyperbaric and isobaric ropivacaine. Hyperbaric solution tends to spread by gravity while in isobaric (plain) solution no effect of gravity assisted spread is seen and tends to concentration at segment near the site of injection. They concluded that during spinal anaesthesia in lateral position hyperbaric solution tends to spread more in cephalic direction while isobaric solution tends to concentrate at lumbar segments.
Many studies like Khaw KS et al., [2], Gupta R et al., [8], Whiteside JB et al., [9] have reported faster rate of onset and offset of sensory and motor blockade in hyperbaric solution than plain solution, but in study done by Kallio H et al., [6] they found no difference between hyperbaric and plain ropivacaine (15 mgs) in median onset of analgesia to T10, and in time taken to reach the highest level of sensory block.
Fettes PD et al., [11], compared in their study 15mg of plain and hyperbaric solution of ropivacaine for elective perennial surgery and found more rapid onset of sensory block with hyperbaric ropivacaine than isobaric solution.
Khaw KS et al., [2]; Gupta R et al., [8]; Kallio H et al., [10]; Fettes PD et al., [11] observed that median time taken for complete regression of sensory and motor blockade were significantly shorter in hyperbaric group than in isobaric group.
The addition of glucose to isobaric ropivacaine increases its density, leads to an equal distribution of drug and increase height of the block, while as isobaric ropivacaine produces less intense, unpredictable and variable height of block when given intrathecally for spinal anaesthesia [9], this can be the reason that more patients in our study from isobaric group felt some discomfort during surgery and required supplementation of analgesia and sedation with ketamine. Similar findings were observed in several studies like Khaw KS et al., [2], Gupta R et al., [8], Fettes PD et al., [11] who compared hyperbaric and isobaric ropivacaine for spinal anaesthesia and found higher incidences of inadequate block, leading to supplementation with general anaesthesia in isobaric group.
In our study mean total duration of sensory analgesia was shorter in group H as compared to group I (p < 0.05) but Khaw KS et al., [2] observed that the time taken from spinal injection to the time of first analgesic request was similar between hyperbaric and isobaric groups which is in contrast to findings of our study.
Conclusion
As compared to isobaric ropivacaine (0.75%), hyperbaric ropivacaine (0.75%) provides reliable and effective spinal anaesthesia with early onset of blockade and early recovery of sensory as well as motor blockage, in geriatric patients.
References
- Khaw KS, Ngan KW, Wong ELY, Liu JYW, Chung R (2001) Spinal ropivacaine for cesarean section: a dose-finding study. Anesthesiology. 95(6): 1346–1350.
- Khaw KS, NganKee W, Wong M, Floria N, Lee A (2002) Spinal ropivacaine for cesarean delivery: a comparison of hyperbaric and plain solutions. Anesth Analg. 94(3): 680–685.
- Gupta K, Singh S, Sharma D, Gupta PK, Krishan A, et al., (2014) Intrathecal fentanyl as an adjuvant to 0.75% isobaric ropivacaine for infraumbilical surgery under subarachnoid block: A prospective study. Saudi J Anaesth. 8(1): 64–68.
- Bernard Rosner (2000) Fundamentals of Biostatistics (5th Edn), Cengage Learning, Duxbury, USA.
- Robert H Riffenburg (2005) Statistics in Medicine. (2nd edn), Academic press.
- Sunder Rao PSS, Richard J (2006) An Introduction to Biostatistics, A manual for students in health sciences. (4th edn), New Delhi: Prentice hall of India.
- Suresh KP, Chandrasekhar S (2012) Sample Size estimation and Power analysis for Clinical research studies. J Hum Reprod Sci. 5(1): 7-13.
- Gupta R, Bogra J, Singh PK, Saxena S, Chandra G, et al., (2013) Comparative study of intrathecal hyperbaric versus isobaric ropivacaine: A randomized control trial. Saudi J Anaesth. 7(3): 249–253.
- Whiteside JB, Burke D, Wildsmith JAW (2001) Spinal anaesthesia with ropivacaine 5 mg ml(-1) in glucose 10 mg ml(-1) or 50 mg ml(-1). Br J Anaesth. 86(2): 241–244.
- Kallio H, Snall EVT, Tuomas CA, Rosenberg PH (2004) Comparison of hyperbaric and plain ropivacaine 15 mg in spinal anaesthesia for lower limb surgery. Br J Anaesth. 93(5): 664–669.
- Fettes PD, Hocking G, Peterson MK, Luck JF, Wildsmith JAW (2005) Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth. 94(1): 107–111.