Cervical sagittal alignment variations and proximal junctional kyphosis after posterior fusion of AIS
Youdi Xue1MD, Limin Liu2MD, Yueming Song2MD, Zeyu Huang2MD
1. Department of Orthopaedic Surgery, Xuzhou Central Hospital, China
2. Department of Orthopaedic Surgery, West China Hospital, Sichuan University, China.
*Corresponding Author
Youdi Xue,
Department of Orthopaedic Surgery,
Xuzhou Central Hospital, China.
E-mail: xueydspine@163.com
Article Type: Research Article
Received: July 21, 2014; Accepted: August 14, 2014; Published: August 19, 2014
Citation: Youdi Xue, Limin Liu, Yueming Song, Zeyu Huang (2014) Cervical sagittal alignment variations and proximal junctional kyphosis after posterior fusion of AIS. Int J Anesth Res. 2(6), 53-58. doi: dx.doi.org/10.19070/2332-2780-1400014
Copyright: Youdi Xue© 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: To determine the changes in cervical sagittal alignment(CSA), measure the incidence of proximal junctional kyphosis(PJK) and identify the correlation between these two parameters following segmental posterior spinal instrumentation and fusion.
Materials and Methods: From May 2008 to September 2011, 35 patients after posterior instrumentation and fusion to the upper thoracic vertebra due to adolescent idiopathic scoliosis in our department were eligible for this study. Pre and post operative and the last follow-up anteroposterior and lateral radiographs of the entire spine were reviewed. The following radiographic parameters were measured: cervical sagittal alignment, proximal junctional measurement(PJM) of the cobb angle, thoracic kyphosis and lumbar lordosis. In this study, positive values were used to denote kyphosis, while the negative values were used to indicate lordosis. The correlations between cervical sagittal alignment and proximal junctional measurement were also identified.
Results: Preoperatively, the average CSA was +2.84 (range,-30.2-+35.6), and 48.6% was kyphosis (17/35); after surgery, the average CSA was +1.78 , and 51.4% was kyphosis(18/35) ; at the last follow up, the average CSA was +1.86, and 54.3% was kyphosis(19/35). Preoperatively, the average PJM was +3.87° while postoperatively, the average PJM was +8.01°, and the incidence rate of proximal junctional kyphosis was 17.1% (6/35); at the last follow up, the average PJM was +9.70°, and 28.6% was PJK (10/35). significant correlation between the CSA and PJK was found postoperatively(r=-0.302), and at the last follow up (r=-0.564).
Conclusion: Cervical kyphosis is frequent in AIS, and the change after posterior spinal fusion surgery is limited. The incidence rate of proximal junctional kyphosis is high, meanwhile there is a significant correlation between cervical sagittal alignment and proximal junctional kyphosis.
2.Introduction
3.Materials and Methods
4.Statistical analysis
5.Results
5.1 Demographic results
5.2 Radiographic results
6.Discussion
6.1 Cervical sagittal alignment
6.2 Proximal junctional kyphosis
7.References
Keywords
Adolescent idiopathic scoliosis; sagittal alignment; cervical spine; proximal junctional kyphosis.
Introduction
Many studies have demonstrated a flattening of the sagittal profile in AIS (adolescents idiopathic scoliosis), including thoracic hypokyphosis associated with flattening or kyphosis of the cervical spine [1,2]. Furthermore as sagittal imbalance has been recognized as main source of pain, disability, and poor health status outcomes, and recent reports have showed correlations between cervical kyphosis and axial symptoms, and scoliotic patients treated with surgery may have a greater incidence of cervicodorsal pain when compared with normal subjects [3,4]. So it is very important to face up to this troublesome problem, and strive to restore normal sagittal alignment in treatment of AIS.
Several studies have identified PJK (proximal junctional kyphosis) as a common phenomenon after posterior long segments fusion for deformity correction [5,6]. Although the effect of PJK on clinical symptoms and patients outcomes was still unclear [6]; pain complaints, dissatisfied self-image, even revision surgery have been documented.
As documented in studies, thoracic kyphosis is correlated to lumbar lordosis in AIS [7], and recent reports have also showed that cervical sagittal alignment(CSA) and thoracic kyphosis is correlated with each other [2,8]. Thus, as integral parts of cervico-thoracic segment of global alignment, it is justified to postulate that some correlation between cervical sagittal alignment and PJK exists to make up a globally balanced spine in the sagittal plane.
Therefore, the purpose of the current study was as follows:
1. To measure the sagittal alignment of the cervical spine and other sagittal parameters in patients with AIS, and determined the changes in cervical sagittal alignment following segmental posterior spinal instrumentation and fusion.
2. To observe the incidence of postoperative PJK in this group of patients;
3. To identify the correlation between CSA and PJK.
Materials and Methods
A retrospective chart and radiographic analysis on 35 patients with AIS who had undergone posterior instrumentation and fusion from May 2008 to January 2011. Inclusion criteria were age from 10 to 18 years at surgery, availability of anteroposterior and lateral full-spine radiographs pre and post surgery, and at least 24 months’ follow up; fusion segment expanded to the proximal thoracic spine (T1-T7). We excluded patients who were undergoing a revision surgery or had a staged or concurrent anterior procedure; in whom the upper instrumented vertebral were below T7; patients with radiographs of ill-defined skeletal landmarks which make accurate measurement difficult. The baseline data were collected about age, gender, Lenke Type classification, the number of spinal segments fused, and the duration of follow up. The following spinal parameters were measured twice in a randomized order at one week interval by two independent observers, and the mean value was recorded:
CSA: measured between the inferior endplate of C2 and the inferior endplate of C7.
Proximal junctional measurement (PJM): the caudal endplate of the UIV to the cephalad endplate of 2 supradjacent vertebrae above the UIV. PJK was defined by the following two criteria:
1.Proximal junction sagittal Cobb angle greater than or equal to 10°;
2.Proximal junction sagittal Cobb angle for the corresponding 2-level spinal segment at least 10° greater than the corresponding preoperative measurement.
Thoracic kyphosis: measured between the superior endplate of T1 and the inferior endplate of T12.
Lumbar lordosis: measured between the superior endplate of T12 and the superior endplate of S1.
Statistical analysis
The data were analyzed using the software SPSS 18.0(SPSS, Inc.,Chicago, IL, USA), Data was expressed as frequencies and percentages, and means and standard deviations as appropriate. Comparisons between variables were made using an independent samples t test. Pearson tests were used to analyze the correlation between PJK and CSA. The P value of <0.05 was considered to be significance.
Results
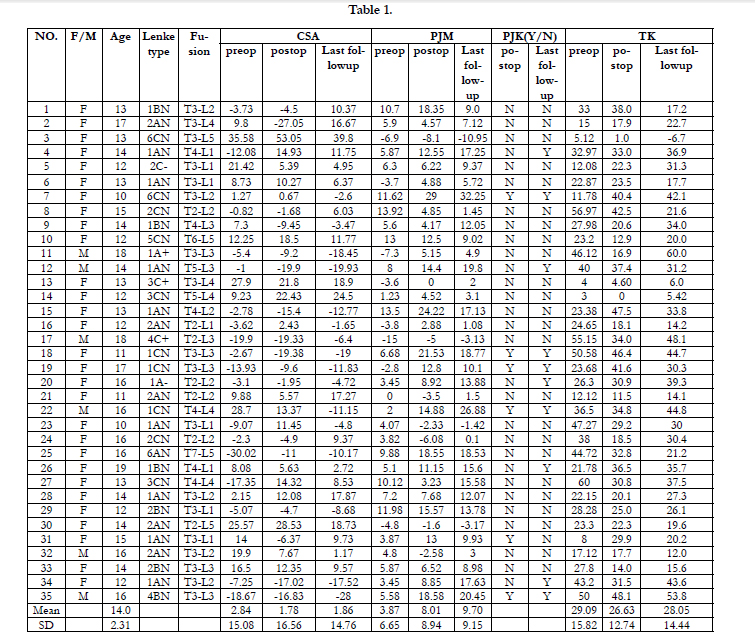
The demographic data and radiographic parameters before and after operation and at the last follow up was detailed in the Table 1.
There was 6 male, and 29 female; the average age of patients at surgery was 14.5 years(range,10-18 years); the average follow up duration is 33.2 months(range, 24-49 months). The proximal fusion level was at at T2 in 7 patients, T3 in 18 patients, T4 in 6 patients, T5 in 2 patients, T6 in 1 patient and T7 in 1 patient. The distal fusion level was at L1 in 8 patients, L2 in 10 patients, L3 in 8 patients, L4 in 5 patients, L5 in 4 patients. According to Lenke type classification, there was 16 Lenke type 1,10 Lenke type 2, 3 Lenke type 3, 2 Lenke type 4, 1 Lenke type 5, and 3 Lenke type 6 patients.
In this study, positive values were used to denote kyphosis, while the negative values were used to indicate lordosis. Preoperatively, the average CSA was +2.84 (range,-30.2-+35.6),and 48.6% was kyphosis (17/35), after surgery, the average CSA was +1.78 , and 51.4% was kyphosis(18/35) ; at the last follow up, the average CSA was +1.86, and 54.3% was kyphosis(19/35) (Fig. 1).
Figure 1. A 16-year-old boy was treated with posterior long segments fusion (T4-L4) for deformity correction of AIS(Lenke Type ICN).
(A). Radiographs of the entire spine were made before surgery, the major thoracic coronal Cobb angle was 72°, the cervical lordosis was -28.7°, the thoracic kyphosis was -36.5°, and the proximal junctional measurement (PJM) between T2 and T4 was -5.0°
(B). Four weeks after surgery ,the standing radiographs of the entire spine showed that the major thoracic coronal Cobb angle was 10.6° (85.3% correction rate), the cervical lordosis was -13.4° , the thoracic kyphosis was -34.8°, and the PJM was -12.8°.
(C). Three years later,the standing radiographs of the entire spine showed that the cervical kyphosis was inverted to lordosis(11.2°), and the phenomenon of PJK was present with the sagittal Cobb angle between T2 to T4 was -26.9°(21.9° increase compared to preoperative). This was very interesting, and the reason may due to the correlation between cervical sagittal alignment and PJK exists to make up a globally balanced spine in the sagittal plane. However the patient did not complain of any pain or cosmetic problems on this area.
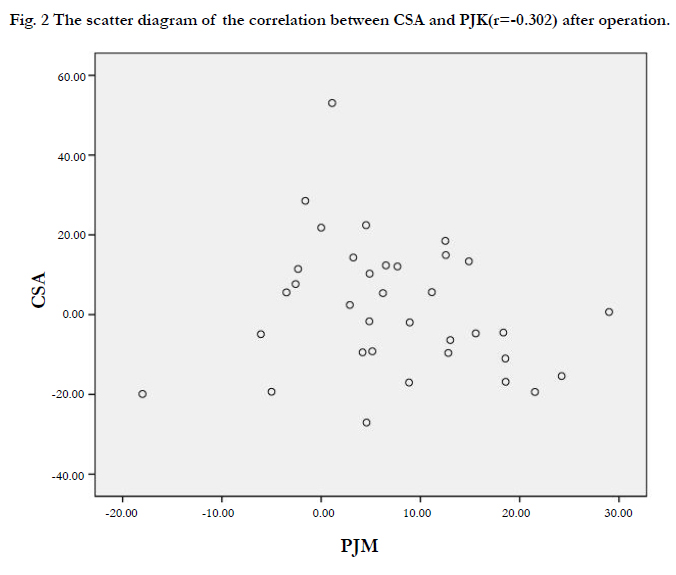
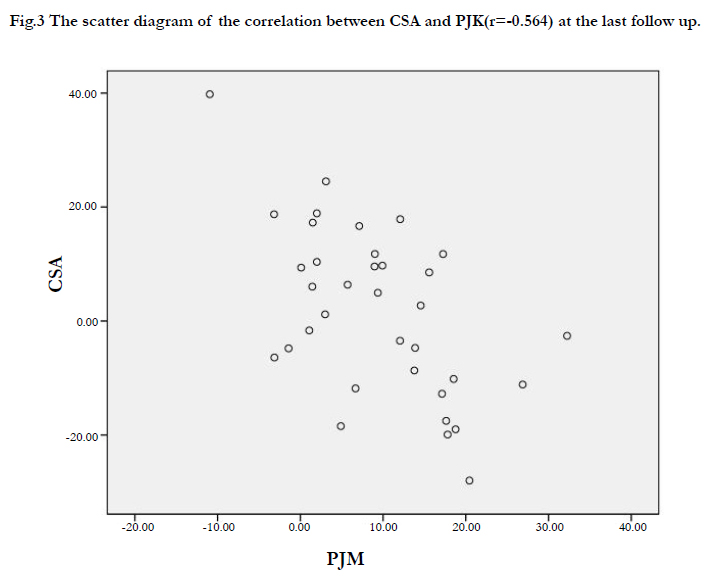
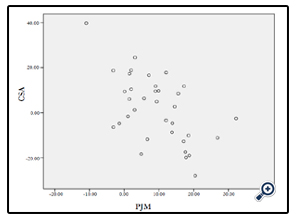
Preoperatively, the average PJM was +3.87° ; while postoperatively, the average PJM was +8.01°, and at the last follow up, the average PJM was +9.70°. According to the definition of PJK, 17.1% (6/35) of all patients presented with PJK after operation, and 28.6% (10/35) at the last follow up. Depend on the statistical test, significant correlation between the CSA and PJK was found postoperatively(r= -0.302, Fig.2), and at the last follow up (r= -0.564, Fig.3).
Abnormal spinopelvic balance and pelvic morphology with flattened spinal sagittal profile is common in AIS [10]. The recent reports have presented the phenomenon that hypokyphotic thoracic spine coexisting with hypolordosis or kyphotic cervical spine. Hilibrand et al.[8] found an inverse correlation between thoracic kyphosis and cervical kyphosis, and postulated that it was a compensatory fashion to maintain forward view, or just a simply continuation of the sagittal misalignment of thoracic lordosis [8,11]. Recent publications have shown a correlation between cervical kyphosis and axial neck pain or new-onset neurologic symptoms [12, 13]. Alteration of normal cervical lordosis, thoracic kyphosis, and lumbar lordosis has been associated with symptomatic pain and accelerated disc degeneration. Neck pain was a major complaint found by Moscowitz et al. after long term follow up of scoliosis fusion, although they did not comment on the sagittal alignment of the cervical spine [14]. Although kyphosis in the cervical spine is often considered pathologic, cervical hypolordosis or kyphosis may be normal variant in asymptomatic children with no known spinal pathology, and the clinical significance of these changes in sagittal shape remains to be determined [15,16].
In our study, the average CSA was +2.84°, and 48.6% was kyphosis, and the average thoracic hypokyphosis was also documented at preoperative full-length lateral radiograph. At the last follow up, the average CSA was +1.86°, and 54.3% was kyphosis, our findings was accordant with previous study, and this may due to the inherent rigidity of the cervical spine, because of wedging-shaped vertebrae and kyphotic inter-vertebral spaces [2,17].
PJK after posterior multiple segmented fusion for AIS has been documented about several decades. However, there are only a few studies focus on this phenomenon, and the cause and effect is still not well appreciated [18,19].
The risk of developing PJK above a spinal deformity fusion is 17% to 39%, with most noted by 2 years postoperative [20]. In this study, 17.1% patients developed PJK after surgery, while increasing to 28.6% at the last follow up after surgery. Although the presence of PJK may not result in significantly differences in clinical outcomes, but sometimes it can be cosmetically unappealing and symptomatic, occasionally necessitating revision surgery [21]. Some studies have demonstrated posterior compression correction techniques and decreased thoracic kyphosis as potential factors in developing PJK [22,23]. Other studies found that preoperative sagittal malalignment and imbalance demonstrated a significant relationship with the incidence of PJK [21], and nonanatomic restoration of thoracic kyphosis increased PJK risk [24]. According to these studies, we may be concluded that there is a delicate balance among spine region, and the presence of PJK is the consequence of the unfused segment to endeavor to balance the imbalanced global sagittal alignment, which may be minimized by postoperative normalization of global sagittal alignment[25,26,27].
The correlation between CSA and PJK
In this study, we tried to determine the correlation of CSA with PJK, and significant correlation between the CSA and PJK was
found postoperatively(r= -0.302), and at the last follow up (r= -0.564). To say in other words, there is significant positive correlation between cervical lordosis and PJK. In fact, in this study, all PJK were present in the cases with cervical lordosis.
Several studies have found that cervical hypolordosis or kyphosis coexists with a loss of thoracic kyphosis, and corrections in thoracic sagittal alignment were accompanied with inverse change in cervical sagittal alignment[2]. Hilibrand et al. [8]found the greatest cervical kyphosis in patients with thoracic hypokyphosis, and hypothesized these changes occur to try to maintain forward view. Cruickshank et al. [28]observed that an area of lordosis must be balanced by kyphosis above and below that area; this demonstration was proved to be correct three decads later. These studies find the cervical sagittal imbalance is correlated with global spine alignment, and the correlation of each part of the global sagittal alignment can be explained by coupled motion principle [17,29].
In this study, the correlation between CSA and PJK can also explained by coupled motion principle, and the compensatory change of CSA and PJK developed to maintain horizontal gaze and balance the global sagittal alignment.
In conclusion, both CSA and PJK is integral part of the global sagittal alignment, and be correlated with each other to maintain horizontal gaze and balance the global alignment.
References
- Pierre Roussouly , Hubert Labelle , Jihane Rouissi , Arnaud Bodin. Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults.Eur Spine J (2013) 22 (Suppl 2):S203–S215.
- Federico Canavese , Katia Turcot , Vincenzo De Rosa. Geraldo de Coulon. Andre´ Kaelin. Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic Scoliosis. Eur Spine J (2011) 20:1141–1148.
- Edgar MA, Metha MH (1988) Long-term follow-up of fused and unfused idiopathic scoliosis. J Bone Joint Surg Br 70:712–716.
- Harrison DD, Harrison DE, Janik TJ et al (2004) Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine 29:2485–2492.
- Lee GA, Betz RR, Clements III DH, et al. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine 1999;24:795–9.
- Yongjung J. Kim, MD, Keith H. Bridwell, MD, Lawrence G. Lenke, MD, Junghoon Kim, MD, and Samuel K. Cho, MD. Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis Following Segmental Posterior Spinal Instrumentation and Fusion. Minimum 5-Year Follow-up. SPINE 2005. Volume 30, Number 18, pp 2045–2050.
- Upasani VV, Tis J, Bastrom T, Pawelek J, Marks M, Lonner B, et al.: Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ?. Spine (Phila Pa 1976) 32:1355–1359, 2007.
- Hilibrand AS, Tannenbaum DA, Graziano GP, Loder RT, Hensinger RN (1995) The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J Pediatr Orthop 15:627–632.
- Majdouline Y, Aubin CE, Robitaille M, et al. Scoliosis correction objectives in adolescent idiopathic scoliosis. J Pediatr Orthop 2007;27:775–781.
- Mac-Thiong JM, Labelle H, Charlebois M, et al. (2003) Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine 28:1404–1409.
- Deacon P, Flood BM, Dickson RA. Idiopathic scoliosis in three dimensions. J Bone Joint Surg[Br], 1984;66:509-512.
- Katsuura A, Hukuda S, Saruhashi Y et al (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 10:320–324.
- Harrison DD, Harrison DE, Janik TJ et al (2004) Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine 29:2485–2492.
- Moscowitz A, Moe JH, Winter RB, Binner H. Long term follow up of scoliosis fusion. J Bone J Surg[Am] 1980;62:364-375.
- Harrison DD, Troyanovich SJ, Harrison DE, et al. A normal sagittal spinal configuration: a desirable clinical outcome. J Manipulative Physiol Ther. 1996;19:398–405.
- Choon Sung Lee, Hyounmin Noh, Dong-Ho Lee, Chang Ju Hwang, Hyoungmin Kim, Samuel K. Cho. Analysis of Sagittal Spinal Alignment in 181 Asymptomatic Children. J Spinal Disord Tech 2012;25:E259–E263.
- Miao Yu, Clement Silvestre, Tanguy Mouton, Rami Rachkidi, Lin Zeng, Pierre Roussouly
- Lee GA, Betz RR, Clements III DH, Huss GK: Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine 24:795–799, 1999.
- Kim HJ , Yagi M , Nyugen J , et al. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis . Clin Orthop Relat Res 2012 ; 470 : 1633 – 9.
- Han Jo Kim, Lawrence G. Lenke, Christopher I. Shaffrey, Ellen M. Van Alstyne, Andrea C. Skelly, Andrea C. Skelly. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery.A systematic review. Spine Volume 37, Number 22S, pp S144–S164 2012.
- Mitsuru Yagi, King B Akilah BA, Oheneba Boachie-Adjei. Incidence, Risk Factors and Classification of Proximal Junctional Kyphosis: Surgical Outcomes Review of Adult Idiopathic Scoliosis. SPINE Volume 36, Number 1, pp E60–E68.
- Rhee JM, Bridwell KH, Clements DH, et al. Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine 2002;27:2350–2356.
- Melvin D. Helgeson, Suken A. Shah,Peter O. Newton, Evaluation of Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis Following Pedicle Screw, Hook, or Hybrid Instrumentation. SPINE Volume 35, Number 2, pp 177–181 2010.
- Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643–9.
- Shu-Hua Yang, Po-Quang Chen. Proximal Kyphosis After Short Posterior Fusion for Thoracolumbar Scoliosis. CLINICAL ORTHOPAEDICS AND RELATED RESEARCH 2003 Number 411, pp. 152–158.
- Kim YJ , Bridwell KH , Lenke LG , et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up . Spine (PhilaPa 1976) 2008 ; 33 : 2179 – 84 .
- Mendoza-Lattes S , Ries Z , Gao Y , et al. Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J 2011 ; 31 : 199 – 206 .
- Cruickshank JL, Koike M, Dickson RA. Curve patterns in idiopathic scoliosis. J Bone J Surg [Br] 1989;71:259- 263.
- Pierre Roussouly, Hubert Labelle, Jihane Rouissi, Arnaud Bodin Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults Eur Spine J (2013) 22 (Suppl 2):S203–S215.