Anticancer Property of Incudent Tooth Paste Formulation
Singhal RK*
Professor and Head, Department of Conservative Dentistry and Endodontics, Maharana Pratap College of Dentistry and Research Centre, Gwalior (M.P), India.
*Corresponding Author
Dr. Rajnish K Singhal, MDS,
Professor and Head,
Department of Conservative Dentistry and Endodontics,
Maharana Pratap College of Dentistry and Research Centre,
Gwalior (M.P), India.
E-mail: rajnishksinghal@gmail.com
Recieved: November 15, 2016; Accepted: November 29, 2016; Published: December 16, 2016
Citation: Singhal RK (2016) Anticancer Property of Incudent Tooth Paste Formulation. J Translational Space Dentistry Med Explor. 1(2), 5-7.
Copyright: Singhal RK© 2015. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Oral leukoplakia which is a major problem in countries with prevalent tobacco use, has been closely linked with inflammation. Twenty patients with oral leukoplakia along with 20 normal healthy control subjects who satisfied all inclusion and exclusion criteria, were included in the study. All subjects brushing twice per day with new tooth paste formulation. Tooth paste formulation induced the disappearance of clinical sign and symptoms. Levels of inflammatory cytokine in serum and saliva were examined just prior to start brushing with new tooth paste and after clinical improvement of precancerous lesions. In contrast to normal healthy subjects, levels of TNF-alpha, IL-6, and IL-8 in serum and saliva showed statistically significant increased in patients with oral leukoplakia. These levels significantly decreased in all groups after brushing. Pain scores and size of lesion in oral leukoplakia improved significantly. Based on these results we conclude that new formulation active ingredient mediates its beneficial effects in patients with oral leukoplakia through the suppression of proinflammatory cytokines.2.Introduction
3.Materials and Methods
4.Results and Discussion
5.Discussion
7.References
Keywords
Herbal Formulation; NF-kappa B; Precancerous Lesions; Serum; Salivary; Anticancer.
Introduction
Oral cancer is the sixth commonest cancer in the world [1]. Its incidence is predominantly high in India specially north India, some other countries in Asia, and in certain places in the western hemisphere. It has been reported that 90% of oral cancers in India among men were attributable to chewing and smoking habits. In India, the age standardized incidence rate of oral cancer is 12.6 per 100 000 population [2]. Oral squamous cell carcinoma develops through a multi-step process of genetic, epigenetic and metabolic changes resulting from exposure to carcinogens [3]. The initial presence of a precursor subsequently developing into cancer is well-established in oral cancer [4]. Oral leukoplakia, submucous fibrosis, lichen planus are major known precursor lesions. Only 8-10% of these lesions ultimately turn into malignancy [5]. Ability to clinically predict malignant transformation is limited and routine histopathological diagnosis has limited its prognostic value. Inspite of advances of technologies in early detection of oral precancerous and cancerous lesions, there are limitations for its use such as, the diagnosis is essentially subjective, all lesions exhibiting dysplasia do not eventually become malignant and some may even regress, and carcinoma can develop from lesions in which epithelial dysplasia was not diagnosed in previous biopsies [6, 7]. Therefore, it is necessary to develop other methods for predicting the malignant potential of pre-malignant lesions and preventive measures [7].
Recently, strong evidences have been suggested that the nuclear factor-κB (NF-κB) signaling pathway plays a critical role in carcinogenesis, protection from apoptosis and chemoresistance in a number of cancer types, including head and neck cancer, breast cancer, hepatocellular carcinoma and gastric cancer [8-12]. Recently, accumulating evidence suggested that the NF-kappa B dependent cytokine levels in saliva and tissue specimens of patients with oral premalignant lesions are elevated [13]. So, an agent that can target NF-kappaB dependent cytokine of attention for prevention and treatment of oral precancerous lesions. Various dentifrices have available in market for prevention of oral diseases. Recently , one formulation of anticancer tooth paste has been proposed. This study was planned to study the find the anticancer properties by using salivary biomarkers nuclear factor-κB (NF- κB)in oral leukoplakia.
Materials and Methods
The patients clinically and histopathologically confirmed as oral leukoplakia and Oral sub-mucous fibrosis were recruited for this study based on the definition of oral cancer and precancerous by the World Health Organization. Healthy normal served as the control group. All subjects neither had smoking history and detectable gingival and/or periodontal inflammation, nor any visible oral lesions under careful examination; moreover, they had not received any treatments for the oral lesions within 90 days prior to the specimen collection, and had no history, symptoms and/or signs of systematic infections and other diseases. The conventional histopathological diagnosis was made by one oral pathologist. This study was approved by the Ethical committee of diagnostic study and informed consents were obtained from all subjects. This was a nonrandomized and phase II trial of herbal tooth paste formulation known as Incudent, Denmark and we are treating on the 20 oral leukoplakia who satisfied all inclusion and exclusion criteria. Patients brush daily and keep the semisolid of paste in mouth for 2-3 minutes till clinical sign and symptoms disappeared. Systemic and local adverse events were assessed using the National Cancer Institute expanded Common Toxicity Criteria version 3.0. Pain control and lesion healing were the 2 main clinical variables for evaluating of oral leukoplakia. we used a visual scale analog ranging from 0.5 (very mild pain) to 5 (severe pain). Clinical and histopathological examinations were conducted, along with collection of serum and salivary samples prior to starting brushing with this formulation. Clinical and histopathological examinations were again performed and along with collection of serum and salivary samples. For each sample, 1.0 ml of supernatant was used for the enzyme-linked immunoassay (ELISA) cytokine assays by using the human ELISA kit for TNF-a, IL-6, and IL-8 (R&D Systems Inc., Minneapolis, MN, USA), according to the manufacturer’s instructions.
Results and Discussion
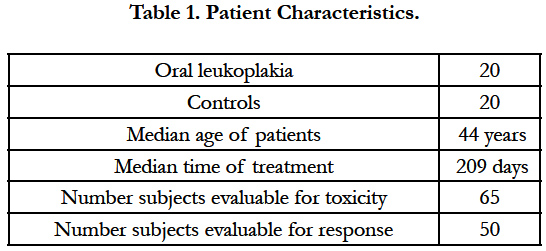
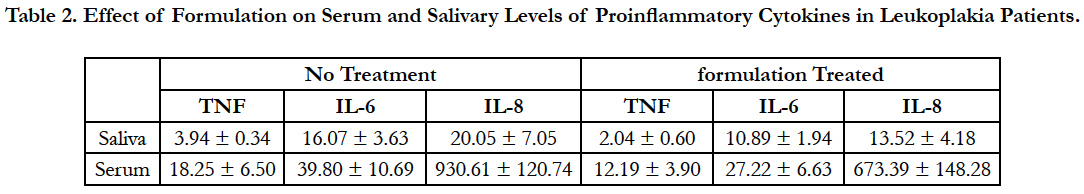
The patient characteristics were showed in Table-1. No difference in TNF-alpha, IL-6, and IL-8 levels in serum and salivary were found in vegetarian and non-vegetarian (data were not shown). Also, further no difference in TNF-alpha, IL-6, and IL-8 levels in serum and salivary were found in females and males (data were not shown). The value of serum and salivary TNF-alpha, IL-6, and IL-8 showed statistically significant increased in oral leukoplakia in contrast to normal healthy subjects; while it significantly decreased in all groups after formulation (Table-2-7, P<0.05). Serum and salivary correlation analysis revealed strong and highly significant correlation for TNF-alpha, IL-6, and IL-8 in all groups (r=0.64, r=0.61, r=0.62, P<0.001) respectively. Furthermore, the values were statistically significant after clinical improvement of diseases. Pain scores and size of lesion in oral leukoplakia improved significantly (p < 0.05). The oral leukoplakia was significantly improved 234+/-15, days respectively after using new formulation. The goal of this study is to determine whether the anticancer effects of new formulation are mediated through inhibiting NF-kappa B dependent cytokine. Our results suggest that formulation significantly increased the local and systemic inhibiting NF-kappa B dependent cytokine, decreased levels of TNF-alpha, IL-6, and IL-8 in all groups after brushing and rinsing mouth with new formulation in precancerous lesions. Furthermore, the values were statistically significant after clinical improve of diseases. Pain scores and size of lesion in oral leukoplakia improved significantly. We did not record any treatment-related toxic effects, even brushing more than twice a day of keep it for more than two minutes. The significant correlation was observed in serum and salivary markers in all groups. Since, saliva can be easily collected; measurement of biomarkers of diseases may prove useful in early detection of oral cancer risks. Moreover, the salivary analysis for oral diagnosis may prove a cost effective method for screening large populations.
Table 2. Effect of Formulation on Serum and Salivary Levels of Proinflammatory Cytokines in Leukoplakia Patients.
References
- Parkin DM, Pisani P, Ferlay J (1993) Estimates of worldwide incidence of eighteen major cancers in 1985. Int. J. Cancer. 54(4): 594–60.
- Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 31(1):3–24.
- Lippman SM, Hong WK (2001) Molecular markers of the risk of oral cancer. N Engl J Med. 344(17): 1323-26.
- Reibel J (2003) Prognosis of oral premalignant lesions: Significance of clinical, histological, and molecular biological characteristics. Crit Rev Oral Biol Med. 14(1): 47-62.
- Gupta PC, Bhonsle RB, Murti PR, Daftary DK, Mehta FS, et al., (1989) An epidemiologic assessment of cancer risk in oral precancerous lesions in India with special reference to nodular leukoplakia. Cancer 63(11): 2247-52.
- Allison P, Locber S, Feinac J (1998) The role of diagnostic delays in the prognosis of oral cancer: a review of literature. Oral Oncol. 34(3): 161-70.
- Rai B, Kaur J, Jacobs R (2011) Direct tissue fluorescence imaging in relation to tissue, serum and salivary protoporphyrin for oral pre-cancerous and cancerous lesions. Oral Oncology. 47(1): 37.
- Wang CY, Mayo MW, Baldwin AS Jr (1996) TNF- and cancer therapyinduced apoptosis: potentiation by inhibition of NF-kappaB. Science. 274(5288): 784-87.
- Pai SI, Westra WH (2009) Molecular pathology of head and neck cancer: implications for diagnosis, prognosis, and treatment. Annu Rev Pathol. 4: 49-70.
- Pikarsky E, Porat RM, Stein I, Abramovitch R, Amit S, et al., (2004) NFkappaB functions as a tumour promoter in inflammation-associated cancer. Nature. 431(7007): 461-66.
- Aggarwal BB (2004) Nuclear factor-kappaB: the enemy within. Cancer Cell. 6(3): 203-8.
- Shishodia S, Aggarwal BB (2004) Nuclear factor-kappaB activation mediates cellular transformation, proliferation, invasion angiogenesis and metastasis of cancer. Cancer Treat Res. 119: 139-73.
- Rhodus NL, Ho V, Miller CS, Myers S, Ondrey F (2004) NF-kappaB dependent cytokine levels in saliva of patients with oral preneoplastic lesions and oral squamous cell carcinoma. Cancer Detect Prev. 29(1): 42-5.