Effects of Age And Gender On Short-Term Weight Loss And Long-Term Weight Maintenance
Frank Dong1*, Justin B. Moore2, Elizabeth Ablah1, Bobbie G. Paull-Forney2, Tracie Collins1
1 Department of Preventive Medicine and Public Health, University of Kansas School of Medicine-Wichita,Kansas, USA.
2 Department of Internal Medicine, University of Kansas School of Medicine-Wichita, Kansas, USA.
*Corresponding Author
Dr. Frank Dong
University of Kansas School of Medicine-Wichita,
1010 N Kansas St, Wichita, KS, USA.
Tel: 316-293-2627; Fax: 316-293-2695
E-mail: fdong@kumc.edu
Received: January 17, 2014; Accepted: February 15, 2014; Published: February 17, 2014
Citation: Dong F, et al. (2014). Effects of Age and Gender on Short-Term Weight Loss and Long-Term Weight Maintenance, Int J Translation Community Dis, 02(01), 06-12. doi: dx.doi.org/10.19070/2333-8385-140002
Copyright: Dong F© 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To determine if there are differences in short-term weight loss and long-term weight maintenance success by age or gender.
Methods: Patients were enrolled in a Midwestern weight loss clinic. The primary outcome measures were short-term weight loss success (achieving ≥ 10% of the initial body weight loss (IBWL) at three months) and long-term weight maintenance success (maintaining ≥ 10% IBWL at one year).
Results: Patients 18 – 45 years were more likely to achieve short-term weight loss success compared to those in the two other age categories (45-64 and ≥ 65 years). However, age was not a significant predictor for long-term weight maintenance success. Females had decreased odds (OR=0.47, 95% CI 0.38, 0.59) of achieving short-term weight loss success, but had increased odds (OR=1.94, 95% CI 1.02, 3.67) of achieving long-term weight maintenance success.
Discussion: Age and Gender effect were different for short-term weight loss and long-term weight maintenance success.
2.Introducation
3.Methods
3.1.Patients
3.2.Instrument
3.3.Procedures
3.4.Dependent and Independent Variables
3.5.Statistical Analysis
4.Results
5.Discussion
6.Limitations
7.Conclusion
8.References
Keywords
Weight Loss; Low-Calorie Diet; Percentage of Initial Body Weight Loss.
Introduction
Obesity, defined as a body mass index (BMI) greater than or equal to 30.0 kg/m2, affects more than onethird (35.7%) of US adults [1]. The prevalence of obesity in those aged 60 years and older (28.0%) is lower than among those aged 40 to 59 years (32.2%) [2]. Obesity is associated with impaired health-related quality of life, disability and fatigue [3,4], and with various medical conditions such as diabetes [5], hypertension, cardiovascular disease [5,6], knee replacement [5], and musculoskeletal disorders [6-8]. These conditions impact the elderly especially hard; those aged 65 years and older are more than eight times as likely as those aged 18 to 44 years to have been diagnosed with diabetes [2].
Obesity is an expensive risk factor. Finkelstein and colleagues reported that obese patients incur 46% increased inpatient costs, 27% more physician visits and outpatient costs, and 80% increased spending on prescription drugs when compared to normal weight controls [9], with annual extra medical costs attributable to obesity in the United States estimated at $75 billion in 2003 [10]. Weight reduction is generally a costeffective intervention: for each 1% reduction in body weight, lifetime medical expenditures may decline by $440 for overweight and obese patients [11].
To reduce the prevalence of obesity, a medical weight loss program incorporating dietary changes and increased physical activity is a feasible alternative to bariatric surgery or pharmacotherapy, particularly for patients who cannot undergo metabolic or bariatric surgery[12,13]. Research has documented that a lowcalorie diet can result in a mean weight loss of up to 13 kilograms over a 24-week period among obese patients [14].
Although research evaluating such programs has been conducted, very little research has explored if there are differences in short-term weight loss and long-term weight maintenance success by age or gender. Busetto et al. reported that 18% (5/28) of the older adults (65- 80 years) in their study achieved ≥ 10% of their initial body weight loss (IBWL) at one year, whereas 38% (18/47) of the younger adults (18-64 years) achieved the same goal [15]. Their study concluded that being younger (18-64 years), being female, and having a lower baseline BMI were the only significant predictors for achieving ≥ 10% of their IBWL at one year [15]. However, the small sample size (N=75) reduced statistical power to reveal potentially significant factors.
Additionally, achieving short-term weight loss success (>= 10% IBWL) during the intensive weight loss phase may predict achieving long-term weight maintenance success [16-18].
The objective of this study was to identify if there is a difference in the short-term weight loss or long-term weight maintenance success by age or gender among adults who participated in a weight loss program. Additionally, we sought to identify significant predictors for short-term weight loss success and long-term weight maintenance success.
Methods
The study sample included obese (BMI ≥ 30 kg/m2) men and women 18 years or older. This study included patients who were enrolled in a medically supervised weight loss program at Via Christi Weight Management clinic (VCWM) in Wichita, Kansas between 2003 and 2012. Patients were required to remain in the program for a minimum of 3 months (Phase 1,weight loss phrase) and they could choose to stay in the program for as long as they want (Phase 2, weight maintenance phrase). Individuals were excluded from participation if they met at least one of the following criteria: younger than 18 years old, pregnant, breastfeeding, active substance abuse, active eating disorder or behaviors, severe liver disease, renal failure, an active malignancy, or a wasting disease (i.e., Cushing’s syndrome, bacterial endocarditis, osteomyelitis, or tuberculosis).
The clinic maintains an electronic database of patients who have voluntarily enrolled and attended weight loss counseling classes. Detailed patient questionnaires were used by VCWM to obtain participant demographics, history of attempts at weight loss, obesity- associated conditions, and current medications. Height, weight, blood pressure, and waist circumference were collected and verified by medical staff during the initial screening period, prior to the program start. Data points for each participant in weight loss and maintenance phases were entered into the clinical database at routine intervals. Body height was measured to the nearest 0.003 meter (0.1 inch) without shoes. Body weight was measured to the nearest 0.05 kg (0.1 pound) with light clothing and no shoes at baseline and at all treatment visits.
Data were de-identified before the analysis to protect patient privacy. The Human Subjects Committee at the University of Kansas School of Medicine-Wichita and the Institutional Review Board at Via Christi Health approved this study. All patients’ clinical measures were entered into the original clinical database.
The medically supervised low-calorie diet (LCD) program limits clients’ food choices to Health Management Resource (HMR®) meal replacements (shakes, soup, cereal packets, entrees) during the weight loss phase (Phase 1). Weight loss participants must intake a minimum of five meal replacement packets and two vitamin-mineral tablets per day and may choose to intake HMR entrees as needed (consuming a minimum of 800 kcal per day). All Phase 1 patients attended weekly health education classes for three months where they were taught basic principles of weight loss and weight management. When clients achieved their weight loss goal or lost their weight loss momentum (defined by prospective criteria), they entered the weight maintenance phase (Phase 2). Phase 2 includes a weekly weigh in and a 60-minute class emphasizing the following components: weekly attendance, midweek check-in call, daily record keeping, greater than or equal to 14 servings of meal replacements per week, greater than or equal to 35 one-cup servings of vegetables and fruits per week, and greater than or equal to 2,000 kcal of physical activity per week. Patients are encouraged to participate in the weight maintenance phase for a minimum of 12 months.
Two primary dependent variables were the short-term weight loss success and long-term weight maintenance success. Short-term weight loss success was defined as achieving ≥10% IBWL at three months, consistent with the National Institute of Health guidelines [19]. The long-term weight maintenance success was defined as maintaining ≥ 10% IBWL at one year post initial enrollment in the program [20].
Four independent variables were included in the model: baseline weight, age (categorical variable; <45 years, 45 to 64 years, and ≥ 65 years), gender, and weight loss status at three months (dichotomous variable; achieved ≥10% IBWL or achieved <10% IBWL at three months).
All statistical analyses were conducted using SAS for Windows version 9.3 (Cary, North Carolina). Descriptive statistics were presented as frequencies and percentages for categorical variables (e.g., gender) and means and standard deviations for continuous variables (e.g, age).
An analysis of variance (ANOVA) was conducted to identify the difference in weight loss among the three age groups. Generalized linear mixed regression analysis was conducted to compare the percentage of weight loss among the three age groups. Chi-square test was conducted to identify the proportion of patients achieving ≥ 10% IBWL among the three age groups. Separate logistic regression analyses were conducted to identify significant predictors of achieving two distinct outcomes: short-term weight loss success and long-term weight maintenance success. The selection of variables was conducted in a stepwise fashion. All statistical analyses were two-sided. P-value <0.05 was considered to be statistically significant.
Results
Among the 2,054 adults who finished the three-month medical weight loss program, 1,534 (74.2%) remained in the program for more than three months but less than one year (the “drop-out group”). The other 520 (25.3%) adults stayed in the program for at least one year (the “completer group”). Among the overall population, 93.4% (n=1,891) were Caucasian, 66.7% (n=1,369) were female, and more than half (58.2%, n=1,195) were between 45 and 64 years (Table 1). Approximately three-quarters (72.3%, n=1,484) achieved ≥ 10% initial body weight loss (%IBWL) at three months. Chi-Square analysis was conducted to determine the difference of the demographic variables between the completer and drop-out group. The completer group had a significantly higher proportion of females (71.4% vs. 65.1%), Caucasians (96.5% vs. 92.3%), patients 45-64 years (64.2% vs. 56.2%) and ≥ 65 years old (12.9% vs. 6.6%). Additionally, 81% of the completer group achieved ≥ 10% IBWL at three months, whereas 69% of the drop-out group achieved ≥10% IBWL at three months.
Figure 1, 2 and 3 presented the result of participants’ performance in terms of achieving ≥10% IBWL at two separate study endpoints, three months and one year, stratified by age category (<45 years, 45-64 years,and ≥65 years) and gender. Among participants who stayed in the program for more than three months and less than one year, the average percentages of IBWL ≥10% at three months were 74.6%, 67.2%, and 58.4% for the 18-44 years, 45-64 years, and ≥65 years groups, respectively (Figure 1, combined gender category). Additionally, for each age category, men were more likely to achieve the short-term weight loss success (Figure 1).
Figure 1: Percentage of patients achieving IBWL ≥ 10% at three months for those who stayed in the program for more than three months but less than one year
Figure 2: Percentage of patients achieving IBWL ≥ 10% at three months for those who stayed in the program for more than one year
Figure 3: Percentage of patients achieving IBWL ≥ 10% at one year for those who stayed in the program for more than one year
A similar pattern was observed in those who stayed in the program for more than one year: the average percentages of short-term weight loss success were 82.4%, 82.9%, and 68.7% for the 18-44 years, 45-64 years, and ≥65 years groups, respectively (Figure 2, combined gender category). Men were also more likely to achieve short-term weight loss success across all three age categories (Figure 2). At the end of one year, the percentages of long-term weight maintenance success were 77.3%, 79.3% and 74.6% for the 18-44 years, 45-64 years, and ≥65 years groups, respectively (Figure 3). Within each age category, an inconsistent pattern appeared on achieving long-term weight maintenance success between males and females. For the 18-45 years group, 70% of males achieved long-term weight maintenance success, whereas 79.8% of females achieved long-term weight maintenance success. For the other two age groups, men were more likely to achieve longterm weight maintenance success.
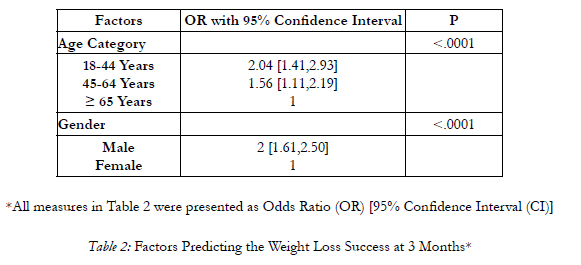
Two logistic regression analyses were conducted to identify predictors associated with short-term weight loss success and long-term weight maintenance success. Predictors for short-term weight loss success included gender, age group (18-44 years, 45-64 years, and ≥65 years), and baseline weight. The results of this analysis were presented in Table 2. Patients had increased the odds of achieving short-term weight loss success if they were male (OR=2.0, 95% CI 1.61, 2.50) and age 18-44 years (OR=2.04, 95% CI 1.41, 2.93) and age 45-64 years (OR=1.56, 95% CI 1.11, 2.19) as compared to older patients (aged ≥ 65 years).
Another logistic regression analysis was conducted to identify factors predicting long-term weight maintenance success (achieving ≥ 10% IBWL at one year). The findings were presented in Table 3. Patients were more likely to maintain ≥ 10% IBWL at one year if they were female (OR=1.94, 95% CI 1.02, 3.67), had a higher baseline weight (OR=1.08, 95% CI [1.04, 1.14] for every five kilograms increased in the baseline weight), and had achieved ≥ 10% IBWL at three months (OR=7.76, 95% CI [4.58, 13.3]). Age was not a significant predictor for long-term weight maintenance success.
Discussion
Age and gender play different roles for short-term weight loss success and long-term weight maintenance success. Younger adults and males in our study had increased odds of achieving short-term weight loss success (achieving ≥ 10% IBWL at three months). However, females were more likely to achieve long-term weight maintenance success (achieving ≥ 10% IBWL at one year) compared to males. Age was not associated with long-term weight maintenance success. Additionally, baseline weight was not a significant predictor for achieving the short-term weight loss success; however, it was a significant predictor for achieving long-term weight maintenance success.
Maintenance of long-term weight loss goals has been demonstrated to be a challenge [21-24]. The study population also suffered a high dropout rate at one year. But among the 520 adults who remained in the program for at least one year, 78.3% maintained ≥ 10% IBWL, a rate significantly higher than the 3%- 20% reported in the literature. [15,25-29] Prior studies suggest that eating less fat, exercising more, and using prescription weight loss medications were associated with increased odds of losing ≥ 10% IBWL [29].
Patients 18-44 and 44-65 years were more likely to achieve the short-term goal of ≥ 10% IBWL at threemonths compared to those ≥ 65 years. However, in our population, age was not a statistically significant predictor of maintaining ≥ 10% IBWL at one year. This differs from other research [28,30], a difference that might be partially attributable to different cutoffs for measuring weight loss success. For example, Lloyd and Khan reported that persons who successfully achieved weight loss goal at three months (defined as achieving only > 5% initial body weight loss) were more likely to be older, male, and obese class I (BMI 30.0-34.9 kg/ m2) [30]. Other differences may stem from the source of the data. For one-year outcomes, Kraschnewski et al. reported that adults 75-84 years had increased odds of achieving ≥ 10% IBWL compared to those 20-34 years [28]. However, their analyses were based on the self-reported data from National Health and Nutrition Examination Survey, whereas this current study used clinically measured data.
It is also worthwhile to point out the fact that for the older adult population (age ≥ 65years), 68.7% achieve the short-term weight loss success (≥ 10% IBWL at three months), and 74.6% of the same population achieve the long-term weight maintenance success (≥10% IBWL at one-year). Our projects demonstrated that long-term weight maintenance success is feasible and promising through the lifestyle intervention. Similar finding were reported by other researchers [31-33]. Older adults should be encouraged to stay in the weight loss program, despite the slow progress of losing weight at the end of three months.
Baseline weight was a significant predictor for longterm weight maintenance but not for short-term weight loss success. This result differs from other research. Høie and Bruusgaard concluded that baseline weight was a significant predictor for short-term but not long-term weight loss [34]. The difference might be explained by the clinical settings and length of the intervention. Specifically, our study used three months as the weight loss phase and one year as the weight maintenance phase, whereas Høie and Bruusgaard used two months as the weight loss phase and 15.2 months for long-term weight loss. Additionally, we used a low-calorie diet (800 kcals) coupled with physical activity as the intervention, which differed from their intervention of utilizing a very low-calorie diet (430 kcals per day).
Males were more likely to achieve short-term weight loss success in our population, but less likely to achieve long-term weight loss goals. Prior studies are conflicting. Similar findings to our own were reported by Sartorio et al [35]. Likewise, Kraschnewski et al. reported that females were more likely to achieve ≥ 10% IBWL at one year [28] Contrary to the aforementioned research, Ovbiosa-Akinbosoye and Long reported that males were more likely than females to lose weight in one year [36]. This difference may be due to different study settings. Ovbiosa-Akinbosoye and Long conductedtheir study in a comprehensive workplace wellness program setting, versus our physician-directed weight management clinic.
Finally, we identified that weight loss success at three months was a significant predictor for longer-term weight maintenance success. Similar findings have been documented by others [16-18,37]. Jeffery et al. concluded that adults who reached weight goals had better long-term weight maintenance than those who did not [16]. Additionally, a 24-month clinical trial concluded that the initial six-month reduction in weight (loss %) was the main predictor for long-term success in weight loss [17]. Other research has also documented that meeting early weight loss goal is one of the strongest predictors of long-term weight maintenance [18,38].
Limitations
This study is subject to several limitations. There was a high attrition rate at the end of one year; following phase 1 weight loss, 75% of adults dropped out of the phase 2 maintenance program prior to completing one year. Second, greater than 90% of the program’s population was Caucasian, and only 3.9% of the overall population was African American. This may limit the generalizability of our findings to other racial or ethnic groups. Additionally, due to the small proportion of African Americans, we were unable to assess the effect of race on the outcomes of interest.
Conclusion
In this study population, older adults (≥ 65 years) had decreased odds of achieving the short-term goal of losing ≥ 10% of their initial body weight compared to younger adults (18-44 and 45-64 years). Males were more likely to achieve short-term weight loss compared to females. However, at one year, the age effect diminished, and females were more likely to achieve the long-term goal of maintaining ≥ 10% of their initial body weight. All participants, especially older adults, should be encouraged to stay in the program to achieve the long-term weight maintenance success.
References
- World Health Organization. Prevention of diabetes mellitus.Report of a WHO Study Group. World Health Organization technical report series. 1994;844:1-100.
- Centers for Disease Control and Prevention. Obesity. 2013; www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201206_06.pdf. Accessed June 24, 2013.
- Anandacoomarasamy A, Caterson ID, Leibman S, Smith GS,Sambrook PN, Fransen M, March LM. Influence of BMI on health-related quality of life: comparison between an obese adult cohort and age-matched population norms. Obesity (Silver Spring, Md.). Nov 2009;17(11):2114-2118.
- Pan HJ, Cole BM, Geliebter A. The benefits of body weight loss on health-related quality of life. Journal of the Chinese Medical Association : JCMA. Apr 2011;74(4):169-175.
- Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. American journal of preventive medicine. Dec 2004;27(5):385-390.
- Nguyen T, Lau DC. The obesity epidemic and its impact on hypertension. The Canadian journal of cardiology. May 2012;28(3):326-333.
- Byers T, Sedjo RL. Does intentional weight loss reduce cancer risk? Diabetes Obes Metab. Dec 2011;13(12):1063-1072.
- Wearing SC, Hennig EM, Byrne NM, Steele JR, Hills AP. Musculoskeletal disorders associated with obesity: a biomechanical perspective. Obesity reviews : an official journal of the International Association for the Study of Obesity. Aug 2006;7(3):239-250.
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and servicespecific estimates. Health affairs (Project Hope). Sep-Oct 2009;28(5):w822-831.
- Finkelstein EA, Fiebelkorn IC, Wang G. State-level estimates of annual medical expenditures attributable to obesity. Obesity research. Jan 2004;12(1):18-24.
- Dall TM, Zhang Y, Zhang S, Arday DR, Sahai N, Dorn P,Jain A. Weight loss and lifetime medical expenditures: a case study with TRICARE prime beneficiaries. American journal of preventive medicine. Mar 2011;40(3):338-344.
- Dunkle-Blatter SE, St Jean MR, Whitehead C, Strodel W,3rd, Bennotti PN, Still C, Reed MJ, Wood CG, Petrick AT.Outcomes among elderly bariatric patients at a high-volume center. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. Mar-Apr 2007;3(2):163-169; discussion 169-170.
- Okay DM, Jackson PV, Marcinkiewicz M, Papino MN. Exercise and obesity. Primary care. Jun 2009;36(2):379-393.
- Anderson JW, Reynolds LR, Bush HM, Rinsky JL, Washnock C. Effect of a behavioral/nutritional intervention program on weight loss in obese adults: a randomized controlled trial. Postgraduate medicine. Sep 2011;123(5):205-213.
- Busetto L, Mazza M, Salvalaio S, De Stefano F, Marangon M, Calo E, Sampietro S, Enzi G. Obesity treatment in elderly outpatients: predictors of efficacy and drop-out. Eating and weight disorders : EWD. Jun-Sep 2009;14(2-3):e56-65.
- Jeffery RW, Wing RR, Mayer RR. Are smaller weight losses or more achievable weight loss goals better in the long term for obese patients? Journal of consulting and clinical psychology. Aug 1998;66(4):641-645.
- Greenberg I, Stampfer MJ, Schwarzfuchs D, Shai I. Adherence and success in long-term weight loss diets: the dietary intervention randomized controlled trial (DIRECT). Journal of the American College of Nutrition. Apr 2009;28(2):159-168.
- Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P.Weight loss by mobile phone: a 1-year effectiveness study.Public health nutrition. Dec 2009;12(12):2382-2391.
- Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obesity research. 1998;6(2):51S-209S.
- Wing RR, Hill JO. Successful weight loss maintenance. Annual review of nutrition. 2001;21:323-341.
- Jeffery RW, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill DR. Long-term maintenance of weight loss: current status. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. Jan 2000;19(1 Suppl):5-16.
- Gohner W, Schlatterer M, Seelig H, Frey I, Berg A, Fuchs R.Two-year follow-up of an interdisciplinary cognitive-behavioral intervention program for obese adults. The Journal of psychology. Jul-Aug 2012;146(4):371-391.
- Boehm G, Bracharz N, Schoberberger R. Evaluation of the sustainability of the Public Health Program “Slim without Diet (Schlank ohne Diat)”. Wiener klinische Wochenschrift. Jul 2011;123(13-14):415-421.
- Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. The Psychiatric clinics of North America. Dec 2011;34(4):841-859.
- Wing RR, Phelan S. Long-term weight loss maintenance. The American journal of clinical nutrition. Jul 2005;82(1Suppl):222S-225S.
- Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. The American journal of clinical nutrition. Nov 2001;74(5):579- 584.
- Lavery MA, Loewy JW, Kapadia AS, Nichaman MZ, Foreyt JP, Gee M. Long-term follow-up of weight status of subjects in a behavioral weight control program. Journal of the American Dietetic Association. Sep 1989;89(9):1259-1264.
- Kraschnewski JL, Boan J, Esposito J, Sherwood NE, Lehman EB, Kephart DK, Sciamanna CN. Long-term weight loss maintenance in the United States. International journal of obesity (2005). Nov 2010;34(11):1644-1654.
- Nicklas JM, Huskey KW, Davis RB, Wee CC. Successful weight loss among obese U.S. adults. American journal of preventive medicine. May 2012;42(5):481-485.
- Lloyd A, Khan R. Evaluation of Healthy Choices: a commercial weight loss programme commissioned by the NHS.Perspectives in public health. Jul 2011;131(4):177-183.
- Waters DL, Vawter R, Qualls C, Chode S, Armamento-Villareal R, Villareal DT. Long-term maintenance of weight loss after lifestyle intervention in frail, obese older adults. The journal of nutrition, health & aging. Jan 2013;17(1):3-7.
- Akers JD, Cornett RA, Savla JS, Davy KP, Davy BM. Daily self-monitoring of body weight, step count, fruit/vegetable intake, and water consumption: a feasible and effective long-term weight loss maintenance approach. Journal of the Academy of Nutrition and Dietetics. May 2012;112(5):685-692.e682.
- Milsom VA, Middleton KM, Perri MG. Successful long-term weight loss maintenance in a rural population. Clinical interventions in aging. 2011;6:303-309.
- Hoie LH, Bruusgaard D. Predictors of long-term weight reduction in obese patients after initial very-low-calorie diet.Advances in therapy. Nov-Dec 1999;16(6):285-289.
- Sartorio A, Maffiuletti NA, Agosti F, Lafortuna CL. Genderrelated changes in body composition, muscle strength and power output after a short-term multidisciplinary weight loss intervention in morbid obesity. Journal of endocrinological investigation. Jun 2005;28(6):494-501.
- Ovbiosa-Akinbosoye OE, Long DA. Factors associated with long-term weight loss and weight maintenance: analysis of a comprehensive workplace wellness program. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. Nov 2011;53(11):1236-1242.
- Postrach E, Aspalter R, Elbelt U, Koller M, Longin R, Schulzke JD, Valentini L. Determinants of successful weight loss after using a commercial web-based weight reduction program for six months: cohort study. Journal of medical Internet research. 2013;15(10):e219.
- Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, Horton ES, Hoskin MA, Kriska A, Lachin J, Mayer- Davis EJ, Pi-Sunyer X, Regensteiner JG, Venditti B, Wylie-Rosett J. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obesity research. Sep 2004;12(9):1426-1434.