Body Dysmorphic Disorder Secondary to Maxillofacial Traumatic Injuries: An Evaluative Analysis
Dr. Vaishali. V*, Dr. Alagappan M, Dr. P. Rajesh
Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Tamil Nadu, India.
*Corresponding Author
Dr.Vaishali. V, MDS,
Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai- 603103, Tamil Nadu, India.
Email: vaish712.venkat@gmail.com
Received: November 08, 2022; Accepted: March 10, 2023; Published: March 18, 2023
Citation: Dr. Vaishali. V, Dr. Alagappan M, Dr. P. Rajesh. Body Dysmorphic Disorder Secondary to Maxillofacial Traumatic Injuries: An Evaluative Analysis. Int J Surg Res. 2023;9(1):167-
170.
Copyright: Dr. Vaishali. V© 2023. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
While the management of traumatic maxillofacial injuries is focused in restoring physical form and function to normalcy, the
psychological morbidity that progresses silently during the recovery period remains undealt. BDD is one such disorder that
has never been studied in maxillofacial trauma survivors but highly impacting and thus needs to be taken seriously. This study
aims to evaluate the prevalence of Body Dysmorphic Disorder in patients surgically treated for traumatic maxillofacial injuries
during their postoperative recovery period.
Materials and Methods: A cross sectional analysis of patients surgically managed for the traumatic facial injuries were enrolled
between their sixth week and six months of recovery period. Age, gender, type of injury sustained (disfiguring or non-disfiguring)
were recorded. BDD-YBOCS scale was applied on them and responses were recorded and subjected to statistical analysis.
Results: The population was predominantly male. . 65.6% (n= 42) of them sustained disfiguring injuries. Prevalence of BDD
was observed in 23.4% (n=15). More than 93% of those found with BDD were with mean age of 24.8 and the association was
highly significant with p<0.000.
Discussion: BDD is commonly existent in post-traumatic patients and with simple tools can be diagnosed with ease. Psychological
well-being forms an integral part of a successful management of maxillofacial injuries.
2.Case Report
3.Discussion
4.References
Keywords
Psychological; Dysmorphophobia; Maxillofacial Trauma.
Introduction
Maxillofacial trauma has seen a surge in the 21st century and
considered the silent epidemic of the era. Though remarkable
progress in the surgical restoration of craniofacial fractures has
occurred, little attention has been paid to the emotional and psychological
distress that such trauma may cause [1]. Documentation
of psychological consequences like anxiety, depression, negative
socialization, Post traumatic stress disorder (PTSD) has been
done from the late 20th century. Assessment of quality of health
post trauma has been done by the psychologists but the role of
maxillofacial surgeons who share first line relation in the management
of the patient is negligible. Since face is crucial for establishing
a social relation, injury sustained in a trauma that hampers this
harmony impacts the individual’s life significantly. Body dysmorphic
disorder acquired post –trauma is a serious condition that has
to be noticed and addressed at the earliest. In dysmorphophobia
or body dysmorphic disorder, the patient has a subjective feeling
of ugliness or physical defect that he or she believes is noticeable
to others, although appearance is within normal limits [2]. This
study intends to evaluate the prevalence of BDD in post-surgical
patients treated for traumatic maxillofacial injuries and uncover
the latent psychological morbidity that proceeds chronically undermining
the patients’ quality of life.
Materials and Methods
An evaluative analysis of 64 patients who sustained maxillofacial
injuries due to trauma and were treated by the Department of
Oral and Maxillofacial Surgery during April 2019 to April 2020
was enrolled in the study. Patients, who were 16 years of age and
above, with surgical treatment (from suturing of lacerated wound
to surgical fixation of complex maxillofacial fractures) at least six
weeks to six months prior to their enrolment, were included in the
study. After obtaining ethical clearance, demographic details were
recorded. The injuries were recorded as disfiguring injuries in case
of significant post-traumatic change of facial orthopaedics or evident scarring and non- disfiguring injuries (no facial asymmetry or
scarring). Those with known psychological or neurologic conditions
were excluded in the study. After obtaining consent from the
subjects, Yale-Brown Obsessive Compulsive Scale, Modified for
BDD (BDD-YBOCS) was applied on them and their responses
were recorded. The BDD- YBOCS is a 12-item semi-structured
clinician-rated instrument to measure the severity of BDD in individuals
showing excessive pre-occupation and subjective distress
with physical appearance. They are rated on a 0-4 scale where
0 indicates no symptoms and 4 indicate extreme symptoms. It
measures the severity of BDD-related obsessions, compulsions,
and avoidance and hence was selected to assess the post-traumatic
incidence of BDD in maxillofacial trauma patients. Total score
varies from 0 to 48 and a score higher than 20 denotes the presence
of BDD in the subject. All the data was recorded and subjected
to statistical analysis.
Statistical Analysis
The collected data were analysed with IBM.SPSS statistics software
23.0 Version. To describe about the data, descriptive statistics,
frequency analysis, percentage analysis were used for categorical
variables and the mean & S.D were used for continuous
variables. To find the significant difference between the bivariate
samples in Independent groups the Unpaired sample t-test was
used. For the multivariate analysis the one way ANOVA was used.
To find the significance in categorical data Chi-Square test was
used. Similarly if the expected cell frequency is less than 5 in 2×2
tables, the Fisher's exact test was used. In all the above statistical
tools the probability value .05 is considered as significant level.
Result
Out of the 64 subjects, 71.9% (n= 46) were males and 28.1%
(n=18) were females. 65.6% (n= 42) of them sustained disfiguring
injuries of the face while 34.4% (n= 22) sustained non disfiguring
injuries. Prevalence of BDD was observed in 23.4% (n=15)
of the study population with total score greater than 20 and absent
in 76.6% (n= 49). Highest total score recorded was 31 and
the lowest 0. Mean BDD score of the population was 16.30. No
significant association of BDD with gender was observed in our
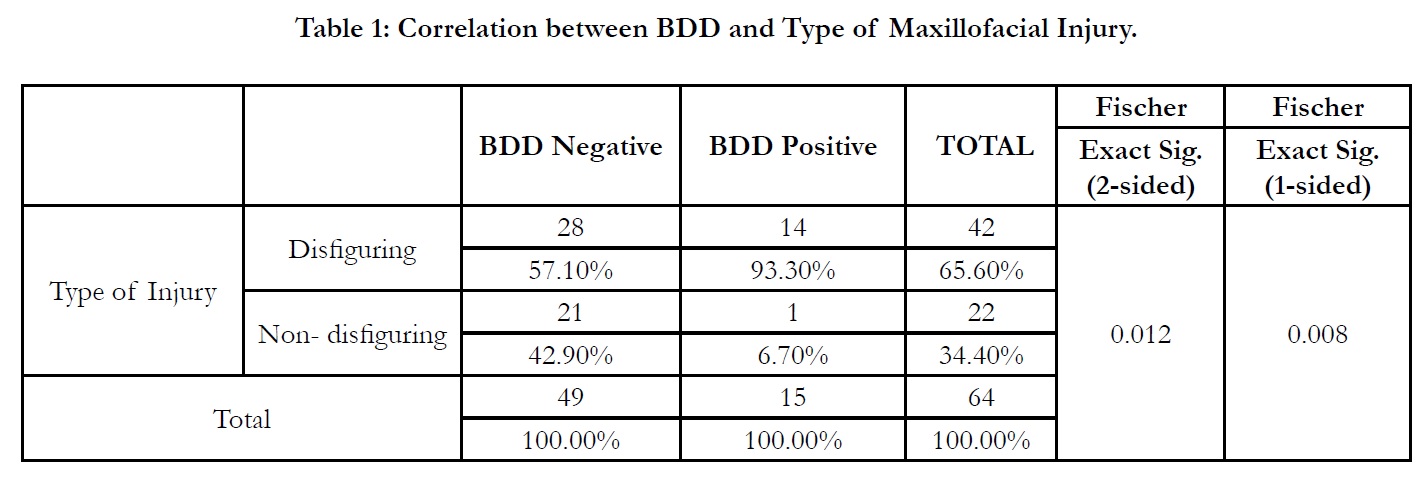
study. Table 1 presents the correlation of BDD with the type of
sustained maxillofacial injuries. 93.3% (n=14) of those with BDD
had sustained disfiguring injuries to the face while 6.7% (n=1) had
no disfiguring injury to the face but was found to have BDD. The
association between the type of maxillofacial injury and incidence
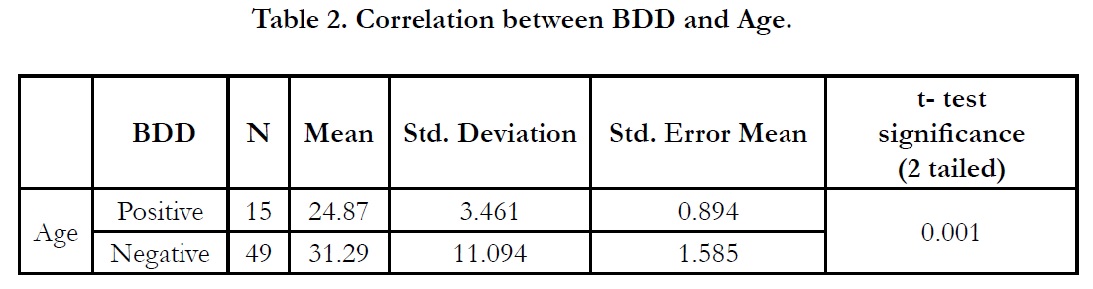
of BDD was statistically significant with p<0.05. Table 2 depicts
the correlation of age and the incidence of BDD. The mean age
of the population positive for BDD was 24.8 ± 3.4 and the association
of BDD bore a high statistical significance with p<0.000.
Discussion
Maxillofacial trauma comprises the major concern of modern day
medicine and public services due to increasing global urbanization.
Due to the complexity and fragility of the anatomical architecture,
the vulnerability of sustaining high impact forces by facial
skeleton is not so uncommon. Road traffic accidents, interpersonal
violence, fall, sport injuries are the most common reasons
of maxillofacial trauma and, significant morbidity and mortality
is associated with the same. The severity of maxillofacial injuries
varies from mild soft tissue injuries like contusion, lacerations or
abrasions to complex fractures of the craniofacial skeleton which
requires respective management protocols. Prompt diagnosis of
the severity of the sustained injury in the emergency department
and early surgical management of the complex injuries reduces
morbidity to a significant extent. Generally, the stability of the facial
construct and reinstating the functional abilities are the prime
objectives of treatment planning, restoration of facial esthetics
is the third pillar of a successful management of maxillofacial
injuries. While the stability and functional aspects of management
greatly influences the restoration of physical form, esthetic restoration
has significant effect on psychological well-being of the
individual in addition to the physical form. Examination of the
mental health of a patient post-trauma is rarely ever recorded and
failure to do so affects the quality of life of the individual thereafter
[3]. Face is vital in recognizing oneself socially and unfamiliar
change in their face as a result of trauma causes grave psychological morbidity [4]. Bisson JI et al reported that 26-41% of those
sustaining maxillofacial injuries suffer from psychological illness
post-treatment ranging from anxiety, depression to Post-traumatic
stress disorder (PTSD)[5]. The importance of identifying and
addressing these consequences are being studied upon by various
researchers recently. In addition to these conditions, there is another
unidentified mental morbidity that is commonly prevalent
in the victims of facial traumatic injuries is the Body Dysmorphic
Disorder (BDD). Maxillofacial injury causes both objective and
subjective changes in facial appearance. Individuals with facial
disfigurement tend to have a negative social imaging and a lower
self-esteem in view of the acquired facial defect [6]. This study intended
to identify such an unexplored yet important psychological
concern uniquely associated with maxillofacial trauma.
Body Dysmorphic Disorder, according to Diagnostic and Statistical
Manual of mental disorders-V (DSM-V)[7] criteria is characterized
to be “preoccupation with one or more perceived defects
or flaws in physical appearance that are not observable or appear
slight to others,” and by “repetitive behaviors (e.g., mirror checking,
excessive grooming, skin picking, reassurance seeking) or
mental acts (e.g., comparing his or her appearance with that of
others) in response to the appearance concerns.” In addition, it
causes “clinically significant distress or impairment in important
areas of functioning” and its “symptoms are not better explained
by normal concerns with physical appearance or by concerns with
body fat or weight in individuals meeting diagnostic criteria for eating
disorders.” Generally patients seek medical treatment and they
still remain dissatisfied after treatment. In maxillofacial patient
population, BDD is most commonly observed in patients with
developmental jaw deformities requiring orthognathic surgeries
or perceived defect of the soft tissues requiring aesthetic plastic
surgeries [8]. Prevalence of BDD in post-traumatic acquired deformities
of face when traced had little literature evidence and
has not been studied previously. Most of it goes unrecognized by
the surgeon and also the patient who is unaware of developing
dissatisfaction of the facial defect with time. The more the BDD
is unaddressed, the more impact it has on the social and personal
life of the individual. It also repels the individual from the common
activities due to increasing severity of preconceived notion
regarding their post-traumatic disfigurement chronically affecting
their lives. The diagnosis of BDD can be done with simple tools
like questionnaires during the post-surgical period. Tools that are
commonly employed for diagnosing BDD [9] are Yale-Brown
Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder
(BDD-YBOCS), Structured Clinical Interview for DSM-IV
Axis I Disorders, Non-Patient Edition (SCID-NP), CGI-I Scale,
Body Dysmorphic Disorder Examination (BDDE), Modified
Hamilton Depression Rating Scale (HAM-D), Brown Assessment
of Beliefs Scale (BABS), The Cosmetic Procedure Screening Scale
(COPS), The Appearance Anxiety Inventory (AAI), and the BDD
Dimensional Scale.
BDD- YBOCS is semi-structured 12 item clinician rated scale
that assess the severity of BDD in the past week. Since BDD
share similar symptoms with Obsessive Compulsive Disorder,
this scale was re-adapted in diagnosing BDD. The first five items
assess obsessional preoccupations of the perceived appearance
defects (time preoccupied, interference in functioning and distress
due to perceived appearance defects, resistance against preoccupations,
and control over preoccupations). Items 6–10 assess
BDD-related repetitive behaviours (e.g., excessive grooming, mirror
checking) and are similar to items 1–5 (time spent performing
the behaviours, interference in functioning due to the behaviours,
distress experienced if the behaviours are prevented, and resistance
of and control over the behaviours). Item 11 assesses insight
into appearance beliefs (e.g., “I am ugly”), and item 12 assesses
avoidance (e.g., of work/school or social activities) because of
BDD symptoms. Scores for each item range from 0 (no symptoms)
to 4 (extreme symptoms); the total score ranges from 0
to 48, with higher scores reflecting more severe symptoms [10].
Minimum score of 20 is required to confirm the patient to be
positive for BDD [11].
This study results revealed that a considerable proportion of the
patients were found to have developed BDD during their postoperative
recovery period. Out of 64 patients enrolled, BDD was
incident in 23.4% of the patients. BDD in general population has
a prevalence rate of 0.7 to 4%. While in patients seeking cosmetic
surgery and dermatology it is around 6 to 16%. About 10% of
those seeking esthetic jaw correction surgeries were reported to
have BDD. Avinash De Souza [12] reported that prevalence of
psychological comorbidity in patients undergoing reconstructive
surgeries post-tumor resection is comparatively lower than patients
sustained traumatic facial injuries. Trauma induced defects
are often considered to be unnecessary, random and unacceptable
that escalates anger and hatred towards oneself and the situation
that could have been avoided by chance as well as idealizing
one’s pre-injury physical appearance making the adjustment process
more difficult. This supports the results of our study. Also,
the rate of incidence of BDD was higher in patients sustaining
disfiguring injuries of the face comprising about 93.3% of the
total positive BDD patients which was statistically significant.
Also another important finding in our study was, those who were
diagnosed with presence of BDD were young adults with mean
age of 24.8 years and the result was highly significant statistically.
This depicts the dire need to address the psychological impact
of trauma during the recovery period. Failing to do so proves to
be detrimental to the rest of the productive years of these young
adults. 20- 30 years being the formative years of an individual
is loaded with vision and responsibility, self-esteem, confidence
and prime importance to the esthetic outlook of the individual.
When a traumatic event causes facial defect, it impacts social image
of the patient. Patients feel inferior due to the stigma around
the facial appearance and tend to exhibit social withdrawal and
isolation. The prolonged recovery, multiple hospital visits, rehabilitation
methods adds up to the mental exhaustion [12]. When
prompt diagnosis is not made, this can progress chronically stagnating
the progress of the individual and coping with the distress
becomes an uphill task. The psychological needs of a individuals
with post- traumatic facial injuries are unique and are more likely
to report symptoms of depression, anxiety, and hostility when
compared to a matched normal control group for a period of up
to 1 year post trauma [13]. In many cases due to the sub-threshold
prevalence of BDD, a diagnostic dilemma prevails and prevents
from being spot. Thus it is imperative to watch out for the psychological
well-being of the patients during the post-surgical recovery
period. A comprehensive approach has to be made by the
surgeon in managing the patient physically and psychologically.
Lack of understanding of the psychological aspect of the patients
can be attributed to no exposure to psychology as a subject resulting
in low awareness [14]. With simple tools that are enormously
available and easy to apply, could identify the prevalence and severity
of the condition, it should be adapted as a part of the post operative protocol and follow an interdisciplinary management of
the patient for a complete success.
This study has few shortcomings. A larger sample size would have
substantiated the importance of the prevalence of BDD. This
study was done cross-sectionally due to the reduced compliance
of the patients of the region and multiple visits and follow up of
the same could validate the course of the disorder over time. The
sample population was predominantly male and a higher size of
sample would alleviate the doubts entailing the same.
Conclusion
This study exposes that BDD is commonly prevalent in patients
with acquired facial defects due to traumatic injuries and has to
be checked for in every patient during follow up. Adequate psychological
support should be provided to the patients to recover
mentally that will hasten up the process of physical well-being.
Young adults are more prone to develop BDD and are often unaware
of it progressing chronically. Hence a multidisciplinary approach
should be formulated during the treatment of maxillofacial
trauma patients and adequate follow up of the patient should
be done to improve the overall recovery of the patient.
References
- Roccia F, Dell'Acqua A, Angelini G, Berrone S. Maxillofacial trauma and psychiatric sequelae: post-traumatic stress disorder. J Craniofac Surg. 2005 May;16(3):355-60. PubMed PMID: 15915097.
- Thomas CS, Goldberg DP. Appearance, body image and distress in facial dysmorphophobia.ActaPsychiatr Scand. 1995 Sep;92(3):231-6. PubMed PMID: 7484204.
- De Sousa A. Psychological issues in acquired facial trauma. Indian J Plast Surg. 2010 Jul;43(2):200-5. PubMed PMID: 21217982.
- Cunningham SJ. The psychology of facial appearance. Dent Update. 1999 Dec;26(10):438-43. PubMed PMID: 10765787.
- Prashanth NT, Raghuveer HP, Kumar RD, Shobha ES, Rangan V, Hullale B. Post-traumatic Stress Disorder in Facial Injuries: A Comparative Study. J Contemp Dent Pract. 2015 Feb 1;16(2):118-25. PubMed PMID: 25906802.
- Sahni V. Psychological Impact of Facial Trauma.Craniomaxillofac Trauma Reconstr. 2018 Mar;11(1):15-20. PubMed PMID: 29387299.
- de Brito MJ, SabinoNeto M, de Oliveira MF, Cordás TA, Duarte LS, Rosella MF, et al. Yale-Brown Obsessive Compulsive Scale modified for Body Dysmorphic Disorder (BDD-YBOCS): Brazilian Portuguese translation, cultural adaptation and validation. Braz J Psychiatry. 2015 Oct-Dec;37(4):310-6. PubMed PMID: 26692429.
- Collins B, Gonzalez D, Gaudilliere DK, Shrestha P, Girod S. Body dysmorphic disorder and psychological distress in orthognathic surgery patients. J Oral Maxillofac Surg. 2014 Aug;72(8):1553-8. PubMed PMID: 24582136.
- Thanveer F, Khunger N. Screening for Body Dysmorphic Disorder in a Dermatology Outpatient Setting at a Tertiary Care Centre. J CutanAesthet Surg. 2016 Jul-Sep;9(3):188-191. PubMed PMID: 27761090.
- Phillips KA, McElroy SL, Dwight MM, Eisen JL, Rasmussen SA. Delusionality and response to open-label fluvoxamine in body dysmorphic disorder.J Clin Psychiatry. 2001 Feb;62(2):87-91. PubMed PMID: 11247107.
- Brito MJ, Nahas FX, Cordás TA, Gama MG, Sucupira ER, Ramos TD, et al. Prevalence of Body Dysmorphic Disorder Symptoms and Body Weight Concerns in Patients Seeking Abdominoplasty. AesthetSurg J. 2016 Mar;36(3):324-32. PubMed PMID: 26851144.
- Phillips KA. An open-label study of escitalopram in body dysmorphic disorder.IntClinPsychopharmacol. 2006 May;21(3):177-9. PubMed PMID: 16528140.
- Wilson N, Heke S, Holmes S, Dain V, Priebe S, Bridle C, et al. Prevalence and predictive factors of psychological morbidity following facial injury: a prospective study of patients attending a maxillofacial outpatient clinic within a major UK city. Dialogues ClinNeurosci. 2018 Dec;20(4):327-339. PubMed PMID: 30936771.
- Krishnan B, Rajkumar RP. Psychological Consequences of Maxillofacial Trauma in the Indian Population: A Preliminary Study. Craniomaxillofac Trauma Reconstr. 2018 Sep;11(3):199-204. PubMed PMID: 30087749.