Does the Facial Construct Protect the Brain from the Impact of Traumatic Injuries? A Retrospective Study
Dr. Rajesh. P1, Dr. Vaishali. V2*
1 Professor and Head, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai, India.
2 Post Graduate, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai, India.
*Corresponding Author
Dr. Vaishali. V, BDS,
Department of Oral and Maxillofacial surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai- 603103, India.
Tel: 8056379290, 8838017051
Email: vaish712.venkat@gmail.com
Received: January 02, 2022; Accepted: February 08, 2022; Published: February 09, 2022
Citation: Dr. Rajesh. P, Dr. Vaishali. V. Does the Facial Construct Protect the Brain from the Impact of Traumatic Injuries? A Retrospective Study. Int J Surg Res. 2022;8(2):156-160. doi: dx.doi.org/10.19070/2379-156X-2200034
Copyright: Dr. Vaishali. V© 2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To evaluate the prevalence and association of traumatic brain injuries in patients sustaining maxillofacial trauma, and
correlate with the proposed role of the facial skeleton to protect the brain.
Background: Maxillofacial skeletal architecture has been considered to sustain the impact during trauma and protect the brain
from injury. Whether or not, this has an important clinical implication as it will help the surgeon to assess and rule out during
the preliminary evaluation thereby reducing the risk of potential delayed complications.
Materials: A retrospective analysis of trauma patients reported to the emergency department of a tertiary care center in Tamil
Nadu during March 2015- March 2020 was done. A detailed review of the maxillofacial trauma cases was done. Details related
to the demography, trauma, injury sustained, primary and secondary survey, records pertaining to the diagnosis of traumatic
brain injuries, their pattern, severity, and spectrum were studied, recorded, and subjected to statistical analysis.
Results: 888 out of 6350 patients sustained maxillofacial injuries. The Mean age was 31.4 years and the population was predominantly
male. 61% sustained soft tissue injuries. Among the hard tissue injuries, mandibular fractures were highest followed
by isolated zygomaticomaxillary complex fractures. 42.4% sustained TBI of which concussion was predominant followed by
diffuse axonal injury, contusion, hemorrhage, and skull fractures. A significant association was found between the incidence of
TBI and various types of maxillofacial injuries.
Conclusion: The incidence of TBI is strongly associated with maxillofacial injuries. Thus traumatic maxillofacial injuries can
be used as predictors of the TBI.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Maxillofacial Trauma; Head Injury; Brain Injury; Oral Surgery.
Introduction
Maxillofacial injuries are conventionally approached as an isolated
entity in the emergency department. Proximity and complexity of
the maxillofacial architecture always bear a risk of concomitant
injury to the cranium during trauma and incidence rates as high as
86% have been reported in the literature [1]. But the construct of
the facial bones has always been considered to protect the brain
from the impact of these traumatic injuries. Data pertaining to
the protective role of facial bones are contradicting and scant.
Knowledge about the association and incidence of traumatic
brain injuries (TBI) coexisting with the maxillofacial injuries is
very important, as concurrent evaluation for evidence of a closedhead
injury may be overlooked or relegated to obscurity following
a patient's initial evaluation [2]. The maxillofacial surgeon must
be aware of the consequences associated with it and its management.
This study aims to determine the association between the
incidence, pattern, and frequency of TBI in patients sustaining
maxillofacial traumatic injuries and its clinical implications.
Methodology
A retrospective Unicenter analysis was done on a total of 6350
trauma cases reported to the emergency department of our institution
from March 2015 to March 2020. Out of the 6350 cases,
a detailed analysis of 888 patients sustaining maxillofacial injuries
was done. Clinical and radiographic data pertaining to the
age, gender, mechanism of injury, type of maxillofacial injury
sustained, frequency and type of facial fracture, the incidence of
traumatic brain injury, and pattern and severity of the brain injury were obtained. The type of maxillofacial injury was recorded as
soft tissue injury and hard tissue injury. Types of facial fracture
were divided into isolated mandibular, isolated maxillary that included
Lefort type I, type II, type III, isolated zygomaticomaxillary,
combined fractures of the mandible and middle third of the
face which included fractures of the mandible and maxilla, mandible
and zygomaticomaxillary complex, and mandible and naso-
orbito-ethmoidal region and finally pan facial fractures which
involved more than three bony components. Traumatic brain injuries
were identified based on the diagnosis and evaluation done
by the Department of Neurosurgery of our hospital. Types of
traumatic brain injuries included concussion, contusion, focal injuries
like epidural, subdural and intracranial haemorrhages, and
diffuse injuries like axonal injuries and subarachnoid haemorrhages.
The Presence of skull fractures was also recorded. Severity
was graded based on the Glasgow Coma Scale as Mild (GCS
13-15), Moderate (9-12), and severe (less than 9) and the loss of
consciousness, Mild(less than 30 minutes), Moderate (30 minutes
to 24 hours) and Severe (more than 24 hours). All the cases with
complete medical records were included in the study. A deficit of
information or intervention due to reasons other than traumatic
brain injuries were excluded from the study. All the details were
recorded and subjected to statistical analysis.
Statistical analysis
The collected data were analyzed with IBM.SPSS statistics software
23.0 Version. To describe the data descriptive statistics frequency
analysis, percentage analysis was used for categorical variables.
Chi-square test was applied and Pearson's correlation was
used to find significance between the variables. In all the above
statistical tools the probability value .05 is considered as significant
level.
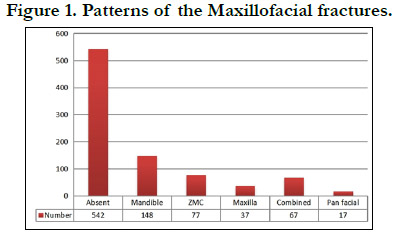
Results
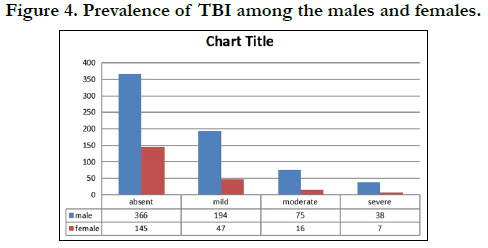
There were 888 patients with maxillofacial injuries out of 6350
reported trauma cases. Of these 888 patients, 683 were males
and 215 were females. About 529(59.6%) of the study population
belonged to the age group of 20-39 years, while 194 (21.5%)
were between 40-60 years, (134)15.1% were less than 20 years and
31(3.5%) above 60 years. 545(61.4%) of them sustained soft tissue
maxillofacial injuries and 343 (38.6%) hard tissue injuries. Out
of these 343 hard-tissue injuries, 148(16.7%) sustained mandibular
fractures, 77(8.7%) zygomatico-maxillary complex fractures,
67(7.5%) combined fracture of mandibular and middle third of
the face, 37(4.2%) maxillary, and finally 17(1.9%) with pan facial
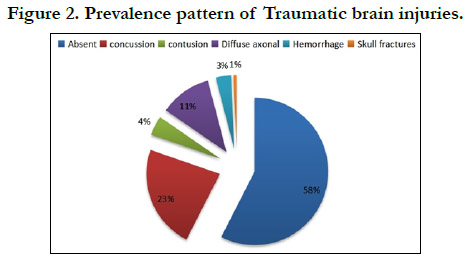
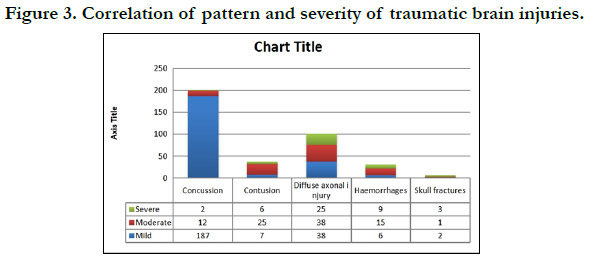
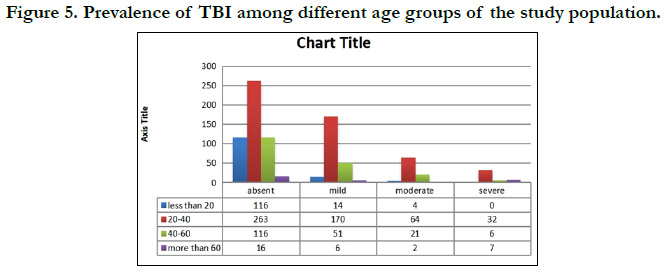
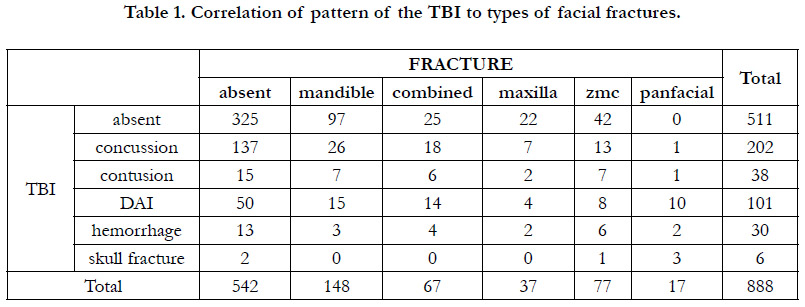
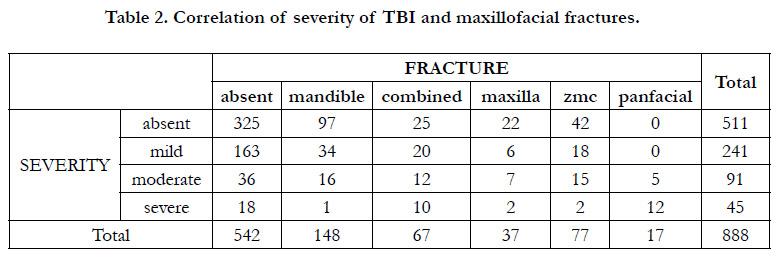
fractures (Figure 1). Patterns of traumatic brain injury observed,
is depicted in Figure 2. 42.45% (n= 377) sustained traumatic brain
injuries of which the highest prevalence was concussion (n= 202),
followed by Diffuse axonal injuries (n= 101), contusion (n=38),
haemorrhage (n= 30) and skull fractures (n=6). Of the 377 patients
injuries incurred by 27% (n= 241) were mild, 10.2% (n=91)
moderate and 5.1% (n=45) severe. Figure 3 shows the association
of the pattern and severity of brain injuries. Concussion and diffuse
axonal injuries constituted for than 90% of the mild injuries
while variations in the pattern were observed with moderate and
severe injuries. Of 343 patients with maxillofacial fractures, 46%
(n= 158) of them sustained traumatic brain injuries of which
concussion was found predominant (n=63, 18.3%), followed by
diffuse axonal injury (n=51, 14.8%), contusion (n=23, 6.7%),
haemorrhage (n=17, 4.9%) and skull fractures (n= 4, 1.1%). Interestingly,
patients who sustained soft tissue maxillofacial injuries
have a significant prevalence of traumatic brain injuries. Of
545 patients, 40% sustained TBI with 25% being concussion (n=
202), 9% with diffuse axonal injuries (n= 50), 2.7% with contusion
(n= 23) and 2.3% with haemorrhages (n=13). Table 1 depicts
the correlation of the pattern of TBI with the type of facial fractures. Correlation of severity of TBI with different types of
facial injuries is given in Table 2. Correlation of the prevalence of
traumatic brain injuries with age and gender has been presented
in Figure 4 and Figure 5 respectively.
Discussion
Maxillofacial traumatic injuries form a significant proportion of
the entire trauma due to the exposure of the region and vulnerability
to injury. The severity of injury varies from a mild injury to the soft tissues to life-threatening injuries to the facial skeleton
and often requires emergency evaluation. The Maxillofacial surgeon
being a part of the trauma team, conventionally approaches
the injuries as an isolated entity, and the concomitant injuries incurred
are not dealt with. A missed or delayed diagnosis of such
co-existing injuries of the other systems might bloom out a fatal
catastrophe. The injuries associated vary depending on the nature
of impact but most commonly observed are the traumatic brain
injuries and cervical spine injuries. Davidoff et al [2] defined traumatic
brain injury as evidence of loss of consciousness and/ or
post-traumatic amnesia in a patient with a non-penetrating head
injury and reported a strong association with maxillofacial injuries
post-trauma.
In the literature, there have always been contradicting claims of
the protective role of the facial architecture to the brain and the
intricate, complex anatomy of the facial skeleton has been extensively
studied to infer it. Several authors suggested that the
facial skeleton absorbs the impact of traumatic forces and provides
a cushioning effect thereby preventing damage to the brain.
Whether or not, the association of both the injuries coexisting
has its clinical implications and this study intends to figure out the
same. Recent evidence supports that the closeness and fragility
of the maxillofacial bones to the cranium increases the risk of
intracranial injuries as forces with sufficient energy will be transferred
directly to the neurocranium. A highly varying incidence
rate of TBI in maxillofacial trauma has been reported. While Lim
et al posed a lower incidence rate of 5.4%, Martin et al and Hayer
et al proposed a rate of 79.4% and 86.4% respectively [3]. In our
study, 42.4% of the total 888 maxillofacial trauma patients had
associated TBI, while 46% of patients with fractures of the facial
skeleton and 40% of those with soft tissue injuries of the face had
TBI. Only very few studies evaluated the incidence of TBI in soft
tissue injuries and Zandi et al reported an incidence rate of 13%
in their study. This alarms the maxillofacial surgeon encountering
the trauma patient first hand to consider any type of maxillofacial
injury to also have sustained a TBI. Also, it highlights that the
absence of maxillofacial fracture doesn’t guarantee the absence
of cranial injuries in patients sustaining trauma to the head and
neck [4]. The spectrum of TBI patterns observed in our study,
from the highest to the lowest rate of incidence is concussion
accounting for 22.7% followed by diffuse axonal injury (11.4%),
contusion injuries (4.3%), focal haemorrhages (3.4%) and finally
skull fractures (0.7%). This is similar to the results of the study of
Joshi et al, Pappachan et al, Keenan et al who reported the highest
incidence of concussion with incidence rates 38%, 47%, 9%
respectively. Contrasting results were found in one of the studies
with the largest sample size of about 1.3 billion by Mulligan et al
where skull fractures were predominant (29.5%), and intracranial
haemorrhages (28.6%) [5].
Clinically TBI is classified based on the Glasgow Coma Scale into
mild (15-13), moderate (12-9), and severe (8-3). In our study 27%
sustained mild TBI, 10.2% with moderate injuries, and 5.1% with
severe injuries which is in accordance with the results of Arslan
et al [6]. In our study concussion constituted 77.2% of the mild
injuries followed by diffuse axonal injuries (15.7%), contusion
(2.8%), and focal haemorrhages (2.4%). In moderate injuries diffuse
axonal injuries were predominant with 41.7%, followed by
contusion with 27.4%, haemorrhages with 16.4%, and concussion
with 13.1%. In severe TBI, diffuse axonal injuries constituted
55.5%, while intracranial haemorrhages were found in 20% and
contusion in 13.3%. The concussion was predominantly found in
patients with mild TBI while diffuse axonal injury and contusion
occurred in higher rates in moderate and severe injuries. This variation
can be attributed to the magnitude and impact of traumatic
forces and the mechanism of trauma since patients with soft tissue
injuries are more likely to have sustained milder forms of TBI
when compared to those who endured fractures of the facial skeleton.
Rajandram et al reported similar results with 18.6% of mild
TBI were observed in patients without maxillofacial fractures [7].
Also, this could be the reason for varying results of TBI patterns
in the study of Mulligan et al as patients with maxillofacial fractures
were their chief study population.
A Significant association of the maxillofacial fractures and the
TBI was observed in the results of our study. 48% of 343 patients
with maxillofacial fractures sustained isolated mandibular
fractures of which 34.4% had concussion, 10% had diffuse axonal
injuries, 4.7% contusion, 2% haemorrhages. Isolated maxillary
fractures accounted for 10.7% out of which 40% sustained TBI.
Isolated zygomatico maxillary fracture was identified in 22.4% of
which 45.4% sustained TBI. Combined fracture of the mandible
and middle third of the face was found in 19.5% out of which
62.6% had TBI. 4.9% of the maxillofacial fractures were pan
facial and high statistical significance (p<0.0005) was found in
their association with the TBI. 100% of the lot sustained TBI in
a diverse spectrum with diffuse axonal injuries being the highest
(58.8%) followed by 17.6% with skull fractures and 11.7% with
focal haemorrhages. Similar results on the incidence of the patterns
of TBI was reported by Joshi et al, Lee et al, and Isik et
al, and they concluded that a positive correlation exists between
the complexity of the maxillofacial fractures and incidence of
TBI [8]. On correlating the severity of TBI to types of maxillofacial
fractures, a positive correlation existed between both. Mild
TBI was found in 22% of mandibular fractures, 16.2% of isolated
maxillary fractures, 23.3% of zygomaticomaxillary complex
fractures, and 29.8% of the combined fractures of the mandible
and mid-third of the face. Moderate injuries were predominant
in pan facial fractures with a proportion of 29.4% followed by
19.4% of zygomaticomaxillary fractures, 18.9% of isolated maxillary
fractures, 17.9% of combined fractures of the mandible and
mid-third of the face, and finally 10.8% of the isolated mandibular
fractures. Severe TBI was observed the highest in pan facial
fractures with 70.5% followed by the combined mandibular and
mid-third of face fractures with 14.9%, isolated maxillary fractures
with 5.4%, and 2.5% of the zygomatico maxillary fractures.
Keenan et al disproved the protective role of facial architecture
[9] and proposed that the risk of TBI increases almost ten-fold in
maxillofacial injuries and the risk of concussion in those doubled.
Several authors emphasized the association of the middle third of
the face fractures to the incidence of traumatic brain injuries even
though mandibular fractures were the highest to be observed
which is similar to the results of our study [11].
With the escalating complexity of maxillofacial fractures, the severity
of the TBI also rises depicting that maxillofacial injuries
can be regarded as significant indicators of coexisting traumatic
brain injuries.
Thus this study implies the fact that maxillofacial injuries don't
prevent damage to the brain while it only potentiates it and should
be definitely considered a marker during the preliminary evaluation. Especially a significant proportion of the study population
without maxillofacial fractures sustained TBI. This group of patients
is most likely to be missed in the emergency department
and are treated for soft tissue injuries and discharged home. They
are at a higher risk due to unexpected exacerbations of the undiagnosed
TBI that might fatally flare-up on rare occasions, like
the second impact syndrome [12]. Injuries of high morbidity and
mortality rates which requires thorough evaluation during the
time of presentation. A high index of suspicion should be exhibited
by the maxillofacial surgeon while treating the patient with
traumatic facial injuries. There are a few shortcomings of this
study. Retrospective designed information bias especially patients
without follow up records. More exhaustive multicentric research
with added parameters can enlighten the contradicting theories
on the spectrum of TBI and its incidence and association with
maxillofacial injuries which paves way for identification of unsuspected,
latent cranial injuries.
Conclusion
Facial injuries can be contemplated to be markers of cranial injuries
after trauma and it is expected of every surgeon attending
to meticulously examine and rule out the traumatic injuries
incurred by the brain before it turns out to be a catastrophe. An
interdisciplinary and comprehensive management model should
be followed for directed care of the patient rather than the isolated
approach.
References
- Zandi M, Seyed Hoseini SR. The relationship between head injury and facial trauma: a case–control study. Oral Maxillofac Surg. 2013 Sep;17(3):201-7.
- Davidoff G, Jakubowski M, Thomas D, Alpert M. The spectrum of closedhead injuries in facial trauma victims: incidence and impact. Ann Emerg Med. 1988 Jan;17(1):6-9.Pubmed PMID: 3337417.
- Salentijn EG, Peerdeman SM, Boffano P, van den Bergh B, Forouzanfar T. A ten-year analysis of the traumatic maxillofacial and brain injury patient in Amsterdam: incidence and aetiology. J Craniomaxillofac Surg. 2014 Sep;42(6):705-10.Pubmed PMID: 24703508.
- Joshi UM, Ramdurg S, Saikar S, Patil S, Shah K. Brain injuries and facial fractures: A prospective study of incidence of head injury associated with maxillofacial trauma. J Maxillofac Oral Surg. 2018 Dec;17(4):531-7.
- Mulligan RP, Friedman JA, Mahabir RC. A nationwide review of the associations among cervical spine injuries, head injuries, and facial fractures. J Trauma. 2010 Mar;68(3):587-92.Pubmed PMID: 19996802.
- Arslan ED, Solakoglu AG, Komut E, Kavalci C, Yilmaz F, Karakilic E, et al. Assessment of maxillofacial trauma in emergency department. World J Emerg Surg. 2014 Dec;9(1):13.
- Rajandram RK, Syed Omar SN, Rashdi MF, Abdul Jabar MN. Maxillofacial injuries and traumatic brain injury--a pilot study. Dent Traumatol. 2014 Apr;30(2):128-32.Pubmed PMID: 23782407.
- Lee KF, Wagner LK, Lee YE, Suh JH, Lee SR. The impact-absorbing effects of facial fractures in closed-head injuries. An analysis of 210 patients. J Neurosurg. 1987 Apr;66(4):542-7.Pubmed PMID: 3559719.
- Keenan HT, Brundage SI, Thompson DC, Maier RV, Rivara FP. Does the face protect the brain? A case-control study of traumatic brain injury and facial fractures. Arch Surg. 1999 Jan;134(1):14-7.Pubmed PMID: 9927123.
- Lim LH, Lam LK, Moore MH, Trott JA, David DJ. Associated injuries in facial fractures: review of 839 patients. Br J Plast Surg. 1993 Dec;46(8):635- 8.Pubmed PMID: 8298773.
- Haug RH, Savage JD, Likavec MJ, Conforti PJ. A review of 100 closed head injuries associated with facial fractures. J Oral Maxillofac Surg. 1992 Mar;50(3):218-22.Pubmed PMID: 1542064.
- Pappachan B, Alexander M. Correlating facial fractures and cranial injuries. J Oral Maxillofac Surg. 2006 Jul 1;64(7):1023-9.
- Hackl W, Hausberger K, Sailer R, Ulmer H, Gassner R. Prevalence of cervical spine injuries in patients with facial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Oct 1;92(4):370-6.