Mealtime Syndrome: Submandibular gland sialolithiasis. A Case Series
Rajwant Kaur Kamal*
Department of Otorhinolaryngology, Government Medical College and Hospital, Patiala, Punjab, India.
*Corresponding Author
Rajwant Kaur Kamal,
Department of Otorhinolaryngology, Government Medical College and Hospital, Patiala, Punjab, India.
Tel: 9501200943
Email: rajwin000@gmail.com
Received: May 02, 2020; Accepted: May 26, 2020; Published: May 30, 2020
Citation: Rajwant Kaur Kamal. Mealtime Syndrome: Submandibular gland sialolithiasis. A Case Series. Int J Surg Res. 2020;7(3):149-151. doi: dx.doi.org/10.19070/2379-156X-2000032
Copyright: Rajwant Kaur Kamal© 2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Submandibular Gland; Sialoliths; Sailendoscopy; Othopantogram.
Introduction
Salivary stone or sialoliths are most common disease of salivary gland. Submandibular gland and its duct constitute 80-95 % of the salivary stone, about 5-20% occur in the parotid gland and only 1-2% in the sublingual gland and the rest seen in the minor salivary gland [1]. The submandibular stone is most frequently involved because of its anatomic location, long tortuous duct with a narrow orifice compared to the main portion of the duct [2]. Submandibular stones constitutes 82% inorganic and 18% organic material whereas parotid stone 49 % inorganic and 51% organic material [3].
Salivary stone are usually less than 1 cm but giant stone also been reported. Stone usually grow by deposition at an estimated rate of 1mm to 1.5 mm per year [4]. Stone can be round or irregular in shape and size varies from 2 mm to 3.2 mm for parotid and 2mm to 4.9 mm for submandibular gland [5].
Sialoliths may be asymptomatic, or may presents with painless swelling but when duct obstructed patient may present with pain and swelling of the involved gland during eating because saliva production is maximum at this time against a fixed obstruction. Patient may have on and off symptom of episodic swelling and discomfort or may have persistent symptom because of salivary fluid accumulation [6]. Radiological diagnostic approaches include conventional radiography, ultrsonography, computed tomography, sialography, MR sialography and sialoendoscopy. The treatment plan varies from conservative to surgical management that include transoral sialolithotomy, laser assisted sialolithotomy, extracorporeal and intracorporeal shock wave lithotripsy, sialoendoscopy and basket retrieval, salivary gland excision etc.
Case Report
In our case series of five patients; 3 female and 2 male of age group 20-40 years old. All the five patients were operated under general anesthesia after taking their consent. First female patient presented with the swelling on the left side of neck for 5 month swelling was 2 cm x 2.5 cm that usually increase after taking meal and associated with dull aching pain with spontaneous resolution within one hour after meal. In CECT neck well defined round to oval shaped hyper dense mass of 6.6 mm x 7.0 mm seen in the left submandibular space with proximal dilatation of its branches of the submandibular duct due to obstruction with adjacent minimal fat standing.
Second female patient of age 32 presented with chief complaint of pain during swallowing for solid from last one month. Pain was sudden in onset, non-progressive without any aggravating factor, pain was relieved by taking medication but it was referred to left ear. CECT neck shows hyper dense mass measuring 8 mm x 5mm along the course of the left sub mandibular duct in its distal part with normal submandibular gland without any periglandular fat standing.
Third female of 30 year old present with history of postprandial swelling for the last 8 months with disappear one to two hour after meal. Her ultrasound of neck shows hyperechoic foci of 6.3 mm x 3.4 mm in size in the region of right submandibular gland duct, whereas right and left gland appear to be normal in size and shape. Figure 1
Fourth patient is male of 24 year presented with generalized body aches from last 2 year with dull aching pain in the right submandibular area with history of swelling of 1.5 mm x 1.0 mm that appear after taking meal and disappear 1-2 hours after meal. Routine blood investigation reports were normal. Oropantogram (OPG) showing 4 mm x 3.5 mm radiopaque shadow in the right submandibular area. On ultrasound of bilateral submandibular gland right gland shows multiple small echogenic mass with the largest 3.2 mm seen in the sub mandibular duct causing its proximal dilatation of 6mm. Figure 2
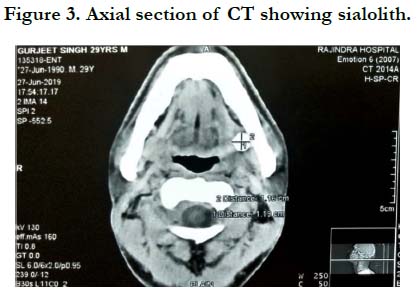
Fifth patient is also male of 29 year old who present with history of swelling at the left angle of mandible for the last 3-4 years. Swelling was insidious in onset, progressive, initially it was almond size and finally progressed to size of walnut it was associated with dull aching pain and slightly increased salivation. On palpation swelling was 3cm x 4 cm smooth, round, regular, mobile, nontender present in the left submandibular region approximately 5 cm from mentum and 4 cm below and behind the left ear tragus. It gives gritty sensation on bimanual palpation. His CECT Neck shows enlarged left submandibular gland of 3.2 cm x 2 cm with normal attenuation; hyperdense focus of 13 mm x 11 mm was seen in the proximal part of left submandibular duct causing proximal dilation of left submandibular duct with maximum diameter of 3.7 mm; one more hyperdense focus of 5.4 mm x 5.4 mm seen in the distal part of left submandibular duct in sublingual space tonsillolith is present in the palatine tonsil on right side; bilateral parotid glands and right submandibular gland appears normal. Figure 3 and 4
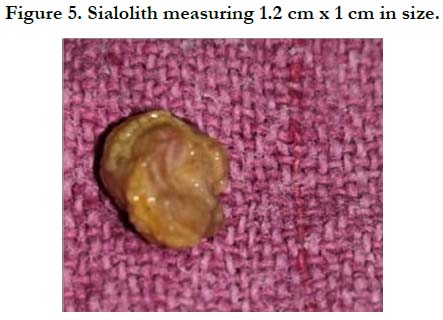
All the patients were operated under general anesthesia by transoral approach. After cleaning and draping, mouth prop inserted on same side and tongue retracted with suture. Both blunt and sharp dissection was used to expose the duct both anteriorly and posteriorly, lingual nerve was protected. Sometime stone not visualized so extra oral pressure made to push the deeper part of the duct intraorally. Floor of mouth sutured with 4-0 resorbable suture. Two weeks antibiotic, anti-inflammatory and antiseptic mouth wash was given to all the five patients. Recovery period was uneventful in all of them and were followed ups ranging from 1 week, 2 week, 1 month, 6 months and 1 year. No recurrence seen in the period of 2-4 years with normal or near normal salivary flow. Figure 5
Discussion
Sailolithiasis also known as mealtime syndrome and it is the second most common disease of the salivary gland. Stone may formed within the parenchyma or the ductal system of a salivary gland. Size of stone may varies from 1 mm to 1 cm, mean size is reported as 6 to 9 mm .Usually stone larger than 1cm considered large and rare [7-9]. Detail history taking and thorough examination is utmost important to make proper diagnosis. Common complaint with which patient presented to us is painless swelling, moderate discomfort to severe pain due to glandular swelling during meal time. If obstruction is complete causes constant pain and swelling. If pus is seen coming from the duct it may be associated with systemic infection [10]. Imaging play key role in diagnosis which include occlusal radiographs, sialography, Computed Tomography, Cone Beam Computed Tomography, MRI or Sialoendoscopy. Treatment modalities depend upon the duration of the symptom, size, and localization. Spontaneous exfoliation of stone might occur. Sialolith can be removed by excision of the stone or with the associated gland, as well as sialoendoscopy and lithotripsy.
Conclusion
Sailoliths may varies in size from millimeter to centimeter. Very often it was associated with sialadenitis. Mostly pain occur due to elevated intraglandular pressure resulting from salivary stimulation, which was increased at the meal time, so sometime called as “mealtime syndrome”. Treatment modalities from conservative to surgical management depending upon the size and location.
References
- Leung AK, Choi MC, Wanger GA. Multiple sialoliths and a sialolith of unusual size in the submandibular duct. Oral Surg Oral Med Oral RadiolEndod. 1999;87:331-3.Pubmed PMID:10102595.
- Iqbal A, Gupta AK, Natu SS, Gupta AK. Unusually large sialolith of wharton’ duct. Annals Maxillofaci Surg. 2012Jan ;2(1):70-3.Pubmed PMID:23483770.
- Zenk J, Benzel W, Iro H. New modalities in the management of human sialolithiasis. Minimally invasive therapy. 1994 Jan 1;3(5):275-84.
- Graziani F, Vano M, Cei S, Mario G. Unusual asymptomatic gaintsialolith of the sub mandibular gland: A clinical report . J Craniofacial Surg. 2006; 17[3]:549-52.Pubmed PMID:16770196.
- Marchal F, Kurt AM, Dulguerov P, Lehmann W. submandibular diagnostic and interventional sailendoscopy: new procedure for ductal disorders. Ann OtolRhinolLaryngol. 2002 Jan; 111(1):27-35. Pubmed PMID:11800367.
- Manjunath R, Burman R. gaint submandibular sialolith of remarkable size in the common area of Wharton’s Duct: J Oral Maxillofac Surg. 2009 Jun;67(6):1329-32.Pubmed PMID:19446227.
- Sinha P, Nagaraj T, Mahalakshmi IP, Suchetha DN. Submandibular gland sialolithiasis with chronic sialadenitis: A case report. International Journal of Medical and Dental Case Reports. 2014;1(1):1-4.
- Siddiqui SJ. Sialolithiasis: Anunusally large submandibular salivary stone. Br Dent J 2002 Jul 27;193(2):89-91.Pubmed PMID:12199129.
- Singhal A, Singhal P, Gupta R. Self exfoliation of large submandibular stone of two cases. ContempClin Dent.2012 Sep;3(Suppl 2):S185-7.Pubmed PMID:23230359.
- Pollack CV, Severance HW Jr.Sialolithiasis: case studies and review. J Eemerg Med. Sep-Oct 1990;8(5):561-5.Pubmed PMID:2254602.