The Effect Of Episiotomy On Sexual Functions In Primiparous Women: A Cross-Sectional Survey Study
Aydın Nihal Sevgi, Atalay Cemal Reşat*
Department of Gynecology and Obstetrics, Ankara City Hospital, Turkey.
*Corresponding Author
Dr. Cemal Resat Atalay,
Department of Gynecology and Obstetrics, Ankara City Hospital, Turkey.
Tel: +905323322020
Fax: + 903124398285
E-mail: atalaycemal@yahoo.com.tr
Received: April 29, 2022; Accepted: May 30, 2022; Published: June 15, 2022
Citation: Aydın Nihal Sevgi, Atalay Cemal Reşat. The Effect Of Episiotomy On Sexual Functions In Primiparous Women: A Cross-Sectional Survey Study. Int J Reprod Fertil Sex Health. 2022;8(1):147-152.
Copyright: Cemal Resat Atalay© 2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The aim of the study was to investigate and compare sexual dysfunction in the postpartum 6-10 weeks in primiparous
pregnant women who underwent mediolateral episiotomy and those who did not undergo episiotomy during normal
delivery.
Materials And Methods: This retrospective cross-sectional questionnaire study was conducted in Ankara City Hospital
between September 2019 and May 2021. Sexually active and healthy pregnant women who were between the ages of 18-35,
pregnant between 37-42 weeks, those with singleton pregnancies, low-risk pregnancies, birth weight within normal limits according
to the gestational week were included in the study. Nulliparous women who had the same characteristics were also
included in the control group. FSFI (Female Sexual Function Index) questionnaire was applied to all patients for sexual function
evaluation. SPSS 11.5 program was used in the analysis of the data.
Results: In the control group 11.5% of the patients had sexual dysfunction, this rate was found to be 26.2% in the group
without episiotomy and 37.7% in the group with episiotomy.
Conclusion: Women who gave birth with episiotomy had a higher rate of sexual dysfunction in the postpartum 6-10 weeks
than women who gave birth without episiotomy.
2.Material And Method
3.Results
4.Discussion
5.Conclusion
6.References
Keywords
Episiotomy; Sexual Dysfunction; Female Sexual Function Index.
Inrtoduction
Episiotomy was widely applied in the world until the first half of
the 19th century and its use gradually increased. In the following
years, it was applied in almost 63% of all births and almost all nulliparous
babies [1]. In this period, it was considered that repair of
episiotomy was easy and application of episiotomy had a reducing
effect on pelvic floor lacerations and prevented pelvic organ
prolapse, sexual dysfunction, and urinary/fecal incontinence in
the long term. It was believed that episiotomy protected the fetus
from pathologies e.g. asphyxia, cranial trauma, cerebral hemorrhage,
and mental retardation. However, there were increasing reports
that episiotomy did not provide these benefits in the second
half of the 20th century.
The routine use of episiotomy is no longer recommended because
of the lack of objective evidence-based data showing the
benefits of routine use [2]. In a meta-analysis involving 12 studies
comparing the use of restrictive episiotomy with routine use in
women expecting spontaneous vaginal delivery, restrictive episiotomy
resulted in up to a 30 % reduction in women who experienced
severe perineal or vaginal trauma. In this meta-analysis, no
significant differences were reported between the groups in terms
of postpartum 3rd day perineal pain, prolonged (six months or
more) dyspareunia, genital prolapse, or urinary incontinence [2].
Sexual problems are reported by about 40 % of women worldwide,
and about 12 % of these women (one in eight women)
actually have a sexual problem [3-7]. Female sexual dysfunction
takes different forms e.g. lack of sexual desire, impaired arousal,
inability to reach orgasm or pain in sexual activity. Sexual dysfunction
may be a problem from the beginning of the sexual activity
or may be acquired later in life after a period of normal sexual
function. The etiology of sexual dysfunction is often multifactorial
and can involve depression or anxiety, relationship conflicts, fatigue, stress, lack of privacy, problems with previous physical or
sexual abuse, medications, or physical and psychological problems
that make sexual activity difficult.
Female sexual dysfunction is diagnosed by taking a medical and
sexual history and determining the diagnostic criteria. There are
many validated questionnaires used in the evaluation of female
sexual function. Female Sexual Function Index (FSFI), is one of
the questionnaires developed to measure the quality of sexual life
and it was used in our study.
The aim of the study was to investigate and compare sexual dysfunction
in the postpartum 6-10 weeks in primiparous pregnant
women who underwent mediolateral episiotomy and those who
did not undergo episiotomy during normal delivery.
Materials And Method
This retrospective cross-sectional questionnaire study was conducted
in Ankara City Hospital between September 2019 and May
2021, after the approval from Ankara City Hospital Clinical Research
Ethics Committee No. 2 was obtained (date: 16.06.2021,
decision number: E2-21-615). The study was conducted on
pregnant women who had a mediolateral episiotomy or without
episiotomy in the delivery room of the Gynecology and Obstetrics
Hospital. Informed consent was obtained from all pregnant
women who participated in the study. Sexually active and healthy
pregnant women who were between the ages of 18-35, pregnant
between 37-42 weeks, those with singleton pregnancies, low-risk
pregnancies, birth weight within normal limits according to the
gestational week were included in the study. Nulliparous women
who had the same characteristics were also included in the control
group.
Pregnant women who had any chronic systemic disease, multiple
pregnancies, fetal or maternal obstetric complications, pregnant
women who had genital trauma or genital surgery for any reason,
and patients who did not have sexual intercourse at least three
times a week were excluded from the study. Also, patients who
did not want to participate in the questionnaire were excluded
from the study.
In this two-stage study, the files of the cases were scanned from
the archives and their demographic characteristics, gestational
week calculated according to the last menstrual date, birth weight,
age, weight, body mass index (BMI), smoking, alcohol use and
the participation in the childbirth education class were recorded
in the first stage.
In the second phase, the Female Sexual Function Index (FSFI),
which is one of the questionnaires developed to measure the quality
of sexual life, was employed. The patients who met the inclusion
criteria had the FSFI. In the second stage, the patients who
met the inclusion criteria had the FSFI form filled by the same
researcher, who was a gynecology and obstetrician by telephone
or face-to-face interviews, after obtaining their informed consent.
The sub-groups of the FSFI were; desire, arousal, lubrication, orgasm,
satisfaction, and pain. Each question is scored between 0
and 5. To be able to argue that there is sexual dysfunction, cut-off
values are calculated for the total score of the scale and the total
score of the sub-groups. The 1st and 2nd questions on the scale
made up the desire sub-group; the 3rd, 4th, 5th, and 6th questions,
the arousal sub-group; the 7th, 8th, 9th, and 10th questions,
the lubrication sub-group, the 11th, 12th, and 13th questions, the
orgasm sub-group , the 14th, 15th, and 16th questions made up
the satisfaction sub-group, and the 17th, 18th, and 19th questions
constituted the pain sub-group. The total score is obtained
by summing the scores of these six sub-groups, and the score
of the scale is calculated by multiplying the total score of each
sub-group with its factor coefficient. The total score is calculated
by multiplying the desire subscale score by 0.6, the arousal and
lubrication subscale scores by 0.3, and the orgasm, satisfaction,
and pain subscale scores by 0.4. The FSFI> 26.5 is interpreted
as no sexual dysfunction, and FSFI <26.5 is interpreted as sexual
dysfunction. The maximum score is 36, and the minimum score
is 2 on the scale.
The SPSS 11.5 program was employed in the analysis of the data.
Mean ± standard deviation and median (minimum-maximum)
were employed as descriptors for quantitative variables, and the
number of patients (percentage) was used for qualitative variables.
Whether there were differences between the categories of the
qualitative variables with two categories in terms of quantitative
variables was examined with the Student t-test if the normal distribution
assumptions were met, and with the Mann-Whitney U
test if they were not. The Kruskal Wallis H test was employed to
determine whether there were differences between the categories
of the qualitative variable with more than two categories in terms
of the quantitative variable because the assumptions of normal
distribution were not met. Paired groups causing significant differences
between the groups were examined using the Mann
Whitney U test with Bonferroni correction. The Chi-Square and
Fisher-Exact tests were employed to examine the relations between
two qualitative variables. The statistical significance level
was taken as 0.05.
Results
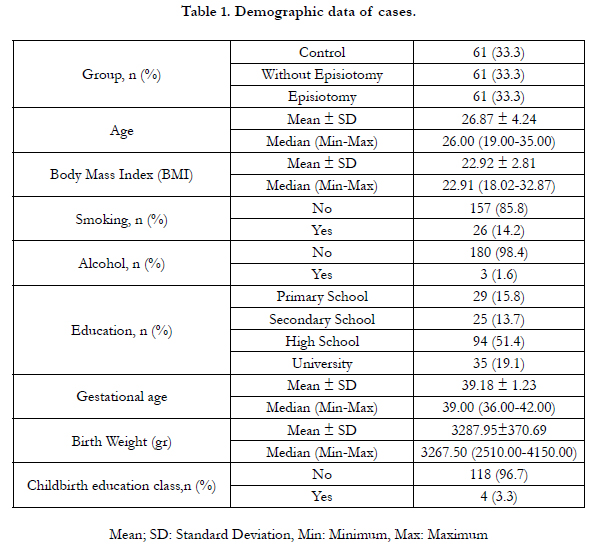
Demographic data of the patients are shown in Table 1.
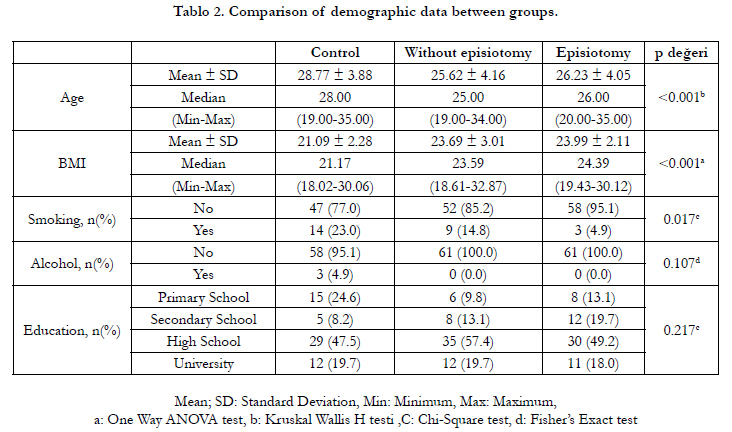
It was examined whether there was a difference between the three
groups in terms of demographic data and a significant difference
was found for age, BMI and smoking variables (p<0.001, p<0.001
and p=0.017), respectively (Table 2).
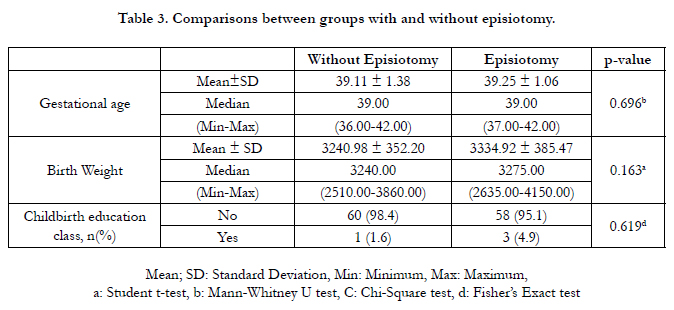
In Table 3, the comparisons between the groups with and without
episiotomy were examined in terms of variables, and no significant
difference was found between the groups.
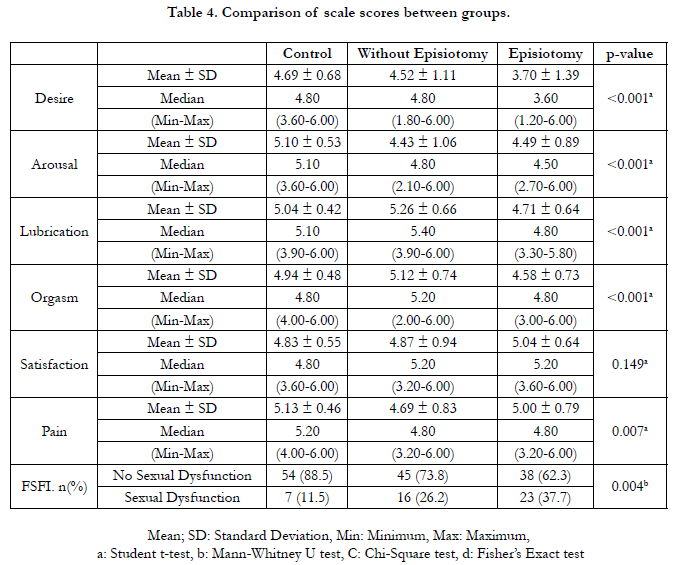
It was examined whether there was a difference between the three
groups in terms of scale scores, and no significant difference was
found only for the satisfaction subscale (p=0.149). (Table 4).
The mean desire scale score was 4.69 ± 0.68 in the control group,
4.52 ± 1.11 in the group without episiotomy, and 3.70 ± 1.39 in
the group with episiotomy. When the paired groups that caused
a significant difference between the three groups were examined,
the differences between the control-episiotomy and without
episiotomy-episiotomy groups were significant (p<0.001 and
p=0.001).
The mean arousal scale score was found to be 5.10 ± 0.53 in the control group, 4.43 ± 1.06 in the group without episiotomy,
and 3.70 ± 1.39 in the group with episiotomy. The differences
between the control-without episiotomy and control-episiotomy
groups were significant (p=0.001 and p<0.001).
Although the mean lubrication score was found to be highest in
the group without episiotomy, it was found to be the lowest in the
group with episiotomy. The differences between the control-episiotomy
and without episiotomy-episiotomy groups were found
to be significant (p=0.043 and p<0.001).
Similarly, the mean orgasm score was the highest in the group
without episiotomy, and it was the lowest in the group with episiotomy.
In terms of orgasm scores, only the difference between the groups without episiotomy and episiotomy was found to be
significant (p<0.001).
The mean pain scale score was found to be 5.13±0.46 in the control
group, 4.69 ± 0.83 in the group without episiotomy, and 5.00
± 0.79 in the group with episiotomy. The difference between the
control and without-episiotomy groups was found to be significant
(p=0.007). In the control group 11.5% of the patients had
sexual dysfunction, this rate was found to be 26.2% in the group
without episiotomy and 37.7% in the group with episiotomy (Table
4).
Discussion
Postpartum sexual function can be affected by various factors
(e.g. hormonal, psychological, social, anatomical factors), which
may cause sexual dysfunction in the postpartum period [8, 9].
According to previous studies, 20-60% of women experience
sexual dysfunction in the first 6 months after delivery [10-14].
The physical and psychological factors e.g. satisfaction, depression,
and delivery type were investigated concerning postpartum
sexual dysfunction. However, the results on the effects of these
factors on the postpartum sexual function of women are mostly
controversial.
Female sexual function is a vital part of life at any age and is affected
by many factors [15]. Especially pregnancy and childbirth
bring with them biological, psychological, and social changes,
which can affect sexual functions. There is a significant worsening
of all sexual areas (e.g. dyspareunia, lack of vaginal lubrication,
difficulty reaching orgasm, vaginal bleeding or irritation after intercourse,
and loss of sexual desire) in the postpartum period.
Studies show that the prevalence of sexual dysfunction ranges
from 41% to 83% in the 2-3 months after birth. In a study published
in 2000 comparing the prenatal (3rd trimester) and 6-month
postpartum conditions of 484 women, Barrett et al. found that
pain, lack of vaginal lubrication, and loss of sexual desire increased
significantly in the first 3 months after birth compared
to the pregnancy period. They also reported that although these
problems decreased 6 months after birth, they did not reach the
level of prenatal well-being [16].
A meta-analysis of Chinese primiparous women showed that
mode of delivery did not affect short and long term postpartum
sexual functions [17]. It was reported in a study that compared
restrictive approach and routine episiotomy, that 37% of women
who underwent restrictive approach and 27% of women who
underwent routine episiotomy resumed sexual intercourse one
month after delivery [18].
In a prospective study comparing vaginal delivery with and without
episiotomy in 243 cases, no difference was found between the
groups in sexual function at 1, 2, and 6 weeks postpartum [19]. A
limited number of studies comparing the results of the restrictive
approach and routine episiotomy reported that the frequency of
dyspareunia at the postpartum 3rd and 4th years did not differ at
significant levels between the groups [20, 21].
A meta-analysis that evaluated 12 studies and 6177 cases concluded
that there were no differences between the presence or
absence of episiotomy in women who reported painful sexual intercourse
6 months or more after birth.[2]
In another study, 158 primiparous cases that gave birth through
mediolateral episiotomy were evaluated. 135 women (85.4%) resumed
sexual activity after 3 months. The FSFI scale was employed
in the study and it was found that 55 (40.7%) of these
women had FSFI scores <26.55 and experienced symptoms of
sexual dysfunction. Desire disorders 68.9% and orgasm disorders
67.4% were the two most common problems. It was also reported
that pain during intercourse was a common problem (58.5%) and
59.3% of the participants were not satisfied with their sexual life.
[8].
In a cohort study by De Souza et al., postpartum sexual functions
were evaluated in the first 7-19 weeks, 6 months, and 12 months.
In this cohort, 54% of the women had a normal vaginal delivery,
21% had an instrumental delivery, and 25% had a cesarean section.
In this study, no difference was found in total FSFI or subgroup
scores by mode of delivery between the prenatal and the
12th month postnatal assessment [22].
In the present study, significant differences were detected between
women with and without episiotomy in terms of sexual desire.
These results are consistent with the results of previous studies
on this subject [16, 23]. Also, significant differences were detected
between the control group and the episiotomy group in terms of
sexual desire. The literature reports that postpartum sexual desire
is negatively affected [24]. However, most studies do not compare
groups of women with and without episiotomy, there are studies
comparing groups of primiparous women with mediolateral episiotomy
and women with cesarean section usually [25].
The mean postpartum orgasm score was found to be at the highest
level in the group without episiotomy. This result is in line
with the results of several studies that mention the ability to reach
orgasm rapidly after birth. These studies also reported that most
women regained their ability to orgasm six weeks after birth. [18,
25]. A significant difference was detected between the groups of
women with and without episiotomy in terms of the mean postpartum
orgasm score in our study.
In this study, the mean postpartum orgasm score of the without
episiotomy group was found to be higher than the control group.
Studies are reporting that there is an increased vascularization of
the labia minora and pelvic structures because of some hormonal
changes caused by childbirth, and as a result, orgasm is more
pronounced, and even many women experience their first orgasm
after their first pregnancy. Also, 25% of women were found to be
more satisfied with their sexual life after birth [26, 27].
There were a lot of studies on pain during sexual intercourse after
birth. As a result of the present study, significant differences were
found between the control group and the group without episiotomy.
In a previous study, it was found that women with intact
perineum had less pain than others [28]. In a study by Hartman et
al., it was found that the pain during sexual intercourse in women
who underwent episiotomy during childbirth was more than in
women who had a cesarean section or did not have perineal damage
[29]. However, some other studies suggest that perineal pain
was not affected by episiotomy [30].
In the present study, the mean satisfaction score was close to each
other in all three groups and no significant differences were detected.
According to the data obtained from the study of Klein
et al., women who underwent episiotomy were affected negatively
in terms of sexual satisfaction [31]. It was found in another study
that the satisfaction levels of women with intact perineum were
higher [28].
Conclusion
As a result of the our study that investigated the effects of episiotomy,
it was found that primiparous women who underwent
episiotomy had lower sexual functions at 6-10 weeks compared to
those without episiotomy. For this reason, we believe that restrictive
episiotomy is a more appropriate approach instead of routine
right mediolateral episiotomy in normal deliveries.
Although the power of the study increased with the results of a
single-center in our study, it still had limitations because it had a
retrospective design. Prospective and more comprehensive studies
are needed in this regard.
References
- Thacker SB, Banta HD. Benefits and risks of episiotomy: an interpretative review of the English language literature, 1860-1980. Obstet Gynecol Surv. 1983 Jun;38(6):322-38. PubMed PMID: 6346168.
- Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. 2017 Feb 8;2(2):CD000081. PubMed PMID: 28176333.
- Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008 Nov;112(5):970-8. PubMed PMID: 18978095.
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999 Feb 10;281(6):537-44. PubMed PMID: 10022110.
- Fugl-Meyer KS, Arrhult H, Pharmanson H, Bäckman AC, Fugl-Meyer AM, Fugl-Meyer AR. A Swedish telephone help-line for sexual problems: a 5-year survey. J Sex Med. 2004 Nov;1(3):278-83. PubMed PMID: 16422957.
- Laumann EO, Nicolosi A, Glasser DB, Gingell C, Wang T; GSSAB Investigators' Group. Sexual problems among women and men aged 40-80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res. 2005 Jan-Feb;17(1):39-57. PubMed PMID: 15215881.
- Zhang C, Tong J, Zhu L, Zhang L, Xu T, Lang J, et al. A Population-Based Epidemiologic Study of Female Sexual Dysfunction Risk in Mainland China: Prevalence and Predictors. J Sex Med. 2017 Nov;14(11):1348-1356. PubMed PMID: 29110805.
- Matthies LM, Wallwiener M, Sohn C, Reck C, Müller M, Wallwiener S. The influence of partnership quality and breastfeeding on postpartum female sexual function. Arch Gynecol Obstet. 2019 Jan;299(1):69-77. PubMed PMID: 30327862.
- Wallwiener S, Müller M, Doster A, Kuon RJ, Plewniok K, Feller S, et al. Sexual activity and sexual dysfunction of women in the perinatal period: a longitudinal study. Arch Gynecol Obstet. 2017 Apr;295(4):873-883. Pub- Med PMID: 28251311. /
- Alligood-Percoco NR, Kjerulff KH, Repke JT. Risk Factors for Dyspareunia After First Childbirth. Obstet Gynecol. 2016 Sep;128(3):512-518. PubMed PMID: 27500349.
- Banaei M, Kariman N, Ozgoli G, Nasiri M, Ghasemi V, Khiabani A, et al. Prevalence of postpartum dyspareunia: A systematic review and metaanalysis. Int J Gynaecol Obstet. 2021 Apr;153(1):14-24. PubMed PMID: 33300122.
- O'Malley D, Higgins A, Begley C, Daly D, Smith V. Prevalence of and risk factors associated with sexual health issues in primiparous women at 6 and 12 months postpartum; a longitudinal prospective cohort study (the MAMMI study). BMC Pregnancy Child birth. 2018 May 31;18(1):196. PubMed PMID: 29855357.
- Lagaert L, Weyers S, Van Kerrebroeck H, Elaut E. Postpartum dyspareunia and sexual functioning: a prospective cohort study. Eur J Contracept Reprod Health Care. 2017 Jun;22(3):200-206. PubMed PMID: 28447919.
- Khajehei M, Doherty M, Tilley PJ, Sauer K. Prevalence and risk factors of sexual dysfunction in postpartum Australian women. J Sex Med. 2015 Jun;12(6):1415-26. PubMed PMID: 25963126.
- World Health Organization. Defining sexual health: report of a technical consultation on sexual health, 28-31 January 2002, Geneva. World Health Organization; 2006.
- Barrett G, Pendry E, Peacock J, Victor C, Thakar R, Manyonda I. Women's sexual health after childbirth. BJOG. 2000 Feb;107(2):186-95. PubMed PMID: 10688502.
- Fan D, Li S, Wang W, Tian G, Liu L, Wu S, et al. Sexual dysfunction and mode of delivery in Chinese primiparous women: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2017 Dec 6;17(1):408. PubMed PMID: 29212464.
- Sleep J, Grant A, Garcia J, Elbourne D, Spencer J, Chalmers I. West Berkshire perineal management trial. Br Med J (Clin Res Ed). 1984 Sep 8;289(6445):587-90. PubMed PMID: 6432201.
- Chang SR, Chen KH, Lin HH, Chao YM, Lai YH. Comparison of the effects of episiotomy and no episiotomy on pain, urinary incontinence, and sexual function 3 months postpartum: a prospective follow-up study. Int J Nurs Stud. 2011 Apr;48(4):409-18. PubMed PMID: 20800840.
- Fritel X, Schaal JP, Fauconnier A, Bertrand V, Levet C, Pigné A. Pelvic floor disorders 4 years after first delivery: a comparative study of restrictive versus systematic episiotomy. BJOG. 2008 Jan;115(2):247-52. PubMed PMID: 17970794.
- Sleep J, Grant A. West Berkshire perineal management trial: three year follow up. Br Med J (Clin Res Ed). 1987 Sep 26;295(6601):749-51. PubMed PMID: 3119022.
- De Souza A, Dwyer PL, Charity M, Thomas E, Ferreira CH, Schierlitz L. The effects of mode delivery on postpartum sexual function: a prospective study. BJOG. 2015 Sep;122(10):1410-8. PubMed PMID: 25752211.
- Katz A. Sexually speaking: sexual changes during and after pregnancy. Am J Nurs. 2010 Aug;110(8):50-2. PubMed PMID: 20671497.
- Paterson LQ, Davis SN, Khalifé S, Amsel R, Binik YM. Persistent genital and pelvic pain after childbirth. J Sex Med. 2009 Jan;6(1):215-21. PubMed PMID: 19170851.
- Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005 Jul-Aug;16(4):263-7. PubMed PMID: 15838587.
- von Sydow K. Sexuality during pregnancy and after childbirth: a metacontent analysis of 59 studies. J Psychosom Res. 1999 Jul;47(1):27-49. PubMed PMID: 10511419.
- Inglis T. Postpartum sexuality. JOGN nursing. 1980 Sep 1;9(5):298-300.
- Signorello LB, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: a retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001 Apr;184(5):881-8. PubMed PMID: 11303195.
- Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J Jr, Lohr KN. Outcomes of routine episiotomy: a systematic review. JAMA. 2005 May 4;293(17):2141-8. PubMed PMID: 15870418.
- Botros SM, Abramov Y, Miller JJ, Sand PK, Gandhi S, Nickolov A, et al. Effect of parity on sexual function: an identical twin study. Obstet Gynecol. 2006 Apr;107(4):765-70. PubMed PMID: 16582110.
- Klein MC, Gauthier RJ, Robbins JM, Kaczorowski J, Jorgensen SH, Franco ED, et al. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. Am J Obstet Gynecol. 1994 Sep;171(3):591-8. PubMed PMID: 8092203.