Acute Generalized Exanthematous Pustulosis in a Child without Drug Intake: Clinical and Histological Features
Senhaji G*, El Jouari O, Zakia D, Lamouaffaq A, Elloudi S, Bay Bay H, Mernissi FZ
Department of Dermatology, University Hospital Hassan II, Fez, Morocco.
*Corresponding Author
Senhaji Ghita,
Doctor, Department of Dermatology, University Hospital Hassan II, Fez, Morocco
Tel: +212 600075857
E-mail: ghitasenhaji88@gmail.com
Received: November 02, 2018; Accepted: November 26, 2018; Published: November 28, 2018
Citation: Senhaji G, El Jouari O, Zakia D, Lamouaffaq A, Elloudi S, Bay Bay H, et al., Acute Generalized Exanthematous Pustulosis in a Child without Drug Intake: Clinical and Histological Features. Int J Pediat Health Care Adv. 2018;5(5):95-98. doi: dx.doi.org/10.19070/2572-7354-1800027
Copyright: Senhaji G© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Acute generalized exanthematous Pustulosis (AGEP) is a rare and sometimes life-threatening, cutaneous reaction caused by drugs in more than 90% of cases, with antibiotics the most frequent triggers. It is a potentially fatal skin reaction rarely observed in children and can be atypical in its presentation. Clinically, it is characterized by the acute onset of dozens of sterile, non-follicular, small pustules on edematous erythema, few hours to three weeks after exposure to the causative agent. The lesions begin on the face and/or skin folds, with widespread distribution after. Systemic symptoms are mild and the disease normally resolves spontaneously after the inciting agent is withdrawn. We report a rare case of AGEP in an 8-year-old boy with no history of drug intake. Through our case, we highlight the atypical clinical and histological presentation, with special concern of the therapeutic options especially in children.
2.Abbreviations
3.Introduction
4.Case Report
5.Discussion
6.Conclusion
7.References
Keywords
Acute Generalized Exanthematous Pustulosis; Pustular Dermatosis; Generalized Pustular Psoriasis; Non-Follicular Pustules; Histology.
Abbreviations
AGEP: Acute Generalized Exanthematous Pustulosis; IL-8: Interleukin-8; GM-CSF: Granulocyte-Macrophage Colony-Stimulating Factor; TEN: Toxic Epidermal Necrolysis; GPP: Generalized Pustular Psoriasis; DRESS: Drug Reaction with Eosinophilia and Systemic Symptoms.
Introduction
Acute generalized exanthematous Pustulosis (AGEP) is a rare and sometimes life-threatening, cutaneous reaction caused by drugs in more than 90% of cases [1], with antibiotics the most frequent triggers [2]. Exposure to mercury and/or viruses have also been implicated in the pathogenesis of this disorder [3]. It is reported as an uncommon condition in children [4], with most cases reported in adults [1]. Clinically, it is characterized by the acute eruption of dozens to hundreds of monomorphous, nonfollicular, sterile pustules on an erythematous base followed in a few days by pinpoint desquamation [2]. Systemic symptoms are mild and the disease normally resolves spontaneously after the inciting agent is withdrawn [5]. We report a rare case of AGEP in an 8-year-old boy with no history of drug intake. Through our case, we highlight atypical clinical and histological presentation, with special concern of the therapeutic options especially in children.
Case Report
An 08 years-old boy, without significant pathological history, presented 10 days before his consultation a painless and very itchy erythematous maculopapular eruption, starting in the trunk, and extending after to the big folds, the face and the limbs, without fever, arthralgia, digestive disorders or prior medication intake. Medical history found that he had been suffering, three days before, from a generalized asthenia associated with rhinorrhea.
Dermatological examination revealed multiple confluent erythematous papules in large erythematous and infiltrated placards on the trunk, folds, back, limbs and forehead, covered with hundreds of lactescent white micropustules, with mild pharyngeal erythema, but without associated lymphadenopathy.
Laboratory investigations were made showing leukocytosis at 15000 with neutrophilia and hypereosinophilia at 1670. A cutaneous showed the presence of a spongiotic dermatitis with subcutaneous and Intraepidermal spongiform and sterile micropustules, filled with many neutrophils mixed with some eosinophils, with a predominantly lymphocytic and neutrophilic dermal infiltrate, and the presence of some apoptotic keratinocytes.
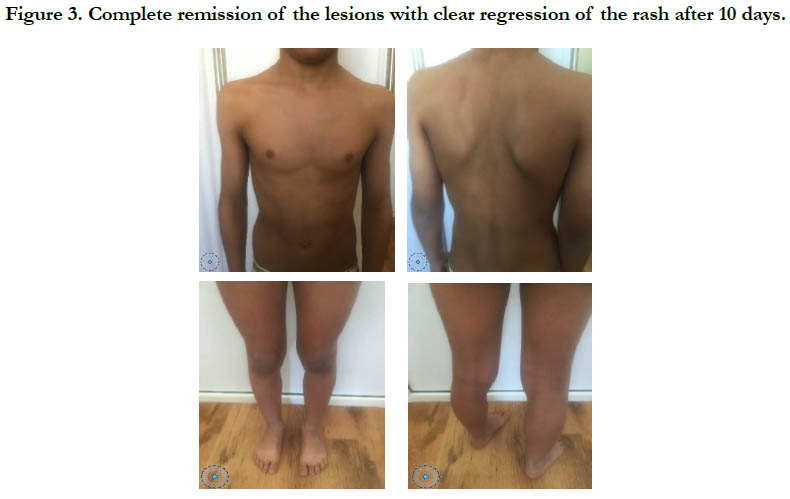
A diagnosis of acute generalized exanthematous pustulosis was done. A treatment with dermocorticoids in association to antihistamines was given with very good improvement and clear regression of his rash in 10 days. The evolution was marked by the complete remission of lesions without appearance of new eruption with a decline of 12 months.
Figure 1. Widespread erythematous papulopustules confluent in large infiltrated placards on the trunk and the back.
Discussion
Acute generalized exanthematous pustulosis was first introduced in the French literature in 1980 by Beylot et al., [3]. It is a potentially fatal skin reaction rarely observed in children and can be atypical in its presentation [6], as in our case where the patient presented with atypical widespread erythematous papules and placards covered by multiple lactescent micropustules. The causes of this entity vary widely and cases reporting new causative agents continue to appear [5]. In children, it is mainly attributed to drugs as antibiotics, antipyretic analgesics and vaccines [7]. Some of the most notorious AGEP-inducing drugs include the beta-lactam antibiotics (penicillins, cephalosporins, and aminopenicillins), macrolides, calcium-channel blockers (diltiazem in particular), antimalarials (hydroxychloroquine and chloroquine), quinolones, sulfonamides, terbinafine, carbamazepine, and acetaminophen [5]. Much less commonly, viral agents such as enterovirus and Epstein- Barr virus [2], and mercury exposure have been suggested in the literature as other possible triggers in both adults and children [6]. Other times it can be attributed to factors such as food, essential oils, food supplement, chemicals for professional use [1].
The etiopathogenesis of this rare disease is still not fully elucidated although some progress has been made [8]. Positive patch test results proposed that AGEP is a delayed type of hypersensitivity reaction (type IV) [4], thus supporting a drug etiology and the concept that T cells play a crucial role [8]. Furthermore, Recruitment of activated T cells and their production of interleukin-8 (IL-8) and granulocyte-macrophage colony-stimulating (GM-CSF) factor appear to be crucial [2], by enhancing neutrophilic inflammation and survival, thus leading to sterile pustular lesions [8]. Indeed, this has been noticed in our patient where the histology showed intraepidermal sterile micropustules filled with neutrophils and eosinophils.
Clinically, it is characterized by the acute onset of dozens of sterile, non-follicular, small pustules on edematous erythema [8]. The first signs of disease can appear as rapidly as a few hours to three weeks after exposure to the causative agent [5], with an average of 5 days [3]. The lesions begin on the face and/ or skin folds, with widespread distribution after [8]. Cutaneous manifestations are often accompanied by systemic symptoms like asthenia, chills and lymphadenopathy [4], however, fever is occasionally absent [6]. The pustules disappear spontaneously in few days, typically followed by post pustular desquamation with a characteristic pattern of punctate desquamation, and the reaction fully resolves within 15 days [6, 8].
Laboratory findings usually show eosinophila, reduced creatinine clearance, and mildly elevated aminotransferases [5].
To confirm the diagnosis, patch tests are being used but the results are not always positive [3]. Thing that leads authors like, Sidoroff et al., to propose a scoring system based on several criteria to make the diagnosis of AGEP [5]. It includes an acute pustular eruption, fever (‡38_C), leucocytosis (‡7000/ll), neutrophilia with or without a mild eosinophilia, subcorneal or intradermal pustules on skin biopsy and spontaneous resolution in <15 days [4]. This scoring algorithm would label the diagnosis as excluded, possible, probable, or definite according to the morphological and histological findings and clinical course of the presenting patient [5]. Our case scored 8, which reinforced our diagnosis.
PEAG is clinically difficult to distinguish from other pustular dermatoses [7], such as bacterial folliculitis, subcorneal pustular dermatosis (Sneddon-Wilkinson disease), Immunoglobulin A pemphigus, toxic epidermal necrolysis (TEN) and drug reaction with eosinophilia and systemic symptoms (DRESS) [1], the main differential diagnosis is a generalized pustular psoriasis (GPP), von Zumbusch type [3]. Histologically, both diseases are similar [3], as both diseases represent a dynamic spongiotic pustular process [8], but the typical changes of psoriasis such as acanthosis and papillomatosis are usually absent in AGEP [7]. Furthermore, the presence of prominent edema of the papillary dermis should suggest AGEP [3]. In our case, the diagnoses of AGPE, pustular psoriasis, generalized eosinophilic papulo pustulosis of Ofugi, lichenoid toxidermy and DRESS syndrome were discussed.
Moreover, as the treatment options differ greatly, skin biopsy should be undertaken to differentiate AGEP from other pustular dermatoses such as GPP [7]. Histologically, two main patterns are observed in AGEP [3]. A minority of patients show features of leukocytoclastic vasculitis with neutrophilic collections both below and within the epidermis [3]. However, in most patients, we usually find subcorneal and/or intraepidermal pustules, papillary dermis edema, neutrophilic and/or occasional eosinophilic perivascular infiltration and keratinocyte necrosis [5], without evidence of vasculitis [3].
Neither clinical nor histopathological aspects can confirm the diagnosis, which insist on the importance on clinicopathological correlation. This was the case of our patient, it illustrates well the difficulty of the diagnosis. In fact, clinically, the patient presented with multiple widespread erythematous papules and placards covered with hundreds of non-follicular subcorneal lactescent pustules with an eosinophilia, whereas the histology had shown intraepidermal spongiform and sterile micropustules, filled with neutrophils and eosinophils, with some apoptotic keratinocytes, and it is the clinicohistological confrontation that allowed us to retain the diagnosis.
No specific treatment is recommended for AGEP [4]. Withdrawal of the suspected drug, if drug origin is suspected, and supportive care according to clinical situation are recommended [4]. Antipyretics, moist dressings, and disinfecting agents during the pustular stage and moisturizing agents during the desquamation (post-pustular) phase have been recommended for symptomatic relief and prevention of complications such as a secondary infection [5]. Corticosteroids are generally unnecessary because their benefit in AGEP has yet to be established, however, they can be considered in severe cases [5]. In our patient, dermocorticoids were used due to the presence of a generalized eruption, in order to relieve pruritus.
Generally, the disease is self-limited, although there is a 1-2% mortality rate as a result of a high fever or secondary infection [5]. However, internal organs are usually not involved and overall prognosis is good [8].
Conclusion
Summary, our case illustrated the atypical clinical and histological presentation of PEAG in a child, and insist on the importance of clinicopathological confrontation to differentiate it from other pustulosis, especially GPP, in childhood are important to terminate the exposure to the causative agent and to avoid unnecessary testing and treatment.
References
- Boccaletti V, Cortelazzi C, Fantini C, Tognetti E, Fabrizi G, Pagliarello C, et al. Acute Generalized Exanthematous Pustolosis Following Paracetamol ingestion in a Child. Pediatr Allergy Immunol. 2015 Jun;26(4):391-2. doi: 10.1111/pai.12386. PubMed PMID: 25845401.
- Lane L, McCoppin HH, Dyer J. Acute generalized exanthematous pustulosis and Coombs-positive hemolytic anemia in a childfollowing Loxosceles reclusa envenomation. Pediatr Dermatol. 2011 Nov-Dec;28(6):685-8. doi: 10.1111/j.1525-1470.2010.01302.x. PubMed PMID: 22082464.
- Lee UH, Yang JH, Choi JC, Chun DK. Acute generalized exanthematous pustulosis in a six-year-old boy. J Dermatol. 2004 Jun;31(6):497-9. PubMed PMID: 15235193.
- Ozmen S, Misirlioglu ED, Gurkan A, Arda N, Bostanci I. Is acute generalized exanthematous pustulosis an uncommon condition in childhood? Allergy. 2010 Nov;65(11):1490-2. doi: 10.1111/j.1398-9995.2010.02377.x. PubMed PMID: 20486903.
- Badawi AH, Tefft K, Fraga GR, Liu DY. Cetirizine-induced acute generalized exanthematous pustulosis: a serious reaction to a commonly used drug. Dermatol Online J. 2014 May 16;20(5):22613. PubMed PMID: 24852773.
- Ersoy S, Paller AS, Mancini AJ. Acute generalized exanthematous pustulosis in children. Arch Dermatol. 2004 Sep;140(9):1172-3. PubMed PMID: 15381568.
- Bayata S, Ermertcan AT, Ates M, Temiz P. Acute generalized exanthematous pustulosis in a child probably induced by terbinafine. Indian J Dermatol Venereol Leprol. 2015 Jan-Feb;81(1):95. doi: 10.4103/0378-6323.148614. PubMed PMID: 25566924.
- Kardaun SH, Kuiper H, Fidler V, Jonkman MF. The histopathological spectrum of acute generalized exanthematous pustulosis (AGEP) and its differentiation from generalized pustular psoriasis. J Cutan Pathol. 2010 Dec;37(12):1220-9. doi: 10.1111/j.1600-0560.2010.01612.x. PubMed PMID: 20738458.