Cardiometabolic Risk Profile and its Relation with the Waist Circumference to Height Ratio in Turkish School-Age Children
Karaagac AT1*, Erdönmez D2
1 Kartal Koşuyolu Research and Training Hospital, University of Health Sciences, Pediatry, Istanbul, Turkey.
2 Acıbadem University Hospital Faculty of Medicine, Pediatry, Istanbul, Turkey.
*Corresponding Author
Aysu Türkmen Karaağaç, MD
Kartal Koşuyolu Research and Training Hospital,
University of Health Sciences, Denizer Cad,
Cevizli Kavşağı, No:2, 34846, Kartal, Istanbul, Turkey.
Tel: 0(533)5679965
Fax: 0(216)5001500/1101
E-mail: aysukaraagac@gmail.com
Received: June 13, 2017; Accepted: November 13, 2017; Published: November 15, 2017
Citation: Karaagac AT, Erdönmez D. Cardiometabolic Risk Profile and its Relation with the Waist Circumference to Height Ratio in Turkish School-Age Children. Int J Pediat Health Care Adv. 2017;4(7):59-62. doi: dx.doi.org/10.19070/2572-7354-1700017
Copyright: Karaagac AT© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Obesity, cardiovascular diseases and diabetes have been rapidly increasing in pediatric age group all around the world. Therefore, cardiometabolic risk factors (CMRF) should be carefully screened beginning from the school ages. The aim of this study was to define the CMRF and to determine their correlations with the weight for height ratios (WHtR) in Turkish school-age children.
Methods: 6-12 year-old, 310 overweight children (150 females, 160 males) evaluated in the pediatry outpatient clinic of Kartal Koşuyolu Research and Training Hospital between January, 2016-February, 2017 were enrolled in this cross-sectional study. Their weights, heights, waist circumferences (WC) and blood pressures were recorded; body mass indices (BMI) and WHtR were calculated; blood glucose, cholesterol and triglyceride levels were analyzed. Children with BMI ≥ 85th percentile were accepted as overweight. The correlations between the CMRF, age and gender of children and their WHtR were analyzed statistically.
Results: Dyslipidemia, increased BMI and WC were more common CMRF than hypertension and hyperglycemia in Turkish school-age children. CMRF had quite significant relationship with gender and moderately significant relation with age. Male children had higher lipid, glucose and blood pressure levels than females. Moreover, a significant association was demonstrated between the CMRF and WHtR in both gender. (p values <0.05).
Conclusion: Male children carry higher cardiometabolic risk than their female counterparts. WHtR can be used to detect children with increased CMRF in pediatric outpatient clinics. It is important to take measures to prevent morbidity and mortality due to metabolic syndrome in adult life.
2.Introduction
3.Material And Methods
3.1 Statistical analysis
4.Results
5.Discussion
6.References
Keywords
Cardiometabolic Risk Factors; Children; Height; Waist Circumference; Weight; Ratio.
Introduction
Cardiometabolic risk refers to a high risk for cardiovascular diseases and diabetes due to obesity, hyperglycemia, dyslipidemia and hypertension [1, 2]. As the school-age children have increasingly common sedentary life styles and tendency to consume junk food, they have become more vulnerable to obesity and related cardiometabolic risk factors (CMRF). These children should be defined and regularly controlled due to the increased morbidity and mortality risks later in adult life [1, 3, 4]. Although waist circumference (WC) and body mass index (BMI) are used as the major determinants of obesity, WC correlates more strongly with visceral adipose tissue than BMI, both in adults and in children. However, cardiometabolic risks are expected to be different between two people with the same WC, but different heights [5]. This study was designed to determine the cardiometabolic characteristics, BMI and WHtR of Turkish school-age children and to analyze whether WHtR could be utilised for screening the children with increased CMRF/.
Material And Methods
6-12 year-old (mean 9.4 ± 2.03 years) 310 overweight schoolage children (150 females, 160 males) were included in this cross sectional study. They were evaluated in the pediatry outpatient clinic of Kartal Koşuyolu Research and Training Hospital, University of Health Sciences between January, 2016 and February, 2017. The medical histories of the children and the written consents for the study were obtained from their parents. The mothers stated that their children had been overweight from the infancy. None of them was on medication nor have had a chronic illness. The heights and weights of the children were measured twice, with the shoes off, and the average was recorded. BMI was calculated by dividing the weight in kilograms by the square of height in meters. Children with BMI ≥ 85 percentile for age and sex were accepted as overweight [6]. WC was measured at the approximate midpoint between the lower margin of the last palpable rib and the top of the iliac crest of the child at the end of a normal expiration. This measurement was performed twice by a non-elastic tape, in a standing position, according to the instructions of World Health Organisation (WHO) stepwise approach to surveillance protocol [7]. The average was recorded and females with WC ≥ 76 cm and males with WC ≥ 86 cm were accepted to have central obesity, according to the Turkish children specific WC cutoff points [8]. After 30 minutes of resting, their blood pressures were measured twice by a standard sphygmomanometer, with 10 minutes interval. The average was recorded as the final value of blood pressure. The children with systolic and diastolic blood pressures ≥ 90th percentile (age, sex and height specific) and the ones receiving antihypertensive treatment were accepted as hypertensive [4]. Their venous blood samples were obtained after 12 hours of fasting to measure blood glucose, total cholesterol, high and low density lipoprotein cholesterols (HDL-C, LDL-C) and triglyceride levels by the enzymatic spectrophotometric method. High fasting glucose levels (≥110 mg/dl), hypercholesterolemia (≥200 mg/dl), low HDL (<40 mg/dl), high LDL (≥100 mg/dl), hypertriglyceridemia (≥110 mg/dl), high BMI and WC values were accepted as the major CMRF according to the International Diabetes Federation (IDF) criteria [9, 10]. The study was approved by the Ethical Committee.
Continuous variables were expressed as mean ± SD and categorical variables as percentages (%). Chi-square and Fischer’s exact tests were used to campare the categorical variables. Linear regression analysis was performed to show the relationship between the WHtR adjusted for age and sex of children and CMRF. Spearman’s correlation test was applied to compare the continuous variables. All statistical analyses were performed by SPSS version 15.0 and p values < 0.05 were accepted as statistically significant.
Results
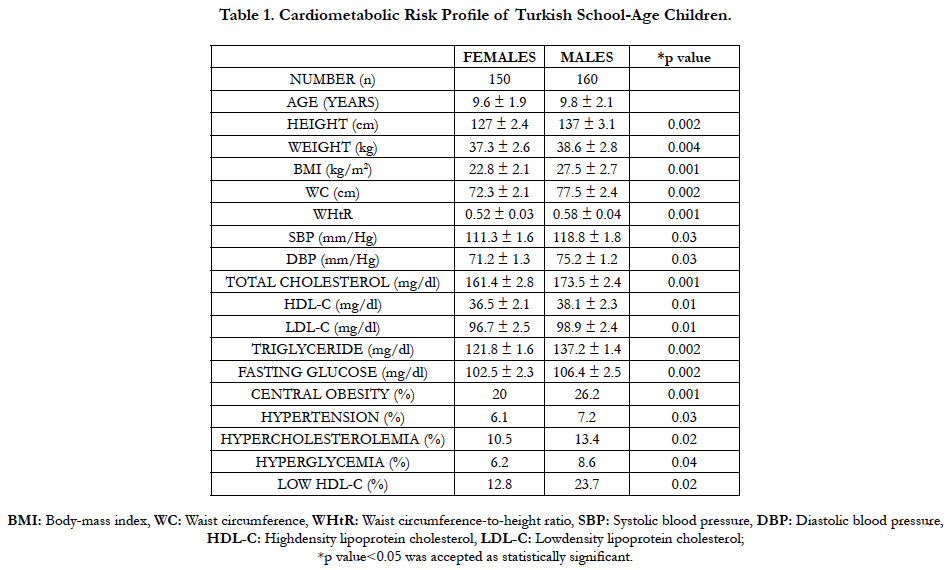
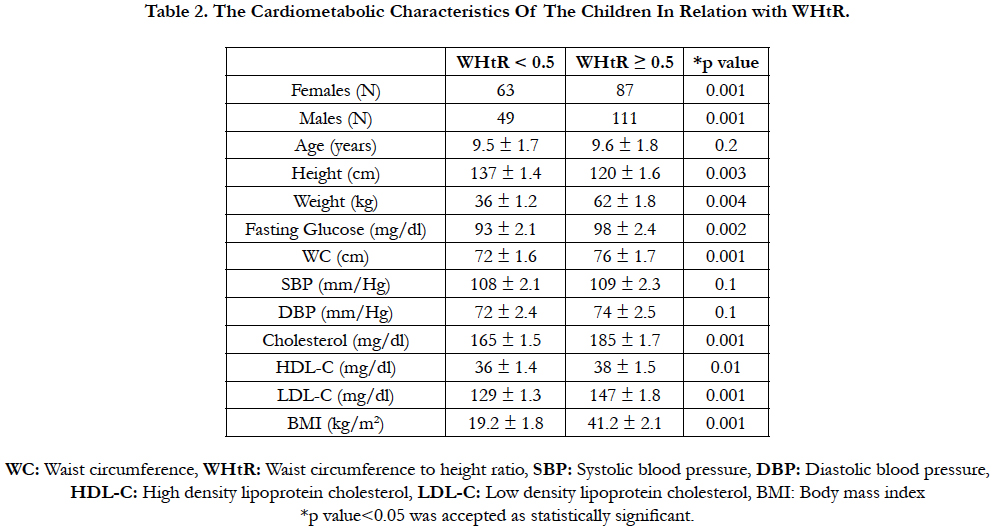
In the present study there were 150 (48.4%) female and 160 (51.6%) male children aged between 6-12 years (mean 9.6±1.9 and 9.8 ± 2.1 years respectively). Their cardiometabolic characteristics showed that they had dyslipidemia, increased WC and high BMI rather than hypertension and hyperglycemia as the major CMRF (Table 1). There were central obesity in 52/150 (34.6%) female children and in 65/160 (40.6%) male children. There was a significant correlation between hypertension, hyperglycemia and gender (p<0.05). Male children were found to have higher total blood cholesterole and lower HDL-C levels than females (13.4-10.5% and 23.7-12.8% respectively) (all p values<0.05). It was also shown that male Turkish school-age children had significanlty higher BMI, WC and WHtR than their female counterparts (all p values<0.05). Moreover, on linear regression analysis adjusted for age and gender, it was found that there was a highly significant correlation between WHtR and WC, blood glucose, triglyceride, cholesterol, HDL-C, LDL-C levels and a moderately significant correlation with SBP in overweight children (all p values<0.05) (Table 2). When the cardiometabolic characteristics of the children were grouped in relation with WHtR, it was found that the prevelances of CMRF ( weight, height, total cholesterol, HDL-C, glucose, SBP, DBP) were significantly higher in children with a WHtR ≥ 0.5 than those with a WHtR < 0.5 (all p values <0.05) (Table 2).
Discussion
This study showed that high BMI, increased WC and dyslipidemia rather than hypertension and hyperglycemia were the major CMRF in Turkish school-age children, male children have more CMRF than females regardless of age and that WHtR could be used confidentally for screening the children with CMRF. Nearly a quarter of the world’s adult population have been suffering from CMRF as dyslipidemia, hypertension and/or hyperglycemia/ impaired glucose control in addition to central obesity [9, 10]. CMRF are also appearing with a rapidly rising frequency among children [11, 12]. For example, in a study from China it has been reported that the overweight and obesity in urban school-age children increased from 8% in 1991 to 12% in 1997 [12]. The International Obesity Task Force (IOTF) has recently reported that at least 10% of children all around the world, representing 155 million children, aged between 5 and 17 years are overweight or obese [13]. The present study showed that there were central obesity in 34.6% of Turkish school-age female children (mean WC of 72.3 ± 4.1 cm and BMI of 22.8 ± 2.4 kg/m2) and in 40.6% of male children (mean WC of 78.5 ± 5.4 cm and BMI of 27.5 ± 3.1 kg/m2). Moreover, male children had significantly higher blood glucose, triglyceride, total and LDL cholesterol levels than their female counterparts, which demonstrate a higher tendency to metabolic syndrome (MS) in adult life. Several studies as Bogalusa Heart Study and NHANES III have demonstrated a relationship between childhood obesity and elevated risk of cardiovascular disease and diabetes, leading to MS, later in adult life [14, 15]. Although WC and BMI are used as the major determinants of obesity, WC correlates more strongly with visceral adipose tissue than BMI, both in adults and in children. However, the limitation of WC is that the cardiometabolic risk may be different between two people with the same WC, but different heights [5, 17]. Therefore, in the present study, WHtR was used to determine the CMRF in Turkish school-age children in addition to the measurements of weight, WC, blood pressure, blood glucose, total cholesterol, HDL-C and triglyceride levels. As in similar studies [18-20], it was demonstrated that the children with WHtR ≥ 0.5 had higher prevalence of CMRF than those with WHtR < 0.5, both in female and male children. The present study showed that Turkish school-age children with WHtR ≥ 0.5 had significantly higher weight, height, total cholesterol, lower HDL-C, and moderately higher blood pressure and glucose levels than those with WHtR < 0.5. In a recent study, Saydah et al. , found that people with a WHtR ≥ 0.65, aged between 12 and 39 years, had 139% greater risk of mortality before the age of 55 than those with a WHtR < 0.65 [21]. Therefore, results of the studies related with CMRF in children should be taken into consideration seriously by pediatricians and health policy makers for early detection and prevention of CMRF to reduce premature morbidity and mortality in adulthood. The major limitation of this study was the number of the study population. As the study was conducted in a tertiary referral center of cardiovascular surgeries, the number of 6-12 year old obese children, according to the IDF suggestions, was limited. However, the results were encouraging to make further investigations about the CMRF in school-age children throughout the country. The present study showed that WHtR and WC could be used together for screening the children with higher CMRF in pediatric outpatient clinics. Such screening programmes may also be organized for different age groups at different levels of education and the children with higher CMRF may be referred to hospitals for detailed investigation and diet programmes as preventive measures.
References
- Maffeis C, Banzato C, Talamini G; Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr. 152(2):207–213. PubMed PMID: 18206690.
- Lauer MS, Fontanarosa PB. Executive Summary Of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001 May 16;285(19):2486–2497. PubMed PMID: 11368702.
- Ahmed A, Ali SW, Massodi S, Bhat MA. Blood Pressure to height Ratio as aScreening Tool for Hypertension in Children. Indian Pediatrics J. 2016 Feb;53(2):137-139. PubMed PMID: 26897146.
- Lee S, Bacha F, Arslanian SA. Waist Circumference, Blood Pressure and Lipid Components of the Metabolic Syndrome. J Pediatr. 2006 Dec;149(6):809- 816. PubMed PMID: 17137898.
- Brambilla P, Bedogni G, Moreno LA, Goran MI, Gutin B, Fox KR, et al., Cross validation of Anthropometry Against Magnetic Resonance Imaging for the Assessment of Visceral and Subcutaneous Adipose Tissue in Children. Int J Obes (Lond). 2006 Jan; 30(1):23-30. PubMed PMID: 16344845.
- WHO. Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. PubMed PMID: 14726171.
- WHO. Waist circumference and waist – hip ratio: Report of a WHO expert consultation, Geneva, Switzerland; 2011.
- Hatipoğlu N, Ozturk A, Mazicioğlu MM, Kurtoğlu S, Seyhan S, Lokoğlu F. Waist Circumference Percentiles for 7 to 17 – year Old Turkish Children and Adolescents. Eur J Pediatr. 167(4):383-389.
- Alberti KG, Zimmet PZ, Shaw JE. The metabolic syndrome in children and adolescents. Lancet. 2008 369(9579):2059-2061.
- Zimmet P, Alberti KGMM, Kaufman F, Tajima N, Silink M, Arslanian S, et al., The metabolic syndrome in children and adolescents–an IDF consensus report. Pediatric Diabetes. 2007 8(5): 299-306. PubMed PMID: 17850473. PubMed PMID: 178504073.
- Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and Metabolic Syndrome in Children and Adolescents. N Engl J Med. 2007 350(23):2362-2374. PubMed PMID: 15175438.
- Wang Y, Lobstein T. Worldwide Trends in Childhood Overweight and Obesity. Int J Pediatric Obes. 2006;1(1):11-25. PubMed PMID: 17902211.
- Lobstein T, Baur L, Uauy R. IASO International Obesity Task Force. Obesity in Children and Young People: A Crisis in Public Health. Obes Rev. 5(Supp 1):4-104.
- Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of Childhood Obesity to Coronary Heart Disease Risk Factors in Adulthood: The Bogalusa Heart Study. Pediatrics. 2001 Sep;108(3):712-718. PubMed PMID: 11533341.
- Azadbakht L, Kelishadi R, Khodarahmi M, Qorbani M, Heshmat R, Motlagh ME, et al., The Association Of Sleep Duration and Cardiometabolic Risk Factors in a National Sample of Children and Adolescents: the CASPIAN III study. Nutrition. 2013 29(9):1133-1141.
- Morrison JA, Friedman LA, Wang P, Glueck CJ. Metabolic Syndrome in Childhood Predicts Adult Metabolic Syndrome and Type 2 Diabetes Mellitus 25 to 30 years later. J Pediatr. 2008 Feb;152(2):201-206. PubMed PMID: 18206689.
- Sungry RY, So HK, Choi KC, Nelson EA, Li AM, Yin JA, et al., Waist Circumference and Waist-to Height Ratio of Hong Kong Chinese Children. BMC Public Health. 2008; 8:324-325.
- Hirschler V, Aranda C, Calcagno M de L, Maccalini G, Jadzinsky M. Can Waist Circumference Identify Children With the Metabolic Syndrome? Arch Pediatr Adolesc Med. 2005 Aug;159(8):740-744. PubMed PMID: 16061781.
- Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health riskks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. 2005 Aug;56(5): 303-307. Pubmed PMID: 16236591.
- Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al., Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001b Apr;24(4):683-689. PubMed PMID: 11315831.
- Saydah S, Bullard KM, Imperatore G, Geiss L, Gregg EW. Cardiometabolic Risk Factors Among US Adolescents and Young Adults and Risk of Early Mortality. Pediatrics. 2013 Mar;131(3):e679-e686.