The Effect of Ad Libitum Carbohydrate-Electrolyte or Placebo Solution Intake on Fluid Balance and Soccer Skill Performance of Preadolescent Boys in Warm Environment
Chryssanthopoulos C1*, Mastellos P1, Philippou A2, Maridaki M1
1 School of Physical Education and Sports Science, National and Kapodistrian University of Athens, Greece.
2 Department of Experimental Physiology, Medical School, National and Kapodistrian University of Athens, Greece.
*Corresponding Author
Costas Chryssanthopoulos,
School of Physical Education and Sports Science,
National and Kapodistrian University of Athens,
41 Ethnikis Antistasis Street, Dafni, Athens, 172 37, Greece.
Tel: 210-7276113
E-mail: chryssan@phed.uoa.gr
Received: July 21, 2017; Accepted: August 29, 2017; Published: September 01, 2017
Citation: Chryssanthopoulos C, Mastellos P, Philippou A, Maridaki M. The Effect of Ad Libitum Carbohydrate-Electrolyte or Placebo Solution Intake on Fluid Balance and Soccer Skill Performance of Preadolescent Boys in Warm Environment. Int J Pediat Health Care Adv. 2017;4(5):41-47. doi: dx.doi.org/10.19070/2572-7354-1700013
Copyright: Chryssanthopoulos C© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
This study compared the effect of a carbohydrate-electrolyte or placebo solution on fluid balance and soccer skill performance of preadolescent boys exercising in warm environment. Sixteen soccer academy club players aged 10.4 ± 0.1 years (Tanner stage: 2.1 ± 0.1) performed two identical 60 min training sessions at about 29°C and relative humidity 38-43% while ingesting ad libitum and randomly either a 6% carbohydrate-electrolyte solution (CHO-E) or an artificially sweetened placebo (P). After the completion of the training, participants performed five soccer skill tests (SST). The SST had also been performed in a previous occasion when children had undergone only a 10-min warm-up (BestP). Body mass (BM) was maintained after training in both conditions, whereas BM loss, estimated sweat loss, percentage of BM loss, heart rate, perceived rate of exertion, abdominal discomfort and thirst were not different between trials. Fluid intake was higher in CHO-E (642 ± 50 ml, range: 300-985 ml) compared to P (458 ± 56 ml, range: 80-1010 ml) (p=0.017). Performance in SST was not deteriorated as a result of the training and was not different between BestP, CHO-E and P. Fluid intake was not correlated with sweat loss (r=0.14). It is concluded that, when exercising for 60 min in warm conditions and have access to fluid, children maintain their fluid balance and soccer skill performance equally well by ingesting either a CHO-E solution or an artificially sweetened placebo.
2.Introduction
3.Materials & Methods
3.1. Participants
3.2. Experimental Design
3.3. Experimental Procedure
3.4. Soccer Skill Tests
3.5. Fluid Intake
3.6. Preliminary Measurements, Familiarization Procedures, Diet and Training Control
3.7. Statistics
4.Results
4.1. Physical Characteristics and SST Performance
4.2. Body Mass Changes and Fluid Intake
4.3. Heart rate, Rate of Perceived Exertion (RPE), Thirst (Th), Abdominal Discomfort (AD) responses, Correlations, Temperature and Relative Humidity
5.Discussion
6.Acknowledgements
7.References
Keywords
Sports Drink; Fluid Balance; Soccer Skill; Preadolescents.
Introduction
Motion analysis studies in soccer have shown that players run at high intensity about every 70 seconds and sprint every 90 seconds while performing a number of technical skills such as passes, headings and tackles trying simultaneously to maintain control of the ball against the pressure of the opponent [36]. Under these circumstances body temperature increases even if competition takes place in a cold environment [21]. When a match is played in the heat (31°C) it has been observed that sprint, jump and high-intensity running performance are compromised especially towards the end of the game [22]. Sweat losses reported from soccer squads present a wide range of values (1.5 - 4.4 L) that is not attributable only to the variability of the weather conditions but also to the large variability in sweating responses even if measurements take place in the same training session where players perform the same training under the same environmental conditions [18, 31, 32]. So, dehydration will eventually occur despite fluid intake as a result of heat loss by evaporation in an attempt the body to limit the rise in core temperature. It has been reported that in an official soccer match over about a 3 hour period representing the arrival of the players to the soccer pitch up to the end of the game an average dehydration of about 3.4% body mass was observed as a result of a mean sweat loss of 4.4 L with individual values to be greater than 5% body mass reduction and swat losses more than 6 L [6]. Dehydration is also reported to impair performance of tasks that require cognition and skill [18]. Therefore, soccer players are advised to replace water and electrolyte losses caused as a result of their participation in the game otherwise fatigue and impaired performance of skilled tasks will occur [11]. Considering the type of fluid consumed it should be taken into account that the ingestion of plain water in large volumes will stimulate urine production due to reduction of sodium concentration and plasma osmolality [10]. During training and matches it is advisable the consumption of a drink containing some sodium [31] so that there is some degree of replacement of this electrolyte. Many studies have examine the efficacy of carbohydrate-electrolyte solutions on fluid balance and soccer skill performance or soccer simulated performance activities during training or competition in temperate, warm and hot conditions [1, 4, 9, 12, 13, 23, 27, 28, 29, 40]. However, all these studies were performed either in adults [1, 3, 4, 9, 12, 13, 23, 29, 40] or in adolescent (13-17 years) players [27, 28]. Surprisingly, to the best of the authors’ knowledge no study on fluid balance and soccer skill performance has been conducted in pre-adolescent (< 12 years) soccer players exercising in warm or hot conditions. Children, at least theoretically, may be at risk when exercising at warm and particularly in hot environment due to the fact that compared to adults possess a reduced sweating capacity, have a higher surface area to body mass ratio that may favor heat gain, produce more metabolic heat per mass unit, while demonstrate slower rate of acclimatization when exposed to high climatic heat stress [5]. The purpose of the present study was to compare the effect of a carbohydrate-electrolyte or placebo solution on fluid balance and soccer skill performance in preadolescent soccer players exercising in warm environment.
Sixteen boys 10-11 years of age participated in the present study. The participants were members of a soccer academy club and trained 3 times per week for one hour. In every training session children followed basic physical fitness exercises, practiced technical soccer skills and played in teams of 7 vs. 7. Furthermore, children participated in one match every week against other teams of similar age from other soccer academy clubs.
The parents of the participants were fully informed about the aim of the study, experimental procedures, any discomfort and possible risks involved before giving informed consent. The study had the approval of the Ethical Committee of the University.
Participants performed two identical 60 min afternoon training sessions separated by seven days. The training sessions were carried out in May, on the same day of the week and commenced at 16:00 hours. Also, the sessions were identical in content and in the order and intensity of the scheduled exercises performed. During training children drunk voluntarily every 15 min either a 6% carbohydrate-electrolyte solution (CHO-E), or placebo (P) in random order. At the end of CHO-E and P, the boys performed five soccer skill tests (SST). These tests had also been performed five days before the first trial and after children had undergone only a 10 min warm-up. Furthermore, diet and training were controlled before each training session.
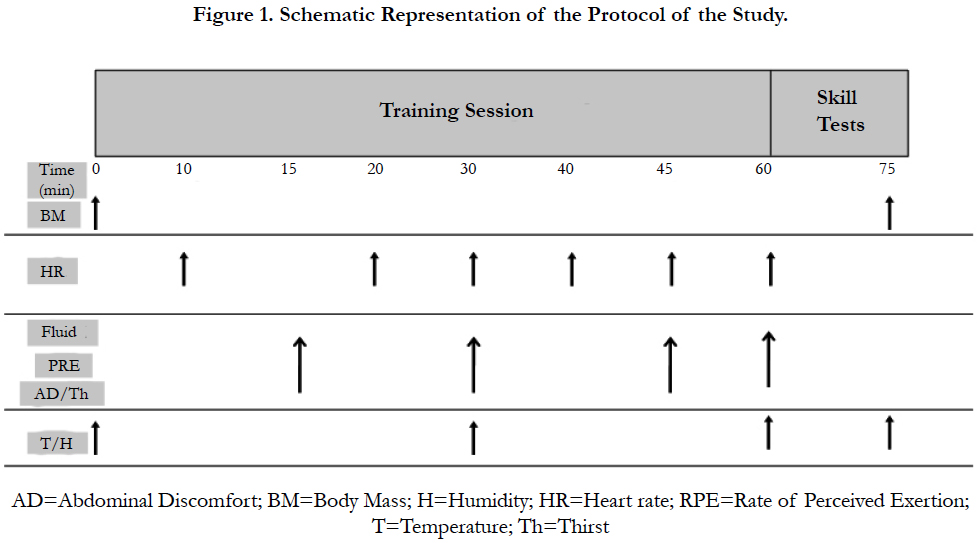
The protocol of the study is presented in Figure 1. Children arrived to the soccer academy club 20-30 min before the start of each experimental training session. In a private place each participant removed his cloths, stood still on a sensitive digital scale accurate to ± 0.02 Kg (PS 400 L BAT, Delmac Instruments, Athens, Greece) and his nude body mass was recorded by a designated experimenter who was able to see only the panel of the scale with the body mass reading. Afterwards, boys dressed their sporting gear and a heart rate (HR) monitor (Polar t2c Kempele Finland) was fitted. The dressing gear was the same in both trials. The training session started at 16:00 hours and included 10 min running for warm-up at an intensity of about 150 b.min-1, 5 min stretching exercises, 10 min juggling with the ball, 15 min technical skills including passing and receiving the ball as well as shooting and 20 min 8x8 game. At 15, 30 45 and 60 min of exercise participants were allowed for 60 sec to drink as much of the assigned fluid as they wished. Also, at the same time intervals the rate of perceived exertion (RPE) [7], abdominal discomfort (AD) and thirst (Th) were recorded. Regarding AD and Th these measurements were made using appropriate subjective scales in order to examine the level of abdominal discomfort boys may experience as a result of fluid intake during exercise (AD) and the degree of thirst (Th). Both AD and Th scales ranged from 0 (AD: "Completely comfortable"; Th: "Not thirsty at all") up to 10 (AD: "Unbearable pain"; Th: "Extremely thirsty"). Throughout exercise HR was monitored continuously. However, since the HR monitors used were not able to store and retrieve the HR data over time, at 10, 20 30, 40, 45 and 60 min each child announced the HR value on his HR monitor to a designated researcher. After completion of the 60-min training session children performed the five soccer skill tests. This procedure lasted about 15 min and afterwards the nude body mass of children was recorded as described earlier after boys carefully removing sweat with a towel. To estimate sweat loss BM loss was corrected for fluid intake and urine output according to the formula:
Sweat Loss = [(BMbefore exercise – BMafter exercise) – Urine Output] + Fluid Intake.
This calculation, however, does not take into account BM loss due to fuel oxidation and respiratory fluid losses. Nevertheless, these factors in the present study are small in magnitude and are unlikely to be different between conditions [10, 28]. Regarding urine output, it should be mentioned that although participants were allowed to urinate during exercise or SST, none of the children in any trial expressed this request. Ambient temperature and relative humidity were recorded at the beginning and at the end of exercise as well as at 30 and 60 min using a portable whirling hygrometer (Brannan, Cumbria, England). Using these data the wet bulb globe temperature (WBGT) was estimated [41]. The above procedure was carried out in exactly the same way in both CHO-E and P.
The five skill tests were the following and performed in this order: 1) ball control with the body (Sk1), 2) ball control with the head (sk2), 3) dribbling with a pass (sk3), 4) passing accuracy (sk4), and 5) shooting (sk5). These tests were performed as described in detail by Malina and colleagues [15]. The scores recorded in Sk1 and Sk2 were the number of hits of the ball before it fell to the floor, in Sk3 the score was the time in sec to complete the test, while the maximum scores in Sk4 and Sk5 were 10 and 25 respectively. These tests are recommended and traditionally used by the Portuguese Football Federation (Federação Portuguesa de Futebol 1986 cited by Malina et al. 2005 [15]), possess reasonable reliability as indicated by interclass correlation analysis (Sk1: 0.76, Sk2: 0.78, Sk3: 0.81, Sk4: 0.70, and Sk5: 70), while face validity can be assumed since these tests assess basic and important elements of soccer technique such as ball control, dribbling, passing and shooting [15].
The fluid intake was ad libitum during the 60 sec time intervals provided. Fluids were kept in a cool place (8-10°C) and provided to children in bottles of 750 ml. Each participant had two 750 ml bottles with his name and number written on it and four designated researchers were responsible each one for 4 boys to drink from the assigned bottle. After completion of the fluid intake periods every bottle was weighted using an electronic food scale (Philips Essence HR 2394 Philips, Budapest, Hungary) and the fluid consumed was recorded assuming that 1g=1ml. In CHO-E trial boys ingested a 6% commercially available carbohydrateelectrolyte solution (Gatorade, orange flavor, non-carbonated), while in the P trial boys consumed fluid that was made up of 35 ml of the CHO-E solution and 1.5 g of a sweetener (Sweet’N Low, Cumberland Packing Corporation, Brooklyn, New York , USA) per 1 liter. This provided about 14 kcal/liter and had a carbohydrate concentration of 0.3 %. The administration of the solutions was random and in a double-blind method. Ten children received the CHO-E fluid in the first while 6 received it in the second trial.
One week before the first training session boys were examined by a physician in order to assess the stage of pubic hair based on the criteria of Tanner [37]. After that assessment body mass and height were measured. Body fatness was estimated using the skinfold method. To measure the skinfolds a Harpenden skinfold caliper (Harpenden, RH15 9LB, England) was used. Triceps and calf skinfolds were measured and applied to the appropriate equation of Slaughter and colleagues [35] to estimate percentage of body fatness.
Children were familiar with the soccer skill tests performed after CHO-E and P since such exercises are used as a common practice to improve technique with the ball in soccer. However, for a period of about three weeks before the first trial, that corresponded to 8 training sessions, children practiced each soccer skill test for 3 min. Emphasis was placed in the order of performing these skill that was the same every time as described earlier. This order was used in the CHO-E and P trials as well. After the 8 training sessions boys were examined in the tests in the next training session after a 10 min warm-up that included 5 min easy jogging and 5 min stretching exercises. The time of this session corresponded to 3 days before the first trial. The performance obtained in that session was considered as “the best” performance (BestP) and was compared to the performance achieved at the end of CHO-E and P.
Participants were instructed to refrain from any training or intense physical activity the day before CHO-E and P trials as well as in the morning of the day of the main training sessions up to 16:00 hrs when experimental procedures commenced. Furthermore, instructions were given to parents and children on how to record their diet during these two days before the first experimental training session and to replicate this diet the two days before the second experimental training session.
Body mass, fluid intake and cumulative fluid intake over time, HR, RPE, Th, and AD responses were analyzed by two-way analysis of variance (ANOVA) (CHO-E/P x Time) for repeated measures with Greenhouse-Geisser correction where needed. One-way ANOVA was used to examine differences in SST performance between BestP, CHO-E and P. To account for a learning effect performance in SST was also analyzed by order (i.e: BestP vs. Trial 1 vs. Trial 2). Differences in average fluid intake, BM loss, estimated sweat loss, percent BM loss, percent BM loss corrected for fluid intake and fluid intake expressed as a percentage of BM were examined by a two-tailed paired Student’s t-test. Furthermore, Pearson correlation was used to examine relationships between fluid intake and fluid loss. To identify differences between means in the event of a significant main effect or interaction in ANOVA, simple main effects were used with Bonferroni adjustment for multiple comparisons. Effect size for main effects and interaction in ANOVA was estimated by calculating partial eta squared (ηp2), while in Student’s t-test by Cohen’s d value. Results are presented as mean and standard error of the mean (mean ± SE). Significance was set at p < 0.05 level.
Participants were 10.4 ± 0.1 years of age, Tanner stage: 2.1 ± 0.1 (range: 1.5-2.5) and their height, BM, body mass index and body fat were 1.41 ± 0.02 m, 35.20 ± 1.38 kg, 17.6 ± 0.4 kg.m-2 and 17.8 ± 1.3 % respectively.
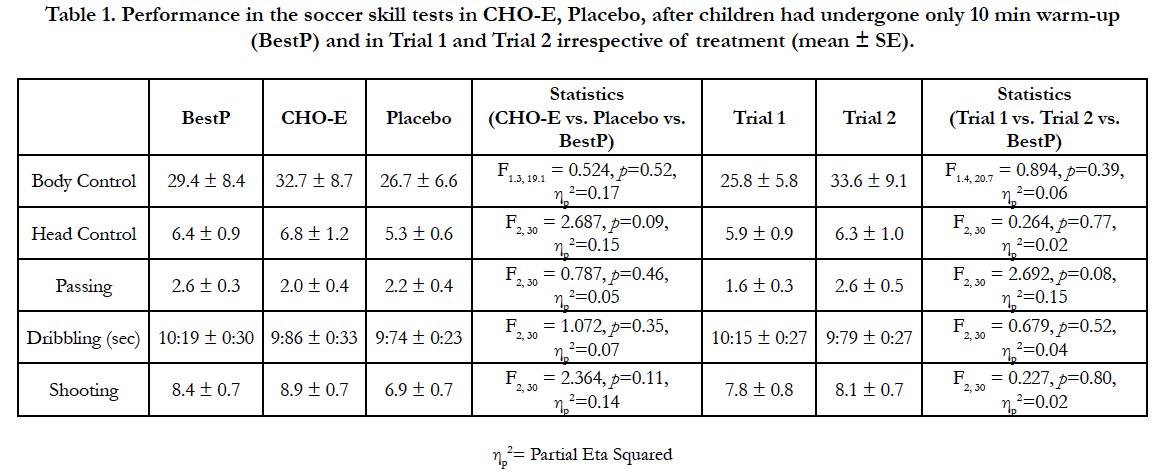
Performance in the SST after CHO-E, P, in BestP as well as irrespective of treatment (i.e. Trial 1 and Trial 2) is presented in Table 1. One-way ANOVA revealed no differences between BestP, CHO-E and P conditions in any SST either when data were analyzed by treatment (BestP vs. CHO-E vs. P) or by order (BestP vs. Trial 1 vs. Trial 2).
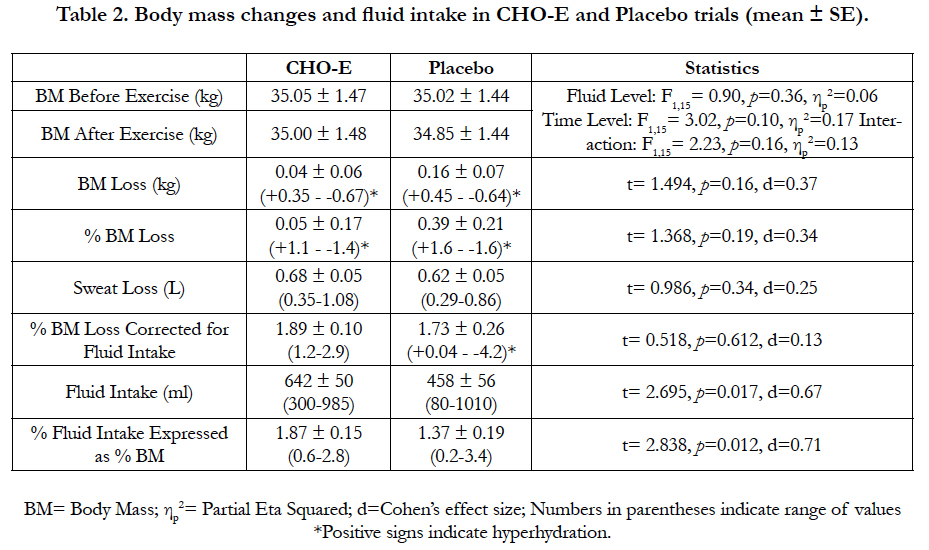
Body mass before and after exercise and BM loss in the two conditions are presented in Table 2. Body mass after exercise was not different compared to BM before exercise indicating that children maintained their BM in both CHO-E and P despite the 60 min exercise and the SST performed at 29°C. Sweat loss was similar between conditions and was about 0.6-0.7 L that corresponded to about 1.7-1.9% of BM, although there was great variability among participants (Table 2).
Table 1. Performance in the soccer skill tests in CHO-E, Placebo, after children had undergone only 10 min warm-up (BestP) and in Trial 1 and Trial 2 irrespective of treatment (mean ± SE).
Children consumed about 40% more fluid in CHO-E compared to P (p=0.017) (Table 2). This amount of fluid corresponded to about 1.9% and 1.4% of BM in CHO-E and P respectively (p=0.012, Table 2). However, there was also considerable variability in BM loss and fluid intake in both conditions as indicated by the range of values (Table 2). Fluid intake allowed children to replace their sweat losses by 95 ± 9% (range: 31-159%) and 74 ± 12% (range: 33-170%) in CHO-E and P respectively (p=0.25, d=0.30). Furthermore, in CHO-E 8 children maintained their BM and ended exercise at a hyperhydrated state, while in P this happened only with 4 participants. Nevertheless, 2 children demonstrated this maintenance of fluid balance in both conditions, whereas the other children who maintained BM achieved this only in one of the two trials (6 in CHO-E and 2 in P).
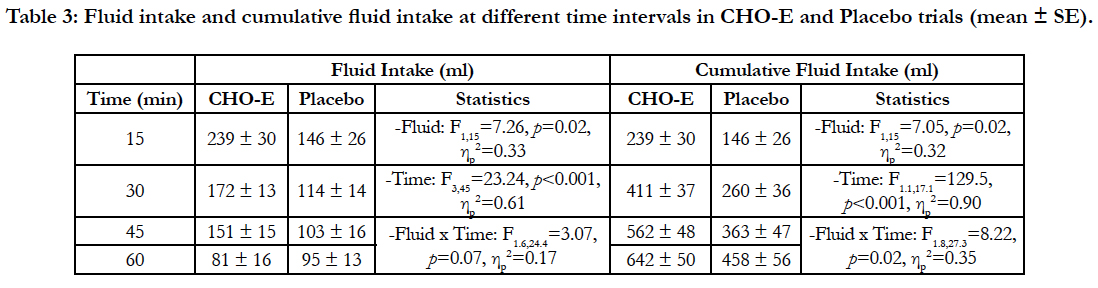
Fluid intake and cumulative fluid intake in respect to time were also different between the two conditions (Table 3). The twoway ANOVA revealed differences at Fluid and Time levels. Bonferroni post-hoc analysis in respect to time revealed that fluid was higher at 15min (239 ± 30 ml), whereas at 60 min fluid intake was the lowest (88 ± 11 ml) (p< 0.05). In cumulative fluid intake differences were found in all 3 statistical levels (Fluid, Time, and Fluid x Time). At interaction level (Fluid x Time) fluid intake was higher at 30min, 45min and 60 min in CHO-E compared to P (p< 0.05), while at Time level cumulative fluid intake got progressively higher with time (p< 0.001).
Table 3: Fluid intake and cumulative fluid intake at different time intervals in CHO-E and Placebo trials (mean ± SE).
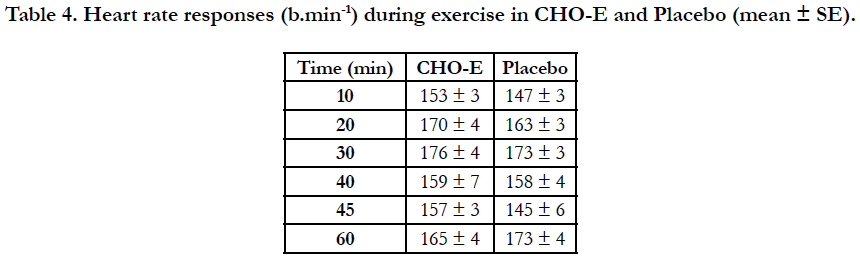
Heart rate responses (Table 4) were not different at Fluid (F1,15= 1.62, p=0.22, ηp2=0.10) and Interaction (F5,75=1.60, p=0.17, ηp2=0.10) levels, whereas there was a difference at Time level (F5,75=13.04, p=0.001, ηp2=0.47) where post-hoc analysis showed that at 10 min HR was lower (150 ± 2 b.min-1) compared to 20 min (167 ± 3 b.min-1), 30 min (175 ± 3 b.min-1) and 60 min (169 ± 3 b.min-1) (p<0.05). Mean HR during the 60 min of exercise was also similar between CHO-E (163 ± 3 b.min-1) and P (160 ± 2 b.min-1) (p=0.22).
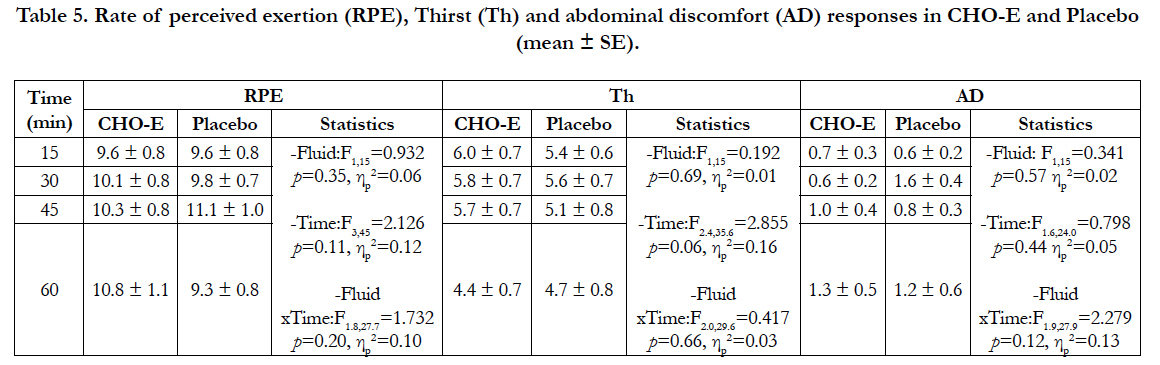
Rate of perceived exertion, Th and AD responses were not different at any statistical level (Table 5). Also, average RPE, Th and AD during exercise were similar between CHO-E (RPE: 10.2 ± 0.7; Th: 5.5 ± 0.6; AD: 0.9 ± 0.2) and P (RPE: 9.6 ± 0.6; Th: 5.2 ± 0.6; AD: 1.0 ± 0.3).
Table 5. Rate of perceived exertion (RPE), Thirst (Th) and abdominal discomfort (AD) responses in CHO-E and Placebo (mean ± SE).
Temperature in Trial 1 and 2 was 29.3°C and 29.5°C, relative humidity 42.5 % and 38.2 %, and WBGT 26.9°C and 26.7°C respectively. However, since fluids were administered in random order temperature (29.4 ± 0.0°C) and WBGT (26.8 ± 0.0°C) were the same in both CHO-E and P, whereas relative humidity (CHO-E: 40.1 ± 0.6 % vs. P: 40.6 ± 0.6 %) was also similar (p=0.63).
Sweat loss was not correlated with fluid intake in CHO-E (r= 0.12, p= 0.65), P (r=0.05, p= 0.85), or when data from the two conditions were combined (r=0.14, p = 0.44).
Discussion
The main finding of the study was that children maintained BM after exercise although they had exercised at 29°C for 60 min and had also performed the SST. Furthermore, the CHO-E drink was as effective in maintaining fluid balance and SST performance as the flavored water solution used in P.
Studies carried out in adult males during soccer matches, training, or soccer simulated activities at cool (5-8°C) [17, 19], temperate (13-24°C) [4, 23, 24, 29, 40], warm (24-29°C) [16], or hot (32- 36°C) [14, 25, 30] environment have reported sweat rates of about 1.1 L/h, 0.7-2.0 L/h, 1.4 L/h and 1.1-2.1 L/h respectively. In these studies fluid was administered either ad libitum [14, 16, 17, 19, 24, 25, 30] or prescribed [4, 23, 24, 29, 40]. When fluid was administered ad libitum, players completed exercise with a 1.1- 2.6% BM dehydration since only 38-51% of their fluid loss was replaced during exercise [14, 16,17, 19, 24, 30]. In the prescribed fluid intake investigations similar dehydration (1.3-2.5% BM) and fluid replacement (38-48%) levels have been reported [4, 23] with the exception of the study by Zeederberg and co-authors that reported 75% fluid replacement. However, when fluid intake was matched to sweat loss dehydration was minimal (0.3%) since sweat loss was replaced by about 92% [24]. Similar to adults adolescents possess great variability in fluid balance responses. In adolescent population (12-18 yrs) when soccer training or competition took place at cool (9-10°C) [8, 26], temperate (17-25°C) [8, 26-28], warm (27-29°C) [34] or hot (30-35°C) [33] environment sweat rates were reported to be about 0.3-1.0 L/h, 0.3-1.2 L/h, 0.5-0.6 L/h and 1.1-1.5 L/h respectively. When adolescent players ingested fluid in prescribed fashion dehydration was 1.5-1.6% although fluid loss was replaced by 76-84% [27, 28], whereas when fluid was provided ad libitum dehydration reported to be about 0.4-1.8% and fluid replacement 35-76% [8, 26, 33, 34]. In the present study the 10-11 year old participants had an average sweat rate of 0.62-0.68 L/h that is similar to 0.71-0.78 L/h reported for young soccer players aged 12-14 yrs exercising at temperate (18-20°C) environment [27, 28]. It is difficult to make direct comparisons between studies, however, since protocols and conditions may differ but most importantly because of the large intra-individual variability in fluid balance responses observed in all the aforementioned studies as well as in the present investigation (Table 2).
Children replaced almost all the fluid loss in CHO-E (95%) and most of this in P (74%). These levels of fluid replacement are similar to that reported for 12-14 yrs soccer players (76-84%) [27, 28] but lower for 16-18 yrs old adolescents (35-76%) exercising at cool - hot (9-33°C) conditions [8, 33, 34]. In general, from the available literature so far it seems that there is a tendency for children to replace fluid losses easier than adults. This might be because children possess a lower sweat capacity compared to adults [5] and consequently the sweat volume that has to be replaced is less.
Participants ingested 40% more fluid in CHO-E (642 ± 50 ml) compared to P (458 ± 56 ml) (p=0.017, d=0.67). The CHO-E solution, except the orange flavor that was also present in the P drink, contained carbohydrates (6%) and sodium. It should be pointed out that all children expressed their preference for the CHO-E solution. It is well known that palatability plays a key role in the fluid preference in the pediatric population. The flavoring of water together with the addition of carbohydrates and electrolytes consistently prevents voluntary dehydration in boys 9-12 yrs exercising in the heat (35°C) [38, 39]. Nevertheless, in the present study children ingested enough of the non-preferred fluid (P) to maintain BM after exercise.
Performance in SST was not different between conditions neither was an order effect (Table 1). Also, deterioration was not observed in any skill as a result of exercise when SST performance was compared in both CHO-E and P with skill performance achieved in BestP where participants had undergone only a 10 min warmup (Table 1). Probably the 60-min exercise period and the exercise intensity (160-163 b.min-1) were not intense enough to reduce children’s soccer skill ability. Several investigators have examined the effect of ingesting a carbohydrate-electrolyte solution on soccer skill performance performed after or during soccer simulated protocols [1, 3, 4, 9, 13, 23, 29, 40]. Surprisingly, all these investigations were conducted in adults (18-23 yrs). The results are equivocal since some authors have reported an improvement in skill performance with the carbohydrate-electrolyte solution [9, 13, 23], some others have observed a positive effect only in some skills such as shooting [4, 29], or others have found no effect [1, 3, 40]. Even when fluid is denied producing 2.2-2.5 % dehydration at 13-20°C soccer skill performance may [20] or may not be different [2, 24] compared to fluid provision. Therefore, since in the present study fluid balance was maintained and exercise intensity was not perceived as intense according to RPE responses (average RPE about 10 in both trials) it was expected the type of fluid to have no effect on skill performance.
No association was found between fluid loss and fluid intake (r=0.14, p=0.44). This observation has also been reported in other studies [14, 16, 17, 19, 30, 33], although Silva and colleagues reported a significant relationship during 3 consecutive days of training in adolescents (17 yrs) at 28-33°C [34].
In conclusion, pre-adolescent children 10-11 yrs maintained fluid balance and soccer skill performance equally well by ingesting either a 6% carbohydrate-electrolyte solution or an artificially sweetened placebo. Future research in preadolescents should employ longer exercise period protocols performed at a wide range of environmental conditions incorporating data on hydration status such as urine specific gravity and osmolality that were not included in the present study.
Acknowledgements
The authors wish to thank Chrysanthos Papanakos, Spiridoula Bante, and Georgios Petinis for their help in the collection of the data, Pathiakakis Soccer Academy Club for providing the necessary facilities for carrying out the study and all parents and children for their participation.
References
- Abbey EL, Rankin JW. Effect of ingesting a honey-sweetened beverage on soccer performance and exercise-induced cytokine response. Int J Sport Nutr Exerc Metab. 2009 Dec;19(6):659-672.
- Ali A, Gardiner R, Foskett A, Williams C. Fluid balance, thermoregulation and sprint and passing skill performance in female soccer players. Scand J Med Sci Sports. 2011 Jun; 21(3):437-445.
- Ali A, Williams C. Carbohydrate ingestion and soccer skill performance during prolonged intermittent exercise. J Sports Sci. 2009 Dec;27(14):1499- 508.
- Ali A, Williams C, Nicholas W, Foskett A. The influence of carbohydrateelectrolyte ingestion on soccer skill performance. Med Sci Sports Exerc. 2007 Nov;39(11):1969-1976.
- Climatic heat stress and the exercising child and adolescent. American Academy of Pediatrics. Committee on Sports Medicine and Fitness. Pediatrics. 2000 Jul;106(1 Pt 1):158-159.
- Arago΄n-Vargas LF, Moncada-Jime΄nez J, Herna΄ ndez-Elizondo J, Barrenechea A, Monge-Alvarado M. Evaluation of pre-game hydration status, heat stress, and fluid balance during professional soccer competition in the heat. Eur J Sport Sci. 2009 Aug 24; 9(5):269–276.
- Borg GA. Perceived exertion: A note on "history" and methods. Med Sci Sports. 1973;5(2):90-93.
- Broad EM, Burke LM, Cox GR, Heeley P, Riley M. Body weight changes and voluntary fluid intakes during training and competition sessions in team sports. Int J Sport Nutr. 1996 Sep;6(3):307–320.
- Currell K, Conway S, Jeukendrup AE. Carbohydrate ingestion improves performance of a new reliable test of soccer skill performance. Int J Sport Nut Exerc Metab. 2009 Feb;19 (1):34-46.
- Edwards AM, Mann ME, Marfell-Jones MJ, Rankin DM, Noakes TD, Shillington DP Influence of moderate dehydration on soccer performance: physiological responses to 45 min of outdoor match-play and the immediate subsequent performance of sport-specific and mental concentration tests. Br J Sports Med. 2007 Jun;41(6):385-391.
- Nutrition for football: The FIFA/F-MARC consensus conference. J Sports Sci. 2006 Jul; 24(7):663–664.
- Goedecke JH, White NJ, Chicktay W, Mahomed H, Durandt J, Lambert MI. The effect of carbohydrate ingestion on performance during a simulated soccer match. Nutrients. 2013 Dec;5(12):5193-5204.
- Harper LD, Stevenson ES, Rollo I, Russell M. The influence of a 12% carbohydrate-electrolyte beverage on self-paced soccer-specific exercise performance. J Sci Med Sport. 2017 Apr 21;pii:S1440-2440(17)3099-7. doi:10.1016/j.jsams.2017.04.015. Epub ahead of print.
- Kurdak SS, Shirreffs SM, Maughan RJ, Ozgunen KT, Ersoz G, Zeren C, et al. Hydration and sweating responses to hot-weather football competition. Scand J Med Sci Sports. 2010 Oct;20(Suppl 3):133–139.
- Malina RM, Cumming SP, Kontos AP, Eisenmann JC, Ribeiro B, et al. Maturity- associated variation in sport-specific skills of youth soccer players aged 13-15 years. J Sports Sci. 2005 May;23(5):515-522.
- Maughan RJ, Merson SJ, Broad NP, Shirreffs SM. Fluid and electrolyte intake and loss in elite soccer players during training. Int J Sports Nutr Exerc Metab. 2004 Jun; 14(3):333–346.
- Maughan RJ, Shirreffs SM, Merson S, Horswill CA. Fluid and electrolyte balance in elite male football (soccer) players training in a cool environment. J Sport Sci. 2005 Jan;23(1): 73–79.
- Maughan RJ, Shirreffs SM, Ozgünen KT, Kurdak SS, Ersöz G, Binnet MS, et al. Living, training and playing in the heat: challenges to the football player and strategies for coping with environmental extremes. Scand J Med Sci Sports. 2010 Oct;20(Suppl 3):117-124.
- Maughan RJ, Watson P, Evans GH, Broa N, Shirreffs SM. Water balance and salt losses in competitive football. Int J Sports Nutr Exerc Metab. 2007 Dec;17(6):583–594.
- McGregor SJ, Nicholas CW, Lakomy HKA, Williams C. The influence of intermittent high-intensity shuttle running and fluid ingestion on the performance of a soccer skill. J Sports Sci. 1999 Nov;17(11):895–903.
- Mohr M, Krustrup P, Nybo L, Nielsen JJ, Bangsbo J. Muscle temperature and sprint performance during soccer matches – beneficial effects of re-warm up at half-time. Scand J Med Sci Sports. 2004 Jun;14(3):156–162.
- Mohr M, Mujika I, Santisteban J, Randers MB, Bischoff R, Solano R, et al. Examination of fatigue development in elite soccer in a hot environment – a multi experimental approach. Scand J Med Sci Sports. 2010 Oct;20(Suppl 3):125–132.
- Ostojic SM, Mazic S. Effects of a carbohydrate-electrolyte drink on specific soccer tests and performance. J Sports Sci Med. 2002 Jun 20;1(2):47-53.
- Owen JA, Kehoe SJ, Oliver SJ. Influence of fluid intake on soccer performance in a temperate environment. J Sports Sci. 2013;31(1):1-10.
- Ozgumen KT, Kurdak SS, Maughan RJ, Zeren C, Korkmaz S, Yazici Z, et al. Effect of hot environment conditions on physical activity patterns and temperature response of football players. Scand J Med Sci Sports. 2010 Oct;20(Suppl 3):140-147.
- Phillips SM, Sykes D, Gibson N. Hydration status and fluid balance of elite European youth soccer players during consecutive training sessions. J Sports Sci Med. 2014 Dec 1;13(4):817-822.
- Phillips SM, Turner AP, Gray S, Sanderson MF, Sproule J. Ingesting a 6% carbohydrate-electrolyte solution improves endurance capacity, but not sprint performance, during intermittent, high-intensity shuttle running in adolescent team games players aged 12-14 years. Eur J Appl Physiol. 2010 Jul;109(5):811-821.
- Phillips SM, Turner AP, Sanderson MF, Sproule J. Beverage carbohydrate concentration influences the intermittent endurance capacity of adolescent team games players during prolonged intermittent running. Eur J Appl Physiol. 2012 Mar;112(3):1107-1116.
- Russell M, Benton D, Kingsley M. Influence of carbohydrate supplementation on skill performance during a soccer match simulation. J Sci Med Sport. 2012 Jul;15(4):348-354.
- Shirreffs SM, Aragon-Vargas LF, Chamorro M, Maughan RJ, Serratosa L, Zachwieia JJ. The sweating response of elite professional soccer players to training in the heat. Int J Sports Med. 2005 Mar;26(2):90-95.
- Shirreffs SM. Hydration: special issues for playing football in warm and hot environments. Scand J Med Sci Sports. 2010 Oct;20(Suppl 3):90–94.
- Shirreffs SM, Sawka MN, Stone M. Water and electrolyte needs for football training and match-play. J Sports Sci. 2006 Jul;24(7):699–707.
- Silva RP, Mundel T, Natali AJ, Bara Filho MG, Alfenas RC, Lima JR, et al. Pre-game hydration status, sweat loss, and fluid intake in elite Brazilian young male players during competition. J Sports Sci. 2012;30(1):37-42.
- Silva RP, Mundel T, Natali AJ, Bara Filho MG, Lima JR, Lopes PR, et al. Fluid balance of elite Brazilian youth soccer players during consecutive days of training. J Sports Sci. 2011Apr;29(7):725–732.
- Slaughter MH, Lohman TG, Boilleau RA, Horswill CA, Stillman RJ, Van Loan MD, et al. Skinfold equations for estimation of body fatness in children and youth. Hum Biol. 1988 Oct;60(5):709-723.
- Stolen T, Chamari K, Castagna C, Wisloff U. Physiology of soccer. An update. Sports Med. 2005;35(6):501–536.
- Tanner JM. Growth at adolescence; with a general consideration of the effects of hereditary and environmental factors upon growth and maturation from birth maturity. 2nd ed. Oxford: Blackwell; 1962.
- Wilk B, Bar-Or O. Effect of drink flavor and NaCl on voluntary drinking and hydration in boys exercising in the heat. J Appl Physiol. 1996 Apr;80(4):1112-1117.
- Wilk B, Kriemler S, Keller H, Bar-Or O. Consistency in preventing voluntary dehydration in boys who drink a flavored carbohydrate-NaCl beverage during exercise in the heat. Int J Sport Nutr. 1998 Mar;8(1):1-9.
- Zeederberg C, Leach L, Lambert EV, Noakes TD, Dennis SC, Hawley JA. The effect of carbohydrate ingestion on the motor skill proficiency of soccer players. Int J Sport Nutr. 1996 Dec;6(4):348-355.
- Zunis Foundation. Heat Stress Adviser: A Program For Palm-Type PDA’s. Avaliable from http://www.zunis.org/sports_p.htm