Child Erysipelas: About 16 Pediatric Cases
Lahlou Asmae*, Douhi Zakia, Gallouj Salim, Baybay Hanane, Mernissi Fatimazohra
University Hospital Hassan II, Dermatology Department; Fez; Morocco.
*Corresponding Author
Asmae Lahlou,
University Hospital Hassan II, Dermatology Department, Fez, Morocco.
E-mail: lahlouasmae@gmail.com
Received: October 18, 2016; Accepted: March 23, 2017; Published: March 27, 2017
Citation: Lahlou Asmae, Douhi Zakia, Gallouj Salim, Baybay Hanane, Mernissi Fatimazohra (2017) Child Erysipelas: About 16 Pediatric Cases. Int J Pediat Health Care Adv. 4(2), 31-33. doi: dx.doi.org/10.19070/2572-7354-1700010
Copyright: Lahlou A© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Erysipelas is an acute or sub-acute non necrotizing bacterial dermo-hypodermitis , caused most frequently by beta-hemolytic group A streptococci. It is a relatively frequent pathology in adults and the elderly, but rare in children and infants. Through the analysis of 16 cases of pediatric erysipelas we evaluate the epidemiological, clinico-biological, therapeutic and outcomes characteristics of erysipelas in children and infants.
2.Introduction
3.Objective of the Study
4.Material and Methods
5.Results
6.Discussion
7.Conclusion
8.References
Keywords
Erysipelas; Dermo-Hypodermitis; Beta-Hemolytic Group A Streptococci.
Introduction
Erysipelas is an acute or sub-acute non necrotizing bacterial dermo-hypodermitis, caused most frequently by beta-hemolytic group A streptococci. It is a relatively frequent pathology in adults and the elderly, but rare in children and infants.
Objective of the Study
Evaluate the epidemiological, clinico-biological, therapeutic and outcomes characteristics of erysipelas in children and infants.
Material and Methods
Study conducted in the dermatology ward University Hospital Hassan II FEZ, In collaboration with pediatricians over a 4 years period from June 2012 to June 2016. We had studied 16 cases of erysipelas, hospitalized in the pediatric ward and pediatric emergency room.
Results
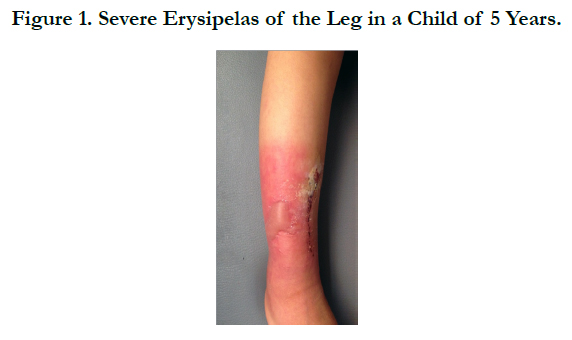
Of the 16 cases studied, 6 were boys and 10 were girls, with median age of 5.5 years (range 4 months -15 years). 25% had an age of less than 2 years. No previous history of erysipelas was noted. The median time to consultation was 3 days. The general condition was conserved in all the cases, but one patient was malnourished. Fever was present in 75% of the cases; however the erythematous plaque which is feature of erysipelas was present in all the cases. It was a simple dermo-hypodermitis in 15 cases. Complicated by an abscess of the soft parts in one case. Preferential location was the lower body, in particular the legs in 62.5% of the cases, followed by the arms 25%, then the face 12.5%. Satellite inflammatory lymph nodes were present in 56.2 % of the cases. The entry location was found in 75% of the cases: 6 skin cuts, 4 scratches and one toe intertrigo, one case of insect bite and one case of furuncle, one case of venous ulcer, and two cases of impetigo. A biological inflammatory syndrome with elevation of leukocytes with neutrophil predominance was constantly found. The ultrasound of the soft parts, realized in 5 patients, had objectified an abcess in 1 case. Pediatric surgical consult and standard x-rays were performed in 4 cases to rule out osteomyelitis. Articulation ultrasound to rule out osteoarthritis was not performed in any patient. 15 of the patients were treated by Amoxicillin-clavulinic acid combination at the dose of 50 mg/kg/day, one patient was treated by Phenoxymethylpenicillin (penicillin V). In addition to treatment of the entry wound fever was subsided after 48 hours of treatment. The median duration of hospitalization was 3 days (range 2 to 6 days). Good amelioration was observed in the 48h following the start of the treatment, with a total of 3 weeks of treatment.
Discussion
Erysipelas is a beta-hemolytic streptococcal infection that affects the skin and subcutaneous tissue. The infecting organism usually enters the body through nasopharyngeal tissue, trauma sites, insect bites or surgical incisions [1].
Erysipelas involves the more superficial layers of the skin and cutaneous lymphatics. In typical erysipelas, the area of inflammation is raised above the surrounding skin, and there is a distinct demarcation between involved and normal skin. Although the older literature indicates the face as the typical site of erysipelas, up to 85 percent of cases now occur on the legs and feet [2]. Blood cultures are positive for the pathogen in only about 5 percent of cases. The great majority of cases are due to group A streptococci, but erysipelas may also be caused by streptococci of groups G, C, and B [3] and, rarely, by staphylococci [2].
Bacterial skin infections, in particular the superficial infections with pyogenes are a frequent occurrence in children. Erysipelas on the contrary is rare. Erysipelas affects persons of all ages, but it is most prevalent among the young and the elderly [2]. It affects children with a median age of 5 years old, like in our series, but should also be suspected in infants, since 25% of our patients had an age less than 2 years old.
According to the Tunisian series by Kacem and al, the preferred location of erisypelas in children is the lower limb, as in our series.
The differential diagnosis of child erysipelas is osteomyelitis and osteoarthritis that are better diagnosed by pediatricians and pediatric surgeons.
The evolution is often benign, nevertheless, severe complications can occur as an evolution of this dermo-hypodermitis, in particular abscess and necrotic fasciitis [4], The general complications are exceptional [5-7]; drug eruptions to penicillin are the most frequent: 5%; rare cases of septicemia are described [8]; decomposition of underlying diseases are always to be feared [6]. We have had a case of abscess in one child in whom the diagnosis was made on the 6th day.
Conclusion
Erysipelas diagnosis is clinical, but sometimes it is difficult to distinguish between the multiple differential diagnoses (osteomyelitis, osteoarthritis, malignant staphylococcal infection, necrotic fasciitis, cellulites) due to the frequency of incomplete clinical presentations in children and infants. Creating awareness among pediatricians and pediatric surgeons is necessary for an early treatment.
References
- Bratton RL, Nesse RE (1995) St Anthony's Fire: diagnosis and management of erysipelas. Am Fam Phys. 51(2): 401-4.
- Chartier C, Grosshans E (1990) Erysipelas Int J Dermatol. 29(7): 459-67.
- Binnick AN, Klein RB, Baughman RD (1980) Recurrent erysipelas caused by group B streptococcus organisms. Arch Dermatol. 116 (7): 798-9.
- Bartter T, Dascal A, Carroll K, Curley FJ (1988) 'Toxic strep syndrome.' A manifestation of group A streptococcal infection. Arch Intern Med. 148(6): 1421-1424.
- Jorup-Ronstrom C (1986) Epidemiological, bacteriological and complicating features of erysipelas. Scand J Infect Dis. 18(6): 519-24.
- Noblesse I, Carvalho P, Young P, Hellot MF, Levesque H, et al., (1999) Facteurs de gravité des érysipèles de jambe. Ann Dermatol Venereol 1999;126 (suppl 2): S65.
- Cone LA, Woodard D, Schlievert PM,Tomory GS (1987) Clinical and bacteriologic observations of a toxic skock-like syndrome due to Streptococcus pyogenes. N Engl J Med. 317(3): 146-9.
- Crickx B, Chevron F, Sigal-Nahum M, Bilet S, Faucher F, et al., (1991) Erysipele: donnees epidemiologiques cliniques et therapeutiques, Ann Dennatol Venereol. 118: 11-6.