Infantile Colic, Is there an Association with the Source of Early Infant Nutrition?
Abdelrazak Ali1,*, Mohamed Abdeltawab Mahmoud2, Emad Ghaly3
1 Assistant Professor of Pediatrics, Al-Azhar University, Cairo, Egypt.
2 Consultant of Hospital management and Medical Quality Control, Ministry of health, Egypt.
*Corresponding Author
Abdelrazak Mansour Ali,
Department of Pediatrics, Al-Azhar University, Cairo, Egypt.
Tel: 15713317055
E-mail: abdelrazak_ali@yahoo.com
Received: December 09, 2016; Accepted: January 06, 2017; Published: January 09, 2017
Citation: Abdelrazak Ali, Mohamed Abdeltawab Mahmoud, Emad Ghaly (2017) Infantile Colic, Is there an Association with the Source of Early Infant Nutrition?. Int J Pediat Health Care Adv. 4(1), 24-28. doi: dx.doi.org/10.19070/2572-7354-170008
Copyright: Abdelrazak Ali© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To determine whether breastfeeding has an impact on colic development.
Design: A prospective cohort study of 436 mother-infant dyads who give birth at term to alive singleton whose birth weight was appropriate for gestational age. Self-administered questionnaires to mothers at 1 and 6 weeks postpartum, requested information on many infant and maternal factors, including source of infant nutrition (exclusively breast fed, complementary fed and exclusively formula fed). Cases of colic were identified by applying modified Wessel criteria or by interpreting the response to the Ames cry score.
Results: Of 536 mothers, 436 (81%) completed the study. Overall the prevalence of colic at 6 weeks of age was 23.6%. No association was seen between the source of infant nutrition and colic. Higher levels of maternal trait anxiety were associated with increased likelihood of colic after controlling for feeding method, maternal age, and parity although the difference failed to reach significance. No significant difference was seen between employed and unemployed mothers, but some difference was seen between both employed and unemployed mothers in one side and the student mothers in the other side, although the difference was statistically insignificant.
Conclusion: Breast feeding did not have a protective effect on the development of colic. Although colic was statistically associated with some variables, including pre-existing maternal anxiety and student mothers, some of colic’s etiology remains unexplained despite the numerous studies done in this field.
2.Material and Method
3.Results
3.1. Factors associated with the development of colic at 6 weeks of age
4.Comment
4.1. What Does This Study Add?
5.References
Keywords
Genital Dermatosis; Children; External Genital Organs.
Introduction
The most frequently accepted definition of colic is that of Wessel of a well thriving infant who has paroxysms of crying lasting for three hours per day for more than three days a week for longer than three weeks [1]. Schmitt suggested the practical definition of “colic as an intermittent unexplained crying during the first three months that reaches a point where parents complain about it and starts before 2 weeks of age and usually stops by 3-4 months of age, it is not the result of bad parenting, nor caused by too much gas [2]. Colic’s onset usually occurs between the 2nd and 6th weeks of life and its disappearance around 3 months. Its prevalence ranges from 5% to 40% depending on the definition and methods used. It remains enigmatic, despite its relatively frequent occurrence. While apparently innocuous, an infant colic can prompt lasting parental distress [3-5]. Gastrointestinal causes [6-8], psychological causes [9-11] and hormonal factors “increase production of serotonin unopposed by the production of melatonin” [11-13] have been suggested for the colic’s development. Other investigators found the correlation between infant colic and allergic products of food and advised the use of hypoallergenic formula in the management of some cases of infant colic [14-16]. An interview of literature, doctors who study colic, have interesting observations: Colicky infants have an increased amount of the hormone motilin in their blood which stimulates gastrointestinal tract to cause cramping [17]. Colicky infants have abnormal contractility of the gallbladder and have increased intestinal permeability [18]. Recently, the composition of intestinal microflora has been attributed as an independent risk factor for colic. Studies indicate that inadequate amounts of lactobacillus and increased amounts of coliform bacteria like E coli, Klebsiellosis and anaerobes in the intestine may influence gut motor function and gas production which subsequently contributes to the occurrence of colic [19]. Replacing microflora with probiotic was found to have remarkable improvement and less crying episodes [20]. More recently, the cause of infant colic was uncovered and attributed to Helicobacter pylori infection [21]. The crying of a colicky infant has typical pattern described as loud continuous high pitched cry. It may be accompanied by tensing of the abdominal muscles, flexing the legs, flushing of the face, cold feet, clenching fingers and passing gases. The peak period of crying usually occurs at evening. The attack may terminate when the infant is completely exhausted or with the passage of flatus [18]. Mothers of excessively crying infants experience high levels of depression, and fathers’ depression during the postpartum period is highly correlated with mother depression. Furthermore, depression in fathers during the postpartum period has deleterious effects on infant and child outcomes as the depressed fathers have less optimal interactions with their infants [22].
Material and Method
Approval of this study was received from the administration of Armed Forces Hospital in Najran, Saudi Arabia. The study was a prospective cohort study of mother-infant dyads. A selfadministered questionnaire to mothers at one and six weeks postpartum including, maternal health behaviors, demographic variables, biological factors and the current source of infant nutrition (exclusive breastfed, complementary fed and exclusively formula-fed). Infants who received any quantity of non-human milk along with breast milk were defined as complementary fed. Standardized measures that assessed maternal anxiety, postnatal depression and social support [23, 24] were incorporated into the first questionnaire because these constructs have been suspected to play a role in colic’s development. The psychometric properties of the state-trait anxiety inventory are well established. So, this scale was used in this study. The state-trait anxiety inventory is composed of 2 scales that measure 2 distinct anxiety concepts: state anxiety and trait anxiety. The trait scale asks participants how they generally feed and is indicative of anxiety proneness [25, 26]. The state anxiety asks participants how they currently feel and sensitivity indicates participant’s levels of transitory anxiety. Possible scores range from 20-80 on each scale [27, 28]. Cases of colic were identified as those infants whose cry/ fuss behaviors fulfilled modified Wessel criteria. For this study, a colicky infant was defined as one who was otherwise healthy and well fed, but who had paroxysms of irritability, fussing, or crying lasting for three or more hours in any one day and occurring on three or more days in any week. Mothers were also asked to complete a short questionnaire based instrument, the Ames cry score, which is composed of three questions, each with four response categories that are scored from 0-3. It asks about the frequency, average and maximum duration of an infant’s cries during the past week. Overall scores, calculated by summing the scores of individual items, range from 0-9, with a score of 3 or greater indicating colic. The overall prevalence of colic at 6 weeks of age was calculated among exclusively breast fed, exclusively formula fed and complementary fed infants. A questionnaire was mailed to mothers approximately one week after they were discharged from the hospital. Another questionnaire was mailed to the mothers at six weeks and four months after delivery. For all analyses, the exposure variable was the source of infant nutrition at one week postpartum, while the outcome was the colic defined at 6 weeks postpartum. This approach addressed one of the shortcomings of earlier works because it permitted an examination of the potential temporal relationship between the source of infant nutrition and colic’s development.
Results
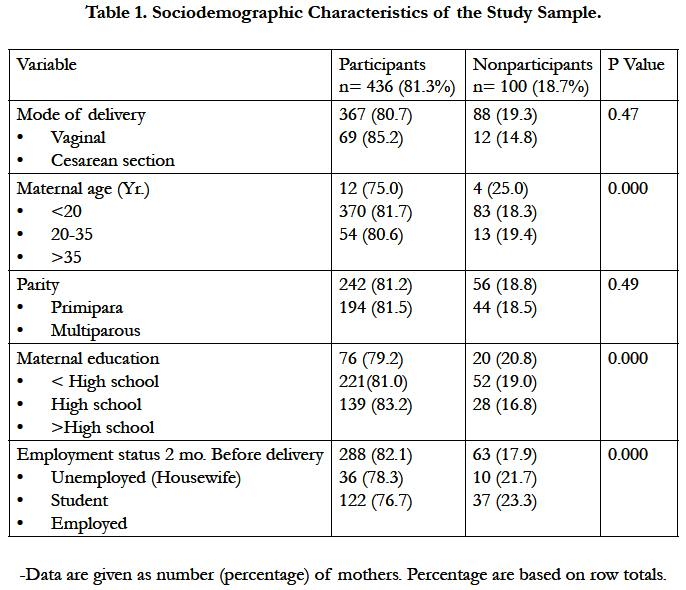
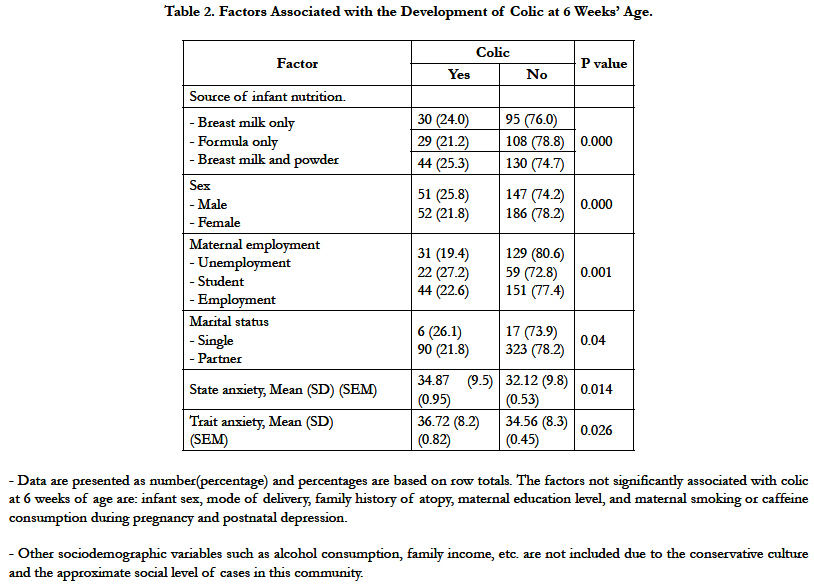
Eligible cases were approached between November 2013 and October 2014. About 68% of participants were breast feeding their infants at 6 weeks postpartum. Only 81% of cases completed the study at 6 weeks postpartum (Table 1). Overall the prevalence of colic was 23.6% when examined separately. The prevalence of colic based on the interpretation derived from the Ames Cry Score was 22%. The mean amount of crying/fussing recorded during an infant sixth weeks of life was more than 10 hours (SD= 6.1 hrs.) while this is 1.5 hr./day. The prevalence of colic among exclusively breast fed, exclusively formula fed and complementary fed infants was 24%, 21% and 25% respectively (Table 2). There was no statistically significant relationship between the source of early infant nutrition, measured at one week postpartum and the development of colic at 6 weeks postpartum. In the 436 motherinfant dyads participating in the study at 4 months, 17 infants (3.9%) had colic at 4 months of age, compared with 103 infants (23.6%) who had colic at six weeks of age. The mothers of infants who had colic at six weeks of age did not have significant differences in rates of anxiety and depression, compared with the mothers of infants who did not have colic.
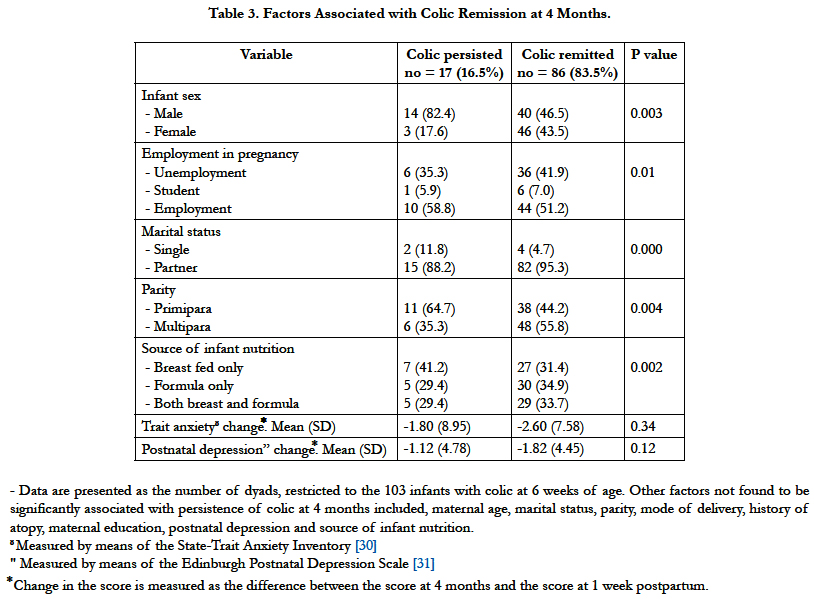
If a mother was employed or attended school full-time before being delivered of an infant, her infant was significantly more likely to exhibit colic. Infants born to mothers who were married or had a common-law partner were less likely to exhibit colic, relative to infants born to single mothers. Elevated levels of postnatal depression also seemed associative with colic's development, but this association failed to reach statistical significance. At 4 months of age, colic persisted in 16.5% of cases. Additionally, the trait anxiety score and the postnatal depression score changed at 4 months of age, compared to the basal scores at one week postpartum(Table 3). Because pacifier use was expected to affect breastfeeding and infant cry/fuss behavior, we considered it as a potential confounder. However, the evidence that pacifier use does not markedly affect the daily duration of cry/fuss behavior [29], prompted our decision not to include pacifier use in the multivariate model.
Comment
Despite using prospective methods, an objective case definition, a population-based relatively large sample and multivariate techniques, our results failed to document any relationship between the source of early infant nutrition and colic's development. Unlike other studies, potential etiologic agents including the source of infant nutrition and levels of maternal distress were assessed before the development of colic, allowing for the exploration of temporal relationships. Additionally, the study provides evidence that most cases of infant colic remit by 4 months with little lasting impact on the levels of maternal anxiety or depression Admittedly, because the participants in our study were, on average, well educated, our findings may not generalize to populations that differ in their socioeconomic background and/or access to health care. Nevertheless, the internal validity of our study is high because of the inclusive nature of the study population, the representative sample, and the high response rates. This internal validity lends support to our conclusion that, in most cases, recommendations to alter an infant's diet in the hope of ameliorating colic are not logically established. Moreover, we examined the potential for an episode of colic to adversely affect maternal mental health after controlling for earlier pre-colic levels of anxiety and depression. Elevated levels of maternal anxiety have received considerable attention as a contributing factor in colic's development [32-34]. Elevated levels of maternal trait anxiety, measured at 1 week postpartum, predicted colicky behavior at 6 weeks; however, this finding failed to reach statistical significance. Our results suggest that about 1 in 4 infants experienced colic at 6 weeks of age. The collection of cry/fuss data at this point of time was expected to capture most cases of colic because the sixth week of life represents the peak of infant crying [35]. Our results document no any relationship between the source of early infant nutrition and colic's development. The absence of a protective effect of breastfeeding on colic's development is firmly considered across time, geography, and study design [36-40]. The assumption that infantile colic is developmental, psycho-biological problem (i.e. developmental sleep disorder) suggested by some investigators [41], is not an evidence-based theory, and their study designed to test the hypothesis that kangaroo care is more effective than conventional care on infantile colic. Moreover, their work was conducted on preterm infants. In this model, colic is viewed as a delay or disturbance in the biorhythmic organization of the infant and colicky infant becomes overly stimulated and overly tired and is less able to initiate a downward shift in the state from awake and crying to a sleep state. This recurrent cycle is theorized to affect the overall interact total synchrony of the mother-infant dyad.
Although continued uncertainty about colic's etiology may be viewed in a negative light, our findings should provide comfort to parents as we provide further evidence that parents are not responsible for their infants' colic. Of course, much work remains to be done to improve our understanding of the underlying processes responsible for colic and to minimize their potential effects on families. Colic's relatively frequent occurrence and potential sequelae command our continued attention. Thus, the author novel finding of “Helicobacter pylori might be the causative agent of infant colic” is a clearly relevant work of attention. Further research needs to determine an optimal manner for identifying infants who are at an elevated risk of state regulatory functional disorders.
Infant colic is a relatively common condition, characterized by excessive and inconsolable crying as formerly estimated. Some have suggested that food intolerance is to blame but this has limited confidence. Because numerous intervention strategies are based on dietary incompatibility theories, there is a need to determine whether this focus is justified. By using prospective methods in a community sample of infants, this study addressed many of the methodological issues of previous works. In doing so, the study provided evidence that about 1 in 4 infants exhibited colicky behavior at 6 weeks of age, suggested that breastfeeding was not protective in colic's development, and although colic was statistically associated with several factors, including preexisting maternal anxiety, the clinical importance of this finding is limited. So, while the origins of colic remain a mystery, its clinical salience cannot be questioned. This stimulates recalling other related functional disorders that are commonly occurring (i.e. recurrent abdominal pain of childhood and irritable bowel syndrome of adolescence). This underlies the importance of continued research particularly in the field of molecular genetic approach. The future studies should be centered and directed to the genetic basis of these interrelated functional disorders.
References
- Wessel MA, Cobb JC, Jackson EB, Harris GS, Detwiler AC (1954) Paroxysmal fussing in infancy sometimes called "colic". Pediatrics. 14(5): 421-34.
- BD Schmitt (2011) My Child Is Sick. American Academy of Pediatrics Books.
- Lucas Sen PL, Assendelft WJ, Van Eijk JT, JW Gubbels, AC Douwes, et al., (2001) Systemic review of the occurrence of infant colic in the community. Arch Dis Child. 84: 398-403.
- Sijmen A Reijneveld, Emily Brugman, Remy A Hirasing (2001) Excessive Infant Crying: The Impact of Varying Definitions. pediatrics. 108( 4): 893- 7.
- David R Fleisher (2014) Management of Functional Gastrointestinal Disorders in children. Springer, berlin : Germany.
- Christian Nordqvist (2016) Pediatrics/children’s health Colic: Causes, Symptoms, and Treatments. In Medical News.
- Shamir Raanan, St James-Robert Ian, Di Lorenzo Carlo, Burns Alan J, Thapar Nikhil, et al., (2013) Infant crying, colic, and gastrointestinal discomfort in early childhood: a review of the evidence and most plausible mechanisms. J Pediatr Gastroenterology Nutr. 57(1): S1–45.
- Lothe L, Lindberg T (1989) Cow’s milk whey protein elicits symptoms of infant colic in colicky formula-fed infants: a double- blind crossover study. Pediatrics. 83(2): 262-266.
- Fiona K, Vincent R, Emma F (2011) The psychology of infant colic: A review of current research. Infant Mental Health J. Vol. 32(5): 526–541. DOI:10.1002/imhj.20308.
- Roberts DM, Ostapchuk M, O'Brien JG (2004) Infantile colic. American family physician (Review). 70(4): 735–40.
- Sumitha Nayak (2014) Infantile Colic--Do we understand the etiology? Pediatrics on-call J. 11(1). DOI: 10.7199/ped.oncall.2014.19.
- F Savino V, Tarasco (2010) New treatments for infant colic. Current Opinion in Pediatrics: General pediatrics. 22(6): 791.
- Francesco Savino (2007) Focus on infantile colic. Acta Pediatrica. 96(9): 1259-64. DOI: 10.1111/j.1651-2227.2007.00428.
- David J Hill, Neil Roy, Ralf G Heine, Clifford S Hosking, Brown J, et al., (2005) Effect of a Low-Allergen Maternal Diet on Colic Among Breastfed Infants: A Randomized, Controlled Trial. Pediatrics. 116(5): e709-15.
- Jatinder Bhatia, Frank Greer (2008) Use of Soy Protein-Based Formulas in Infant Feeding; Pediatrics. 121(5): 1062-8.
- Marina Iacovo, Robin A Ralston, Jane Muir, Walker KZ, Truby H (2012) Dietary Management of Infantile Colic: A Systematic Review. Matern Child Health J. 16(6): 1319-1331.
- Telmesani AMA, Khan MN (2016) Infantile Colic - A Challenge to Parenthood. Int J Community Fam Med. 1: 109.
- Lehtonen L, Svedström E, Korvenranta H (1994) Gallbladder hypocontractility in infantile colic. Acta Paediatr. 83(11): 1174-7.
- Gupta SK (2002) Is colic a gastrointestinal disorder? Curr Opin Pediatr. 14(5): 588-592.
- Savino F, Cordisco L, Tarasco V, Palumeri E, Calabrese R, et al., (2010) Lactobacillus: Lactobacillus reuteri DSM 17938 in Infantile Colic: A randomized, Double-Blind, Placebo-Controlled Trial. Pediatrics. 126(3): e526-e533.
- Abdelrazak Mansour Ali (2012) Helicobacter pylori and Infantile Colic. Arch Pediatr Adolesc Med. 166(7): 648-650.
- Katch Leslie (2012) The Relationship Between Infant Crying and Father Well-Being. Dissertations, Paper 306.
- Guido HE Gendolla, Mattie Tops, Sander L Koole (2014) Perinatal developmental origins of self-regulation. In Handbook of behavioral approaches to self-regulation. Springer, New York Heidelberg, London.
- John R Britton (2011) Infant Temperament and Maternal Anxiety and Depressed Mood in the Early Postpartum Period. J Women Health. 51(1): 55-71.
- Balsamo M, Romanelli R, Innamorati M, Ciccarese Gabriele, Carlucci Leonardo, et al., (2013) The State –Trait Anxiety Inventory: Shadows and Lights on its Construct Validity. J Psychopathological Behavioral Assess. 35:475. doi:10.1007/s10862-013-9354-5.
- Julian Laura J (2016) Measures of Anxiety. Arthritis care res. 63(0 11) : 10.1002/acr.20561.
- White David J, de Klerk S, Woods W, Gondalia S, Noonan C, et al., (2016) Anti-Stress, Behavioral and Magnetoencephalography Effects of an L-Theanine-Based Nutrient Drink: A randomized, Double-Blind, Placebo-Controlled, Crossover Trial. Nutrients. 8(1): 53.
- Chang Yu-San, Wu YH, Su SF, Hsu CY, Chen HL (2013) Factors related with the ability to maintain wakefulness in the daytime after fast and forward rotating shifts. Kaohsiung J Med Sci. 29(11): 611 – 616.
- Kramer MS, Barr RG, Dagenais S, Yang H, Jones P, et al., (2001) Pacifier use, early weaning, and cry/fuss behavior: a randomized controlled trial. JAMA. 286(3): 322-6.
- Spielberger CD, Gorsuch RL, LuscheneR (1970) The State-Trait Anxiety Inventory. Palo Alto, Calif Consulting Psychologists Press.
- Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry.150: 782- 786.
- Rautav PH, H Helenius, Lehtonen L (1993) Psychosocial predisposing factors for infantile colic. BMJ. 307(6904): 600- 604.
- Carey WB (1968) Maternal anxiety and infantile colic: is there a relationship? Clin Pediatr (Phil). 7(10): 590- 595.
- Miller AR, Barr RG, Eaton WO (1993) Crying and motor behavior of sixweek- old infants and postpartum maternal mood. Pediatrics. 92(4): 551- 558.
- Barr RG, Roman A, Yaremko J, Leduc D, Fran Coeur TE (1992) The crying of infants with colic: a controlled empirical description. Pediatrics. 90(1): 14- 21.
- Forsyth BW, Leventhal JM, McCathy PL (1985) Mothers' perceptions of problems of feeding and crying behaviors. A prospective study. Am J Dis Child. 139(3): 269- 272.
- Singer JL, Rosenberg NM( 1992) A fatal case of colic. Pediatric Emergency Care. 8(3): 171- 172.
- Ames E Bradley C (1983) Infant and parent characteristics related to parents' reports of colic in one-month-old and three-month-old infants. Paper presented at Canadian Psychological Association Meeting, Winnipeg, Manitoba.
- Canivet C, Hag Ander B, Jakobsson I, Lanke J (1996) Infantile colic: less common than previously estimated? Acta Pediatrica. 85(4): 454- 458.
- Lucas A, St James–Roberts I (1998) Crying, fussing and colic behavior in breast- and bottle-fed infants. Early Hum Dev. 53(1): 9- 18.
- Reza Saeidi, Maryam Zaidi Abadi, Abolghasem, Mahbobeh Ghaolami (2014) The effectiveness of Mother infant Interaction on infantile colic. IJN. 4(4): 37-38.