Childhood Genital Dermatosis
Elloudi S*, Lahlou A, Lakjiri S, Baybay H, Gallouj S, Mernissi FZ
1 Programa de Pós Graduação em Saúde da Criança e do Adolescente, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brasil.
2 Centro de Estudos em Alimentação e Nutrição (CESAN), Hospital (PPGSCA) de Clínicas de Porto Alegre- Universidade federal do Rio Grande do
Sul, Porto Alegre, RS, Brasil.
3 Unidade de Neuropediatria, Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brasil.
4 Programa de Pós Graduação em Saúde Coletiva, Universidade do Extremo Sul Catarinense, Criciúma, SC, Brasil.
*Corresponding Author
Sara Elloudi,
Department of Dermatology and Venereology,
University Hospital Hassan II Fez, Morocco.
Tel: 212- 0667410849
E-mail: saraelloudi@gmail.com
Received: November 19, 2016; Accepted: December 14, 2016; Published: December 16, 2016
Citation: Elloudi S, Lahlou A, Lakjiri S, Baybay H, Gallouj S, et al., (2016) Childhood Genital Dermatosis. Int J Pediat Health Care Adv. 3(3), 21-23. doi: dx.doi.org/10.19070/2572-7354-160007
Copyright:Elloudi S© 2016. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Genital dermatology studies the cutaneous mucosal dermatosis of the external genital organs. We carried out a descriptive study involving 100 children consulting for genital symptomatology. Different pathologies have been found in our patients. In children, regardless of age, all inflammatory or other dermatological diseases may have a genital location. In most cases, it is integrated into a generalized dermatosis, and in this case the remote lesion can make the diagnosis.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.References
Keywords
Genital Dermatosis; Children; External Genital Organs.
Introduction
Genital dermatology studies the cutaneous mucosal dermatosis of the external genital organs (EGO). This pathology is very varied and most of the etiologies remain favorable prognostic. The objective of this study was to describe the epidemiological and clinical profile of dermatoses of EGO affecting children in the Department of Dermatology of University Hospital Hassan II of FEZ.
Materials and Methods
This is a descriptive study which allowed to collect all the cases of genital dermatoses affecting the children recruited in our department of dermatology covering a period of 3 years from January 2013 to January 2016. The criteria of inclusion were all children Presenting in consultation of dermatology for a genital symptomatology.
Result
A total of 100 children were included in this study, 58 girls (58%) and 42 boys (42%). The mean age of the children was 6 years (1 year -16 years), 60% were of an average socio-economic level. The mean duration of progression was 24 months, pruritus was the most common symptom in 62% of cases. Anal localization was found in 15% of cases.
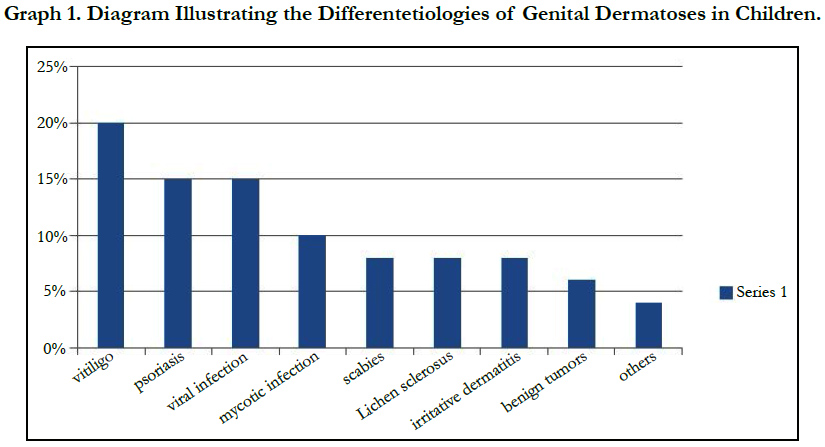
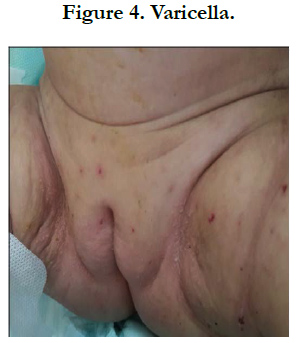
Different pathologies were found in our patients dominated by vitiligo in 20%, followed by psoriasis and viral origin in 15% of cases each, mycotic infection occupied the 3rd place with a percentage of 10%, followed by Scabies in 8%, lichen sclerosus and irritative dermatitis in 8% each. Other etiologies are found, such as benign tumors (6%), eczema, chronic inflammatory bowel diseases (CIBD) (4%). Biopsy was indicated only in 4% of patients.
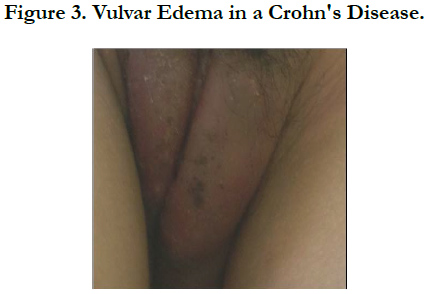
The 58 girls in our study had an average age of 6 years and complained of pruritus in 54% of cases with an average duration of 24 months. Lesions were vulvar in 25 girls. 20% of girls had genital vitiligo lesions with 50% focal genital location, and 15% had lesions of human papilloma virus (HPV). Among the 8% of girls who had sclerosus lichen, 50% had associated anal lesions. Psoriasis was present in 15% of girls. The least common diagnoses were mycotic genital lesions, benign tumors, and a case of genital localization of crohn disease.
For boys, they had an average age of 8 years and an average duration of symptoms of 20 months. Lesions were found on the scrotum in 32 boys, on the penis in 10 boys. 74% of boys had pruritus that was predominantly scabies in 17%, followed by psoriasis in 12%, followed by mycotic and HPV infections in 10% of cases. Only 8% of boys had genital vitiligo lesions.
Discussion
In children, regardless of age, all inflammatory or other dermatological diseases may have a genital location. In most cases, it is integrated into a generalized dermatosis [1, 2], and in this case, the remote elemental lesion can make the diagnosis as the case of CIBD. Childhood genital dermatoses have not been extensively treated in the literature, with almost all studies focusing on vulvar pathology, particularly infectious vulvovaginitis. Hence the interest of our study which allowed us to describe the epidemiological profile of the genital lesions seen by the dermatologist.
Through this study, it has been observed that childhood genital dermatoses are much less frequent than in adults, this is similar to that described in the literature [3]. In girls, there was a predominance of vitiligo (20%) followed by psoriasis and viral pathology in 15% of cases, followed by other etiologies such as mycotic genital lesions, lichen sclerosus, eczema, and benign tumors. This is different from what is found in the literature, especially in the study by Fischer and Rogers [4] who evaluated 130 girls. Of these patients, 41 (33%) had irritative dermatitis, 23 (18%) had lichen sclerosus, 21 (17%) had psoriasis, 15 (12%) had benign vulvar tumors and 13 had streptococcal vulvovaginitis. In an Indian study (5), the most frequent non-venereal dermatosis in prepubertal girls (21 cases) was vitiligo in 57.1% of the cases, followed by lichen sclerosus in 14.3% and psoriasis in 9.5% of cases.
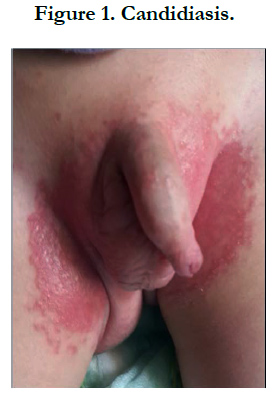
It is important to note that vulvo-vaginal candidiasis, which is a significant part of vulvar disease in adults [6], has not been recorded in girls in our series as well as in the Fisher series and Rogers [3] and in the Indian series [5]. This may be explained by the fact that the majority of children with genital symptoms are seen initially by Pediatric physicians or general practitioners, and in most cases are treated as mycotic infections, and it is only in the face of persistence Of the symptomatology they consult dermatologists for a more specialized opinion. On the other hand, candidiasis is oestrogen dependent.
The presence of genital warts in children, raises the possibility of sexual abuse of children [7, 8]. There is a female preponderance as was the case in our study. Sclero-atrophic lichen is rare in children, but its exact frequency is difficult to define, the diagnosis age is around 7 years but there is a significant diagnostic delay [9]. In our study it presented 8% of cases, all of them female and pruritus was the main reason for consultation.
Finally, Ano-vulvar localizations of systemic diseases are rarely revealing and isolated in children: Behçet's disease [10] and Crohn's disease [11, 12], the diagnosis of which is difficult at the beginning when it exists an edema isolated from a large lip, before inguinal fissures appear in rhagades, and anal fissures. This condition can remain for a long time exclusive vulvar, without digestive manifestations, and several biopsies may be necessary to confirm the diagnosis.
References
- D Teillac-hamel (1992) Pathologie ano-vulvaire de I' enfant. J de pediatrie et de puericulture. 5(7): 448.
- D Hamel- teillac (2004) Localisations vulvo-vaginales des dermatoses inflammatoires chez l’enfant. Ann Dermatol Venereol. 131(10): 907-11.
- Fischer G, Rogers M (1997) Paediatricvulvovaginitis. In: Proceedings of 3rd symposium on diseases of the vulva and vagina. Melbourne, Australia: Melbourne University, 26–29.
- Fischer G, Rogers M (2000) Vulvar diseases in children: A clinical audit of 130 cases. Pediatr Dermatol. 17(1): 1-6.
- Singh N, Thappa DM, Jaisankar TJ, Habeebullah S (2008) Pattern of nonvenereal dermatoses of female external genitalia in South India. Dermatol Online J. 14(1): 1.
- Fischer GO (1996) The commonest causes of symptomatic vulvar disease: a dermatologist’s perspective. Australas J Dermatol. 37(1): 12–18.
- Boyd AS (1990) Condylomata acuminata in the pediatric population. Am J Dis Child. 144(7): 817-24.
- Stalder JF, Heloury Y, David A, Litoux P (1989) Anogential Condyloma in children and sexual Abuse. Practical management. Ann Dermatol Venereol. 116(3) : 265-8.
- Pelisse M, Fischesser D, Moyal M, Hewitt J, Enjolras O, et al., (1984) Pediatric vulvar lichen sclerosus. Ann Dermatol Venereol. 11(8) : 741-2.
- Rakover Y, Adar H, Tal I, Lang Y, Kedar A (1989) Behcet disease : long term follow up of three children and review of the literature. Pediatrics. 83(6): 986-92.
- Hewitt J, Pelisse M, Paniel B (1987) Maladies de la vulve. Medsi/Mac Graw Hill : Paris. 41-8.
- Mezoff AG, Cohen MR, Matsel SK, Farell MK (1990) Crohn disease in an infant with central nervous system thrombosis and protein-losing enteropathy. J Ped. 117(3): 436-439.